LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does tirzepatide help with inflammation? This question has gained attention as research explores effects beyond this medication's FDA-approved uses for type 2 diabetes and weight management. Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist that improves glycemic control and promotes weight loss. Emerging evidence suggests it may reduce inflammatory markers like high-sensitivity C-reactive protein (hsCRP), though whether this represents direct anti-inflammatory action or secondary benefits from metabolic improvements remains under investigation. Understanding tirzepatide's potential effects on inflammation helps patients and clinicians make informed treatment decisions.
Quick Answer: Tirzepatide may reduce inflammatory markers like high-sensitivity C-reactive protein, though it is unclear whether this represents direct anti-inflammatory effects or secondary benefits from weight loss and improved glycemic control.
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus (brand name Mounjaro) and chronic weight management (brand name Zepbound) in adults with a BMI ≥30 kg/m² or ≥27 kg/m² with at least one weight-related comorbidity. As a dual agonist, tirzepatide activates both GIP and GLP-1 receptors, which are incretin hormones that play crucial roles in glucose homeostasis and metabolic regulation.
The mechanism of action involves multiple pathways that contribute to glycemic control and weight reduction. Tirzepatide enhances glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriately elevated glucagon secretion, and slows gastric emptying. These effects collectively improve postprandial and fasting glucose levels in patients with type 2 diabetes. The GLP-1 receptor activation also reduces appetite and food intake through central nervous system pathways, contributing to significant weight loss observed in clinical trials.
Administered as a once-weekly subcutaneous injection, tirzepatide is available in doses ranging from 2.5 mg to 15 mg, with recommended dose escalation in 2.5 mg increments approximately every 4 weeks to minimize gastrointestinal side effects. The medication is metabolized by proteolytic cleavage and beta-oxidation, with metabolites eliminated via urine and feces. It has a half-life of approximately five days that supports weekly dosing. Clinical trials have demonstrated substantial reductions in hemoglobin A1c (up to 2.5% reduction from baseline) and body weight (up to 20% reduction from baseline) in the SURPASS and SURMOUNT clinical trial programs.
Emerging evidence suggests that tirzepatide may influence systemic inflammatory markers, though there is no FDA indication for anti-inflammatory therapy, and such use would be considered off-label. Some clinical studies have documented reductions in high-sensitivity C-reactive protein (hsCRP) among patients treated with tirzepatide for type 2 diabetes or obesity. Elevated inflammatory biomarkers are established risk factors for cardiovascular disease and are frequently increased in patients with metabolic syndrome.
In the SURPASS clinical trial program, post-hoc analyses revealed decreases in hsCRP levels among tirzepatide-treated participants compared to baseline. These analyses were exploratory and not primary endpoints of the trials. Reductions in inflammatory markers appeared to correlate with improvements in glycemic control and weight loss, though the independent contribution of tirzepatide remains under investigation. Limited data exist regarding tirzepatide's effects on other inflammatory markers such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α) in humans, with most evidence coming from preclinical studies.
Mechanistically, GLP-1 receptor agonists have demonstrated anti-inflammatory properties in preclinical models through multiple pathways. These include reduced nuclear factor-kappa B (NF-κB) activation, decreased oxidative stress, and improved endothelial function. The GIP receptor activation component of tirzepatide may provide additional effects, as GIP receptors are expressed on immune cells and adipocytes, potentially modulating inflammatory responses in these tissues. However, these mechanisms are primarily established in animal models with limited confirmation in human studies.
It remains uncertain whether tirzepatide exerts direct anti-inflammatory effects independent of its metabolic benefits. Weight loss itself substantially reduces systemic inflammation, and improved glycemic control decreases glucotoxicity-related inflammatory pathways. Distinguishing direct pharmacological anti-inflammatory actions from secondary metabolic improvements requires further mechanistic studies and randomized controlled trials specifically designed to assess inflammatory outcomes as primary endpoints. Currently, routine measurement of inflammatory markers is not recommended as part of standard tirzepatide therapy.
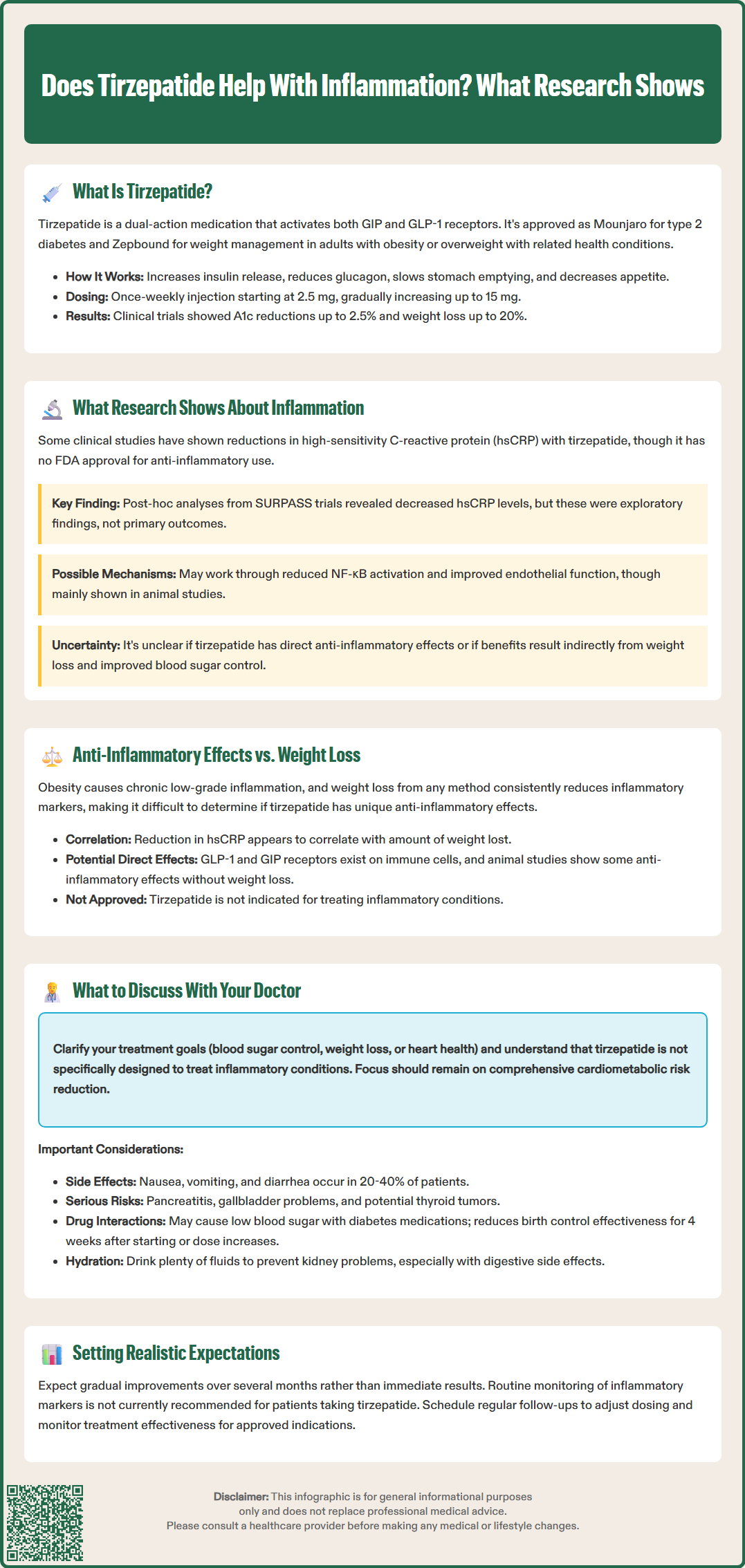
Differentiating between direct anti-inflammatory properties of tirzepatide and the indirect benefits of weight reduction presents a significant clinical and research challenge. Obesity is recognized as a chronic inflammatory state characterized by elevated circulating inflammatory cytokines, adipose tissue macrophage infiltration, and systemic low-grade inflammation. Weight loss through any intervention—whether pharmacological, surgical, or lifestyle-based—consistently reduces inflammatory markers, making it difficult to isolate drug-specific effects.
Observational evidence suggests that the magnitude of inflammatory marker reduction with tirzepatide correlates with the degree of weight loss achieved. Patients experiencing greater weight reduction typically demonstrate more substantial decreases in hsCRP. This relationship supports the hypothesis that much of tirzepatide's anti-inflammatory benefit may be mediated through weight loss rather than direct receptor-mediated anti-inflammatory signaling, though controlled studies specifically addressing this question are limited.
Some mechanistic data suggest potential direct effects. GLP-1 and GIP receptors are expressed on various immune cells, including monocytes, macrophages, and lymphocytes. Receptor activation may modulate immune cell function, cytokine production, and inflammatory signaling pathways independent of metabolic changes. Animal studies have demonstrated anti-inflammatory effects of GLP-1 receptor agonists in models where weight loss was minimal or absent, suggesting direct pharmacological actions on inflammatory pathways. However, translation of these findings to humans requires further investigation.
From a clinical perspective, it's important to note that tirzepatide is not indicated for treating inflammatory conditions. The American Diabetes Association Standards of Care does not recommend targeting inflammatory markers as treatment goals for diabetes or obesity management. Instead, the guidelines emphasize comprehensive cardiometabolic risk reduction through improved glycemic control, weight management, blood pressure control, and lipid management. Any changes in inflammatory markers with tirzepatide should be considered secondary effects rather than primary treatment targets.
If you are considering tirzepatide or currently taking this medication, several important topics warrant discussion with your healthcare provider regarding inflammation and overall treatment goals. First, clarify your treatment objectives—whether the primary focus is glycemic control, weight management, or broader cardiometabolic risk reduction. Understanding that tirzepatide is not specifically indicated for inflammatory conditions helps set appropriate expectations.
Patients with conditions characterized by chronic inflammation, such as cardiovascular disease, metabolic dysfunction-associated steatotic liver disease (MASLD, formerly NAFLD), or metabolic syndrome, should discuss how tirzepatide fits into their comprehensive management plan. Your provider can assess baseline inflammatory markers if clinically indicated and monitor changes over time, though routine inflammatory marker testing is not standard practice for tirzepatide therapy.
Important safety considerations include common adverse effects such as gastrointestinal symptoms (nausea, vomiting, diarrhea), which occur in 20-40% of patients but typically diminish with continued use. More serious but rare risks include pancreatitis (severe abdominal pain radiating to the back), gallbladder disease (right upper quadrant pain, fever, jaundice), and potential thyroid C-cell tumors (based on animal data). Tirzepatide should be used with caution in patients with severe gastrointestinal disease or gastroparesis.
Discuss medication interactions, particularly with insulin or sulfonylureas, which may require dose adjustments to prevent hypoglycemia. Women using oral contraceptives should be advised that tirzepatide may reduce contraceptive effectiveness due to delayed gastric emptying; alternative or additional contraception methods are recommended for 4 weeks after initiation and dose increases. Tirzepatide should not be used during pregnancy or breastfeeding, and women of reproductive potential should use effective contraception. Avoid using tirzepatide with other GLP-1 receptor agonists.
Maintain adequate hydration, especially if experiencing gastrointestinal side effects, to reduce the risk of acute kidney injury. Finally, establish realistic timelines for metabolic improvements, recognizing that benefits typically emerge gradually over several months of treatment. Regular follow-up appointments allow for dose optimization, adverse effect management, and assessment of treatment efficacy across multiple health parameters.
No, tirzepatide is not FDA-approved for treating inflammatory conditions. It is approved only for type 2 diabetes mellitus (Mounjaro) and chronic weight management (Zepbound), and any anti-inflammatory effects observed are considered secondary benefits.
Post-hoc analyses from clinical trials show tirzepatide may reduce high-sensitivity C-reactive protein (hsCRP) levels, though reductions appear to correlate with weight loss and improved glycemic control. Whether tirzepatide has direct anti-inflammatory effects independent of metabolic improvements requires further research.
Routine inflammatory marker testing is not recommended as part of standard tirzepatide therapy. Treatment goals focus on glycemic control, weight management, and comprehensive cardiometabolic risk reduction rather than targeting inflammatory markers.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.