LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does tirzepatide show up in urine tests? This is a common concern for patients prescribed Mounjaro or Zepbound for type 2 diabetes or weight management. Tirzepatide, a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist, is not detected by standard urine drug screening panels. These routine tests target small-molecule substances of abuse, not large peptide medications. Understanding what drug screens actually detect—and why tirzepatide isn't among them—can provide reassurance for patients undergoing employment testing, pre-operative screening, or routine clinical assessments while using this FDA-approved prescription therapy.
Quick Answer: Tirzepatide does not show up in standard urine drug tests because it is a large peptide molecule not targeted by conventional immunoassay-based screening panels.
Tirzepatide, marketed as Mounjaro and Zepbound, is not included in standard urine drug screening tests. This glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist is a large peptide molecule that is not targeted by conventional immunoassay-based urine drug screens used in employment, athletic, or routine clinical settings.
Standard urine drug tests are designed to identify specific small-molecule substances of abuse such as amphetamines, benzodiazepines, cannabinoids, cocaine, opioids, and phencyclidine. These tests rely on antibody recognition of specific drug metabolites or parent compounds. Tirzepatide, with a molecular weight exceeding 4,800 daltons, is structurally and chemically distinct from these substances and would not trigger a positive result on these panels.
Furthermore, tirzepatide is not classified as a controlled substance by the Drug Enforcement Administration (DEA). It is an FDA-approved prescription medication indicated for type 2 diabetes management and chronic weight management in adults with obesity or overweight with weight-related comorbidities. There is no regulatory or clinical rationale for including tirzepatide in routine drug screening protocols.
Patients using tirzepatide for legitimate medical purposes should not be concerned about false-positive results on employment or pre-procedural drug screens. However, specialized laboratory testing could detect tirzepatide if specifically developed and requested for research purposes, though this would typically involve serum or plasma samples rather than urine and is not part of standard clinical practice.
Urine drug screens (UDS) are immunoassay-based tests that detect specific classes of psychoactive substances and their metabolites. The standard 5-panel test screens for amphetamines, cocaine metabolites, marijuana (THC), opiates, and phencyclidine. Extended panels may include barbiturates, benzodiazepines, methadone, and synthetic opioids, but these remain focused on substances with abuse potential or regulatory significance.
The detection mechanism relies on antibody-antigen interactions. When a target drug or metabolite is present in urine above a predetermined cutoff concentration, it binds to specific antibodies in the test reagent, producing a measurable signal. These cutoff thresholds are established to minimize false positives while maintaining clinical sensitivity. For example, the federal workplace testing cutoff for marijuana metabolites is 50 ng/mL for initial screening, as defined by the Substance Abuse and Mental Health Services Administration (SAMHSA).
Importantly, urine drug screens are designed for rapid, cost-effective detection of small, lipophilic molecules that are commonly abused or have legal implications. Peptide-based medications like tirzepatide, insulin, or other biologic therapies are not included in standard panels because they require entirely different analytical methods for detection, such as liquid chromatography-mass spectrometry (LC-MS) or specialized immunoassays developed specifically for these compounds.
Cross-reactivity—where structurally similar compounds trigger false positives—is a known limitation of immunoassay testing. Common examples include pseudoephedrine causing amphetamine positives or poppy seed consumption affecting opiate results. However, tirzepatide has no known structural similarity with any substance included in standard drug panels, making false-positive results highly unlikely.
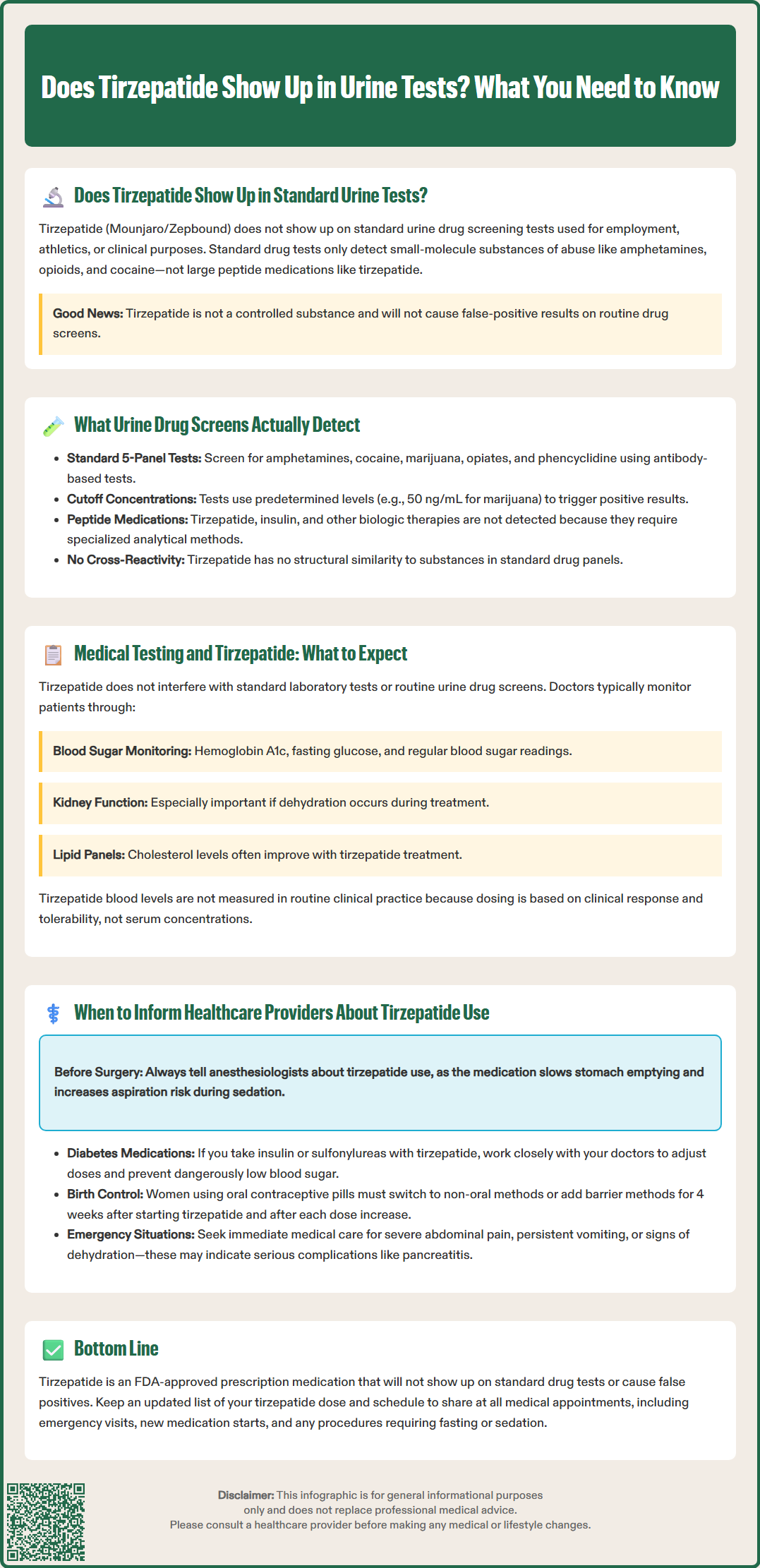
When undergoing medical testing while taking tirzepatide, patients should understand that this medication does not interfere with standard laboratory assessments. Tirzepatide is administered subcutaneously once weekly and works by activating GIP and GLP-1 receptors to enhance glucose-dependent insulin secretion, suppress glucagon release, slow gastric emptying, and reduce appetite. These mechanisms affect metabolic parameters but do not alter routine drug screening results.
Clinicians monitoring patients on tirzepatide typically assess glycemic control through hemoglobin A1c, fasting glucose, and self-monitored blood glucose readings. Renal function may be monitored, particularly if patients experience significant gastrointestinal adverse effects that could lead to dehydration. Lipid panels may show improvement with tirzepatide therapy due to weight loss and improved insulin sensitivity, as demonstrated in clinical trials.
For patients undergoing pre-operative evaluation or employment-related testing, tirzepatide use presents no complications for standard urine drug screens. However, patients should be aware of tirzepatide's effects on gastric emptying when scheduling procedures requiring anesthesia. According to 2024 American Society of Anesthesiologists (ASA) multi-society guidance, most patients can continue GLP-1 receptor agonists perioperatively, but individualized risk assessment is recommended. Those with significant gastrointestinal symptoms, in the dose-escalation phase, or with other risk factors may benefit from specific precautions.
Specialized testing for tirzepatide levels is not performed in routine clinical practice. Unlike medications requiring therapeutic drug monitoring (such as immunosuppressants or certain antibiotics), tirzepatide dosing is standardized based on clinical response and tolerability rather than serum concentrations. If measurement of tirzepatide were needed for research purposes, specialized reference laboratories would typically analyze serum or plasma samples using targeted assays, but this is not part of any standard testing panel.
Patients should proactively disclose tirzepatide use to all healthcare providers, regardless of the clinical context. While tirzepatide does not appear on drug screens, comprehensive medication reconciliation is essential for safe clinical care. This is particularly critical before surgical procedures, as tirzepatide's effect on gastric emptying may necessitate adjusting the timing of the last dose prior to anesthesia to reduce aspiration risk.
Inform prescribers and proceduralists about tirzepatide use in the following situations: before any surgical or endoscopic procedure requiring sedation or anesthesia; when starting new medications that may affect blood glucose or gastrointestinal function; during emergency department visits, especially for abdominal pain, nausea, or vomiting; and when undergoing imaging studies that require fasting preparation. According to FDA labeling, tirzepatide has not been studied in patients with a history of pancreatitis, and alternative therapies should be considered for these patients.
For patients with type 2 diabetes, coordination between endocrinologists, primary care physicians, and specialists is essential to prevent hypoglycemia when tirzepatide is combined with insulin or sulfonylureas. Dose adjustments of these concomitant medications are often necessary. Additionally, tirzepatide may affect the absorption of oral medications due to delayed gastric emptying, which is relevant for drugs with narrow therapeutic windows. Notably, the FDA label advises that women using oral contraceptives should switch to a non-oral contraceptive method or add a barrier method for 4 weeks after initiation and for 4 weeks after each dose escalation of tirzepatide.
Patients should seek immediate medical attention for severe, persistent abdominal pain (which may radiate to the back), with or without vomiting, as these could be symptoms of acute pancreatitis. Similarly, symptoms of gallbladder disease or severe vomiting leading to dehydration warrant urgent evaluation. Patients should maintain an updated medication list including tirzepatide dose and frequency, and carry this information to all medical appointments. While tirzepatide will not affect drug screening results, accurate medication disclosure supports comprehensive care, appropriate risk assessment, and optimal clinical decision-making.
No, tirzepatide will not cause a false positive on standard drug tests. It has no structural similarity to substances screened in routine urine drug panels and is not a controlled substance.
Tirzepatide will not affect employment drug screening results, so disclosure is not required for testing purposes. However, you should always inform healthcare providers about all medications you're taking for comprehensive medical care.
Specialized laboratory assays could theoretically detect tirzepatide in serum or plasma samples if specifically developed and requested, but this is not part of standard clinical practice or routine drug screening protocols.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.