LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
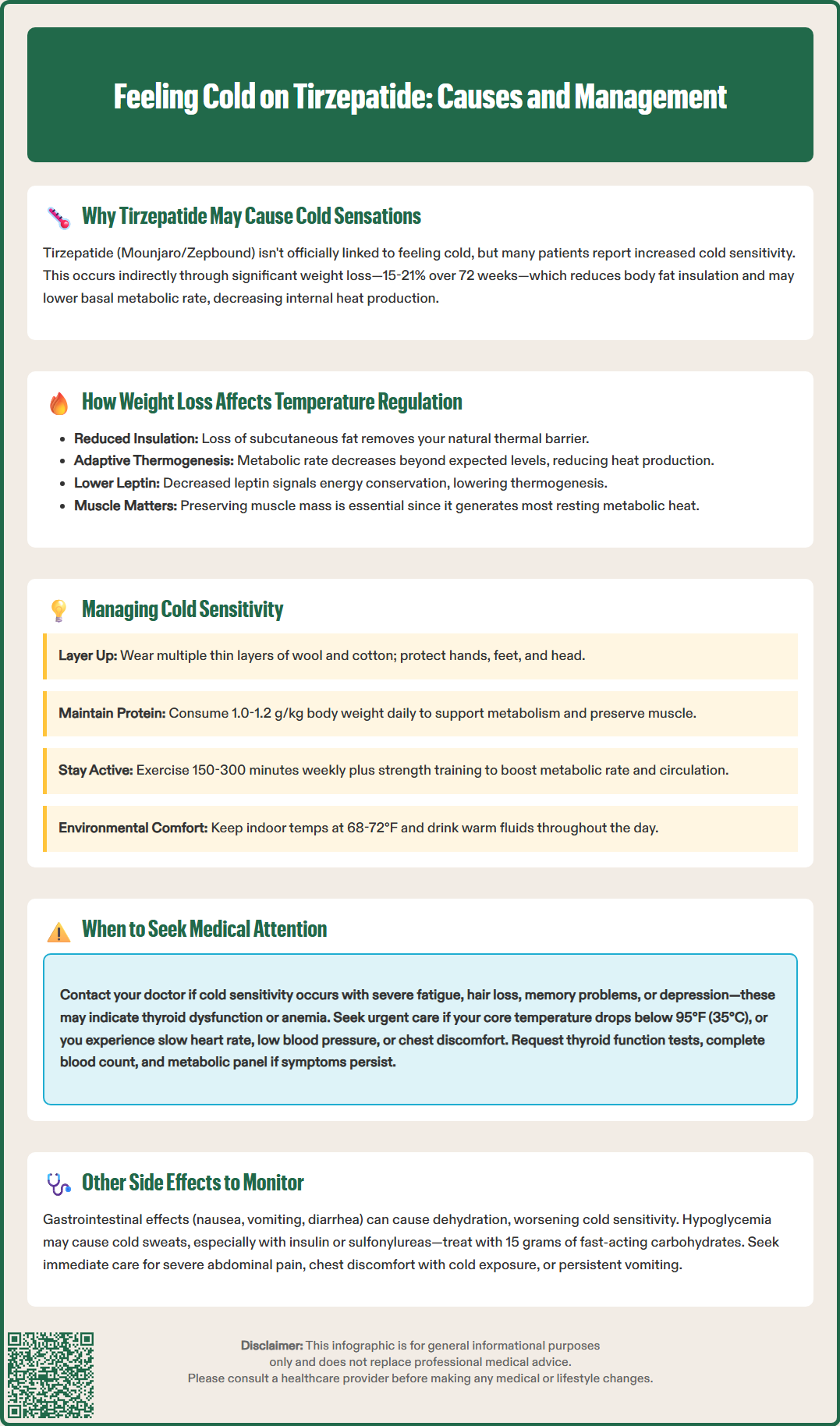
Many patients taking tirzepatide (Mounjaro, Zepbound) report feeling unusually cold during treatment. While not listed as a direct adverse effect in FDA prescribing information, this cold sensitivity appears linked to the medication's weight loss effects rather than direct temperature regulation changes. Tirzepatide is a dual GIP and GLP-1 receptor agonist approved for type 2 diabetes and chronic weight management. As patients lose significant body weight—often 15-21% over 72 weeks—reduced adipose tissue decreases natural insulation and may lower metabolic rate. Understanding why this occurs and when it requires medical attention helps patients manage this common experience while continuing effective therapy.
Quick Answer: Cold sensations on tirzepatide result from weight loss reducing body insulation and metabolic rate, not from direct drug effects on temperature regulation.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). While feeling cold is not listed as a direct adverse effect in the FDA prescribing information, some patients report increased cold sensitivity during treatment. This phenomenon appears to be an indirect consequence of the medication's primary therapeutic effects rather than a direct pharmacological action on temperature regulation.
The mechanism behind cold sensations on tirzepatide is likely multifactorial. The medication works by enhancing insulin secretion in a glucose-dependent manner, suppressing glucagon release, and slowing gastric emptying. These actions lead to reduced caloric intake and significant weight loss. Clinical trials demonstrated average weight reductions of 15-21% of body weight over 72 weeks in people with obesity (SURMOUNT-1), while more modest weight loss was observed in type 2 diabetes patients (SURPASS trials). As patients lose substantial amounts of adipose tissue, their body's natural insulation decreases, potentially making them more susceptible to environmental temperature changes.
Additionally, weight loss itself may contribute to altered temperature perception. During periods of caloric restriction and weight loss, the body may lower its basal metabolic rate as an adaptive mechanism, potentially reducing heat production. This metabolic adaptation, combined with decreased insulating fat tissue, may create the subjective experience of feeling colder than before treatment initiation.
It is important to note that there is no official link established between tirzepatide and cold intolerance as a direct drug effect. The cold sensations reported by patients are generally considered secondary to the weight loss process rather than a specific adverse reaction to the medication itself.
The human body maintains core temperature through a complex thermoregulatory system involving the hypothalamus, metabolic heat production, and insulation provided by subcutaneous fat. When significant weight loss occurs—as commonly seen with tirzepatide therapy—multiple physiological changes may affect temperature regulation. Understanding these mechanisms helps patients recognize that cold sensitivity is often a normal physiological response to body composition changes rather than a concerning medical problem.
Adipose tissue serves several thermoregulatory functions:
Insulation: Subcutaneous fat acts as a thermal barrier, reducing heat loss to the environment. As this layer diminishes with weight loss, the body loses some of its natural insulation, potentially making individuals more sensitive to ambient temperature changes.
Metabolic considerations: While adipose tissue has some metabolic activity, skeletal muscle is the primary contributor to resting metabolic rate and heat production. Preserving lean muscle mass during weight loss is crucial for maintaining metabolic rate and thermogenesis.
Hormonal regulation: Fat tissue produces leptin and other hormones that influence metabolic rate and energy expenditure. Decreased leptin levels during weight loss may signal the body to conserve energy, potentially affecting thermogenesis.
During rapid weight loss, the body may undergo metabolic adaptation—sometimes called "adaptive thermogenesis"—where energy expenditure decreases beyond what would be expected from reduced body mass alone. This adaptation may persist for varying periods after weight loss, potentially contributing to ongoing cold sensitivity. Some research suggests that individuals who have lost significant weight may experience lower metabolic rates than predicted for their new body size, though this varies considerably between individuals.
The rate of weight loss also matters. Tirzepatide typically produces gradual but substantial weight reduction over months. This timeline allows some physiological adaptation, but the magnitude of weight loss still represents a significant change in body composition that may affect temperature regulation. Many patients report that cold sensitivity improves as their weight stabilizes and the body adapts to its new composition.
While increased cold sensitivity is generally a benign consequence of weight loss, certain presentations warrant medical evaluation to exclude underlying conditions. Patients should understand the difference between expected cold sensitivity and symptoms suggesting thyroid dysfunction, anemia, or other metabolic disorders that require investigation and management.
Seek medical attention if cold intolerance is accompanied by:
Severe fatigue and weakness: Profound tiredness beyond typical adjustment to weight loss may indicate thyroid dysfunction or anemia.
Unexplained weight changes: Weight loss exceeding expected patterns or unexpected weight gain despite medication adherence.
Hair loss or brittle nails: These symptoms, combined with cold intolerance, suggest possible hypothyroidism.
Cognitive changes: Difficulty concentrating, memory problems, or depression may indicate thyroid or metabolic issues.
Low body temperature: Seek urgent medical care for core body temperature below 95°F (35°C), which indicates hypothermia. Persistent cold intolerance without hypothermia warrants discussion with your healthcare provider.
Cardiovascular symptoms: Slow heart rate, low blood pressure, or chest discomfort with cold exposure require prompt evaluation.
Hypothyroidism represents an important differential diagnosis when evaluating cold intolerance. While tirzepatide does not directly cause thyroid dysfunction, weight loss and metabolic changes can sometimes unmask subclinical thyroid disease. Thyroid function testing is recommended when symptoms suggest thyroid dysfunction. Patients experiencing significant cold intolerance should undergo thyroid function testing, complete blood count to assess for anemia (including iron studies), vitamin B12 levels (especially if taking metformin), and metabolic panel to evaluate overall health status.
Additionally, patients should report cold intolerance if it significantly impairs quality of life or daily functioning. Severe symptoms interfering with work, social activities, or sleep warrant medical discussion even if no underlying pathology is identified. Healthcare providers can assess whether dose adjustment, temporary treatment interruption, or additional supportive measures are appropriate. The goal is balancing therapeutic benefits of tirzepatide with tolerability and patient well-being.
Most patients can successfully manage cold sensitivity through practical lifestyle modifications while continuing tirzepatide therapy. These strategies address both environmental factors and physiological adaptation to support comfort without compromising treatment efficacy. A systematic approach to managing cold intolerance improves medication adherence and overall treatment satisfaction.
Environmental and clothing adjustments:
Layered clothing: Wearing multiple thin layers traps air and provides better insulation than single heavy garments. Natural fibers like wool and cotton offer superior warmth.
Temperature control: Maintaining indoor temperatures at 68-72°F (20-22°C). If using space heaters, ensure they are UL-listed, placed away from flammable materials, and equipped with automatic shut-off features for safety.
Extremity protection: Hands and feet lose heat rapidly; wearing warm socks, gloves, and hats significantly improves comfort.
Warm beverages: Drinking warm (not hot) fluids throughout the day can provide comfort, though their effect on core temperature is modest.
Nutritional considerations are equally important. While tirzepatide reduces appetite, maintaining adequate caloric intake supports metabolic function. Patients should work with healthcare providers or registered dietitians to ensure nutritional adequacy during weight loss. Protein intake deserves particular attention—adequate protein (1.0-1.2 g/kg body weight daily during active weight loss) supports lean muscle mass preservation, which contributes to metabolic heat production. Iron-rich foods help prevent anemia, which can exacerbate cold sensitivity.
Physical activity plays a dual role in managing cold intolerance. Regular exercise increases metabolic rate, generates body heat, and helps preserve lean muscle mass during weight loss. The U.S. Physical Activity Guidelines recommend at least 150-300 minutes of moderate-intensity aerobic activity weekly, plus muscle-strengthening activities at least twice weekly. Exercise also improves circulation, helping distribute warmth throughout the body.
Patients should avoid extreme temperature exposure during the adjustment period. Gradual cold exposure may help the body adapt, but sudden exposure to very cold environments can be uncomfortable. If cold sensitivity persists beyond six months of stable weight or significantly impairs quality of life, discussing dose adjustment or alternative treatment strategies with healthcare providers is appropriate. Some patients find that cold sensitivity improves once weight stabilizes, as the body adapts to its new composition.
Temperature regulation changes during tirzepatide therapy may coincide with or exacerbate other medication-related side effects. Understanding these potential interactions helps patients and healthcare providers develop comprehensive management strategies. The most common adverse effects of tirzepatide include gastrointestinal symptoms, which occur in a dose-dependent manner and may interact with thermoregulatory changes.
Gastrointestinal effects represent the most frequent adverse reactions to tirzepatide. According to FDA prescribing information, these include nausea (12-24%), diarrhea (7-23%), decreased appetite (10-19%), vomiting (2-11%), constipation (5-17%), and dyspepsia (5-9%), with rates varying by dose and indication. These symptoms typically emerge during dose escalation and often improve over time. Dehydration from gastrointestinal symptoms can worsen cold sensitivity, as adequate hydration is essential for proper circulation and temperature regulation. Patients experiencing persistent nausea or vomiting should maintain fluid intake and contact healthcare providers if unable to tolerate oral fluids.
Hypoglycemia risk increases when tirzepatide is combined with insulin or sulfonylureas, though the medication alone rarely causes low blood sugar due to its glucose-dependent mechanism. Hypoglycemia can present with cold sweats, chills, and shivering—symptoms that may be confused with general cold intolerance. The American Diabetes Association recommends that patients monitor blood glucose as directed and recognize hypoglycemia symptoms: trembling, sweating, rapid heartbeat, confusion, and hunger. Treatment involves consuming 15 grams of fast-acting carbohydrates and rechecking glucose after 15 minutes.
Cardiovascular considerations include a small mean increase in heart rate (1-4 beats per minute) noted in clinical trials. While this effect is generally mild, patients with pre-existing cardiovascular conditions should be monitored. Cold exposure can stress the cardiovascular system, particularly in individuals with coronary artery disease. Patients experiencing chest discomfort, palpitations, or shortness of breath—especially with cold exposure—should seek immediate medical evaluation.
Injection site reactions (redness, itching, or swelling) occur in approximately 0.1-1.7% of patients according to prescribing information. Cold ambient temperatures may increase injection discomfort. Allowing the medication to reach room temperature before injection and rotating injection sites reduces local reactions. Patients should never apply heat to injection sites, as this may alter medication absorption.
Rare but serious adverse effects requiring immediate medical attention include pancreatitis (severe abdominal pain radiating to the back), gallbladder disease, and acute kidney injury. The FDA prescribing information includes a boxed warning regarding thyroid C-cell tumors observed in animal studies, though human relevance remains uncertain. Patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 should not use tirzepatide.
Cold sensitivity is not listed as a direct adverse effect in FDA prescribing information, but patients commonly report it as an indirect consequence of significant weight loss. The sensation results from decreased adipose tissue insulation and potential metabolic rate reduction rather than direct drug action on temperature regulation.
Seek medical attention if cold intolerance occurs with severe fatigue, hair loss, cognitive changes, unexplained weight changes, slow heart rate, or body temperature below 95°F. These symptoms may indicate thyroid dysfunction, anemia, or other conditions requiring evaluation and treatment.
Wear layered clothing, maintain indoor temperatures at 68-72°F, protect extremities with warm socks and gloves, ensure adequate protein intake (1.0-1.2 g/kg daily), stay hydrated, and engage in regular physical activity. Most patients find cold sensitivity improves as weight stabilizes and the body adapts to new body composition.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.