LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Understanding what to eat on semaglutide is essential for maximizing treatment benefits while minimizing side effects. Semaglutide, a GLP-1 receptor agonist approved by the FDA for type 2 diabetes and chronic weight management, significantly affects appetite and digestion by slowing gastric emptying and reducing hunger signals. These effects mean that dietary choices become particularly important—every meal should provide optimal nutrition within a reduced food intake. This guide provides evidence-based recommendations on food selection, meal planning, and managing common gastrointestinal symptoms to help you achieve the best outcomes during semaglutide therapy.
Quick Answer: Patients taking semaglutide should prioritize lean proteins, non-starchy vegetables, and complex carbohydrates in smaller, frequent meals while limiting high-fat, fried, and ultra-processed foods to minimize gastrointestinal side effects and optimize treatment outcomes.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (under brand names Ozempic and Rybelsus) and chronic weight management (Wegovy). Understanding how this medication affects your gastrointestinal system is essential for optimizing your dietary approach during treatment.
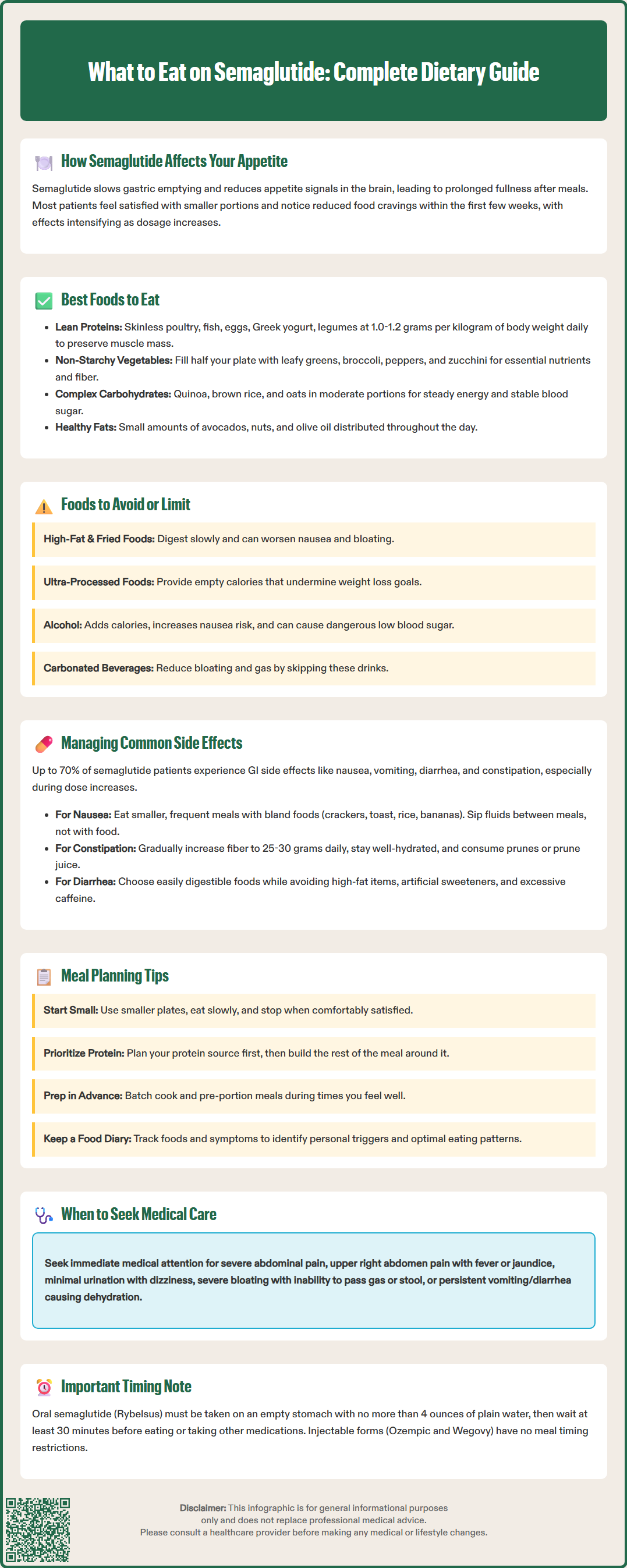
The medication works by mimicking the natural GLP-1 hormone, which plays multiple roles in glucose regulation and appetite control. Semaglutide slows gastric emptying—the rate at which food moves from your stomach into your small intestine. This delayed emptying creates a prolonged sensation of fullness after meals, which contributes significantly to reduced caloric intake. Additionally, semaglutide acts on appetite centers in the brain, particularly the hypothalamus, to decrease hunger signals and food cravings.
These pharmacological effects have important implications for your eating patterns. Many patients report feeling satisfied with smaller portion sizes and experiencing reduced interest in food between meals. The slowed digestion means food remains in your stomach longer, which can be beneficial for weight management but may also contribute to gastrointestinal side effects if dietary choices are not optimized.
Clinically, patients typically notice these appetite changes within the first few weeks of treatment, with effects becoming more pronounced as the dose is titrated upward according to FDA-approved protocols. The magnitude of appetite suppression varies among individuals, but understanding these mechanisms helps explain why dietary modifications are often helpful during semaglutide therapy.
Importantly, semaglutide is not recommended for patients with severe gastrointestinal disease or gastroparesis. If you have significant pre-existing GI symptoms, discuss these with your healthcare provider. Note that oral semaglutide (Rybelsus) has specific meal-timing requirements that differ from injectable forms, which we'll cover in a later section.
Optimizing your diet while taking semaglutide requires focusing on nutrient-dense foods that support your health goals while minimizing gastrointestinal discomfort. Because the medication reduces your overall food intake, every bite should contribute meaningful nutritional value.
Lean proteins should form the foundation of your meals. Prioritize options such as skinless poultry, fish (particularly fatty fish like salmon for omega-3 fatty acids), eggs, low-fat Greek yogurt, and plant-based proteins like legumes and tofu. Adequate protein intake—typically 1.0 to 1.2 grams per kilogram of body weight daily during weight loss, or as recommended by your healthcare provider—helps preserve lean muscle mass during weight loss and promotes satiety. If you have kidney disease, your protein needs may differ, so consult your healthcare provider.
Non-starchy vegetables are excellent choices because they provide essential vitamins, minerals, and fiber while being low in calories. Focus on leafy greens, broccoli, cauliflower, bell peppers, zucchini, and tomatoes. These foods add volume to meals without overwhelming your reduced stomach capacity.
Complex carbohydrates in moderate portions support sustained energy levels. Choose whole grains like quinoa, brown rice, oats, and whole wheat products. These provide fiber that aids digestion and helps maintain stable blood glucose levels—particularly important for patients using semaglutide for diabetes management.
Healthy fats in controlled amounts are important for nutrient absorption and satiety. Include sources like avocados, nuts, seeds, and olive oil, but be mindful of portions since fats are calorie-dense. Small amounts distributed throughout the day are generally better tolerated than large quantities in a single meal, given the delayed gastric emptying associated with semaglutide therapy.
The American Diabetes Association's Diabetes Plate Method offers a simple visual guide for meal planning: fill half your plate with non-starchy vegetables, a quarter with lean protein, and a quarter with carbohydrates, plus a small amount of healthy fat. Aim for 25-30 grams of fiber daily (about 14g per 1,000 calories), increasing intake gradually to minimize GI discomfort.
Certain foods can exacerbate the gastrointestinal side effects of semaglutide or work against your treatment goals. Understanding which foods to limit or avoid helps optimize both your comfort and therapeutic outcomes.
High-fat and fried foods are particularly problematic for patients taking semaglutide. Because the medication slows gastric emptying, fatty foods that naturally take longer to digest can remain in your stomach for extended periods, increasing the risk of nausea, bloating, and discomfort. Limit fried foods, heavy cream sauces, fatty cuts of meat, and full-fat dairy products, especially during the initial titration phase when side effects are most common.
Ultra-processed foods and added sugars should be minimized. These items provide minimal nutritional value while contributing excess calories that can undermine weight management goals. Sugary beverages, candy, pastries, and highly processed snacks can also cause rapid blood glucose fluctuations, which is counterproductive for patients using semaglutide for diabetes management.
High-fiber foods in large quantities may seem counterintuitive to limit, but excessive fiber intake—particularly when increased suddenly—can worsen gastrointestinal symptoms. While fiber is important, introduce high-fiber foods gradually and distribute fiber intake throughout the day rather than consuming large portions of beans, cruciferous vegetables, or bran products in single meals.
Alcohol warrants caution for several reasons. Beyond its caloric content and potential to impair judgment around food choices, alcohol can irritate the gastrointestinal tract and may increase nausea in patients taking semaglutide. Heavy alcohol use may also increase the risk of pancreatitis. If you take semaglutide with insulin or sulfonylureas, alcohol can increase your risk of hypoglycemia. If you choose to drink, do so in moderation and preferably with food, and monitor your blood glucose more frequently if you have diabetes.
Carbonated beverages may increase bloating and discomfort due to the gas they introduce into an already slower-emptying stomach. Many patients find that switching to still water or herbal teas improves their comfort level during treatment.
Keep track of your personal food triggers. Many patients find that very spicy foods, greasy items, or very large meals can worsen symptoms, particularly during dose titration periods.
Gastrointestinal side effects are common with semaglutide therapy. Depending on the dose and indication, up to 70% of patients may experience some GI effects, with higher rates typically seen at weight management doses (2.4 mg) and during dose escalation. Nausea, vomiting, diarrhea, constipation, and abdominal discomfort can often be managed effectively through strategic dietary modifications.
For nausea management, several dietary approaches have proven helpful in clinical practice. Eat smaller, more frequent meals rather than three large meals daily—this approach works with the medication's effect on gastric emptying rather than against it. Choose bland, easily digestible foods when nausea is present, such as crackers, toast, rice, bananas, and applesauce. Avoid lying down immediately after eating, as this can worsen nausea. Ginger, either as tea or in small amounts in food, may provide natural relief for some patients. Stay well-hydrated, but sip fluids slowly between meals rather than drinking large amounts with food, which can increase stomach fullness and discomfort.
Constipation, another common side effect, responds well to dietary intervention. Gradually increase your fiber intake through fruits, vegetables, and whole grains, aiming for 25-30 grams daily. Ensure adequate hydration by drinking enough fluids to keep your urine pale yellow. Prunes and prune juice have natural laxative properties that many patients find helpful. Regular physical activity also supports healthy bowel function.
For diarrhea, focus on easily digestible foods and avoid high-fat items, artificial sweeteners (particularly sugar alcohols), and excessive caffeine. The BRAT diet (bananas, rice, applesauce, toast) can be helpful during acute episodes, though it should not be followed long-term due to nutritional limitations.
If you take semaglutide with insulin or sulfonylureas, be aware of increased hypoglycemia risk. Work with your healthcare provider to adjust these medications as needed. If you experience hypoglycemia, follow the 15-15 rule: consume 15 grams of fast-acting carbohydrate, wait 15 minutes, and recheck your blood glucose.
IMPORTANT SAFETY INFORMATION: Contact your healthcare provider immediately if you experience:
Severe, persistent abdominal pain, with or without vomiting (possible pancreatitis)
Pain in the upper right abdomen, fever, or yellowing of skin/eyes (possible gallbladder problems)
Minimal urination, dizziness, or extreme thirst (possible kidney problems)
Severe abdominal distention or inability to pass gas or stool (possible intestinal obstruction)
Persistent vomiting or diarrhea can lead to dehydration and electrolyte imbalances requiring medical attention. Consider keeping oral rehydration solutions on hand.
Successful long-term outcomes with semaglutide therapy often depend on establishing sustainable eating patterns that align with the medication's effects. Strategic meal planning helps ensure adequate nutrition while minimizing side effects and supporting your health goals.
Start with smaller portions and adjust based on your individual tolerance. Many patients find they need less food to feel satisfied while taking semaglutide. Use smaller plates to make reduced portions appear more satisfying visually. Plan to eat slowly and mindfully, putting down utensils between bites and stopping when you feel comfortably satisfied rather than full.
Prioritize protein at each meal to meet your daily requirements despite reduced overall food intake. A practical approach is to plan your protein source first, then build the rest of your meal around it. For example, a breakfast might center on eggs or Greek yogurt, lunch around grilled chicken or fish, and dinner around lean meat or plant-based protein.
Prepare meals in advance when you feel well, as this ensures you have appropriate options available during times when nausea or fatigue might otherwise lead to poor food choices. Batch cooking proteins, pre-cutting vegetables, and portioning snacks can significantly reduce daily decision-making and preparation burden.
Time your largest meal strategically. Many patients tolerate food better earlier in the day, so consider making breakfast or lunch your main meal if evening nausea is problematic. However, individual responses vary—track your symptoms and adjust accordingly.
Keep a food and symptom diary during the initial months of treatment. Record what you eat, portion sizes, timing, and any symptoms experienced. This information helps identify personal triggers and optimal eating patterns, and provides valuable data to share with your healthcare provider during follow-up appointments.
Plan for adequate hydration throughout the day. Set reminders if needed, and keep water readily accessible. Adequate fluid intake helps prevent dehydration and may help manage some side effects.
Important medication-specific instructions:
If taking oral semaglutide (Rybelsus): Take once daily on an empty stomach with no more than 4 ounces of plain water. Wait at least 30 minutes before eating, drinking anything else, or taking other oral medications. Swallow tablets whole; do not cut, crush, or chew.
Injectable semaglutide (Ozempic, Wegovy) does not have specific meal timing requirements.
Before procedures or surgery, inform your surgical and anesthesia teams about your semaglutide use due to its effects on gastric emptying and potential aspiration risk.
Consider working with a registered dietitian who has experience with patients taking GLP-1 receptor agonists. Professional guidance can help ensure you meet nutritional requirements while managing side effects and achieving your therapeutic goals safely and effectively.
Avoid or limit high-fat and fried foods, ultra-processed foods, added sugars, and excessive alcohol, as these can worsen gastrointestinal side effects like nausea and bloating. Carbonated beverages may also increase discomfort due to semaglutide's effect on gastric emptying.
Aim for 1.0 to 1.2 grams of protein per kilogram of body weight daily to preserve lean muscle mass during weight loss. Focus on lean sources like skinless poultry, fish, eggs, low-fat Greek yogurt, and plant-based proteins at each meal.
Injectable semaglutide (Ozempic, Wegovy) has no specific meal timing requirements. However, oral semaglutide (Rybelsus) must be taken on an empty stomach with no more than 4 ounces of plain water, and you must wait at least 30 minutes before eating or drinking anything else.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.