LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

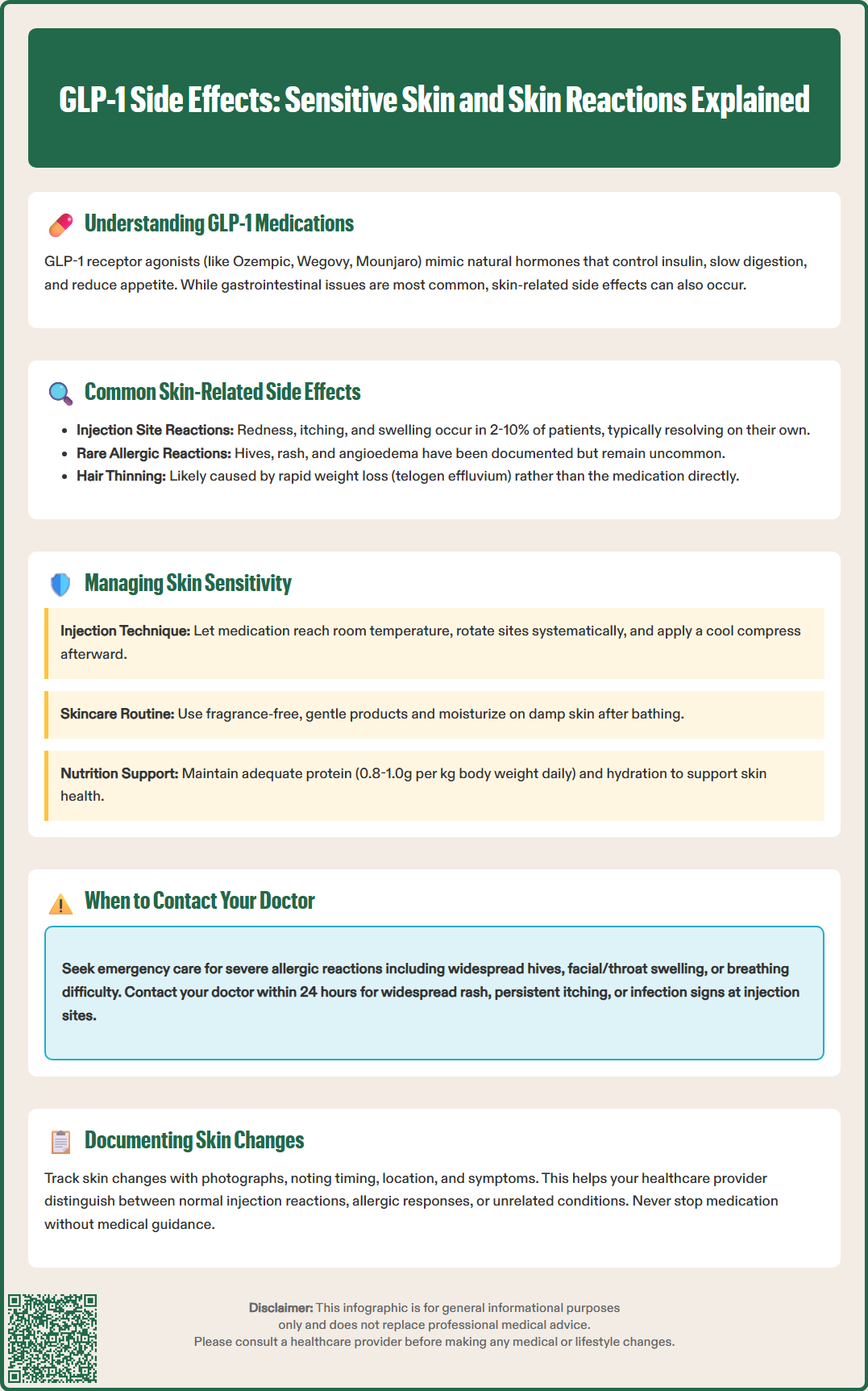
GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound) are widely prescribed for type 2 diabetes and weight management. While gastrointestinal side effects are well-documented, some patients report skin-related concerns, including sensitive skin. Understanding the relationship between GLP-1 medications and skin reactions helps patients distinguish between documented adverse effects, injection site reactions, and changes related to weight loss. This article examines the evidence for GLP-1 side effects on sensitive skin, reviews recognized dermatological reactions, and provides guidance on managing skin symptoms during treatment.
Quick Answer: GLP-1 receptor agonists are not officially linked to generalized sensitive skin, though injection site reactions occur in 2-10% of patients and rare allergic skin reactions have been reported.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists represent a class of medications increasingly prescribed for type 2 diabetes management and, more recently, for chronic weight management. These medications include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda). Tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 receptor agonist with similar effects. These medications work by mimicking the action of naturally occurring incretin hormones, which stimulate insulin secretion in response to food intake, suppress glucagon release, slow gastric emptying, and promote satiety through central nervous system pathways.
The most commonly reported side effects of these medications are gastrointestinal in nature. According to FDA prescribing information, these include nausea, vomiting, diarrhea, constipation, and abdominal pain. These effects typically occur during dose initiation or escalation and often diminish over time as the body adjusts to the medication. The gastrointestinal side effects result directly from the drug's mechanism of slowing gastric emptying and affecting gut motility.
Beyond gastrointestinal symptoms, other documented adverse effects include injection site reactions, fatigue, headache, and dizziness. More serious but less common risks include pancreatitis (characterized by severe abdominal pain that may radiate to the back), gallbladder disease, and acute kidney injury from volume depletion. These medications carry a boxed warning about thyroid C-cell tumors observed in rodent studies and are contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Hypoglycemia can occur, particularly when these medications are combined with insulin or sulfonylureas. Understanding this established side effect profile provides important context when patients report symptoms that fall outside typical patterns, such as skin-related concerns.
The relationship between GLP-1 receptor agonists and generalized skin sensitivity remains unclear, as there is no official established link between these medications and widespread sensitive skin as a direct pharmacological effect. FDA prescribing information for GLP-1 medications does not list generalized skin sensitivity or heightened skin reactivity as recognized adverse effects. However, specific dermatological reactions have been documented in clinical trials and post-marketing surveillance.
Injection site reactions are the most commonly reported skin-related side effects of GLP-1 medications. These localized reactions may include redness, itching, swelling, bruising, or discomfort at the injection site. According to FDA prescribing information, injection site reactions occur in approximately 2-10% of patients, varying by specific product. These reactions are typically mild, self-limiting, and resolve without intervention.
Rare cases of allergic skin reactions have been reported with GLP-1 use, including urticaria (hives), rash, and pruritus (itching). Angioedema, a potentially serious allergic reaction involving deeper tissue swelling, has been documented in post-marketing reports, though it remains uncommon. These are considered hypersensitivity reactions per product labeling.
Some patients using GLP-1 medications for weight management have reported hair thinning or alopecia, particularly with semaglutide (Wegovy) and tirzepatide (Zepbound). This is likely associated with rapid weight loss rather than a direct medication effect, representing a condition called telogen effluvium.
It is important to distinguish between documented adverse effects and anecdotal patient experiences. Some individuals taking GLP-1 medications report subjective changes in skin texture, increased dryness, or heightened sensitivity to skincare products. These reports may reflect individual variation, concurrent factors such as rapid weight loss (which can affect skin integrity), nutritional changes, or coincidental dermatological conditions rather than a direct drug effect.
Patients taking GLP-1 receptor agonists should be aware of both common and concerning skin manifestations that may occur during treatment. Injection site reactions are the most frequent skin-related finding and typically present as localized redness, mild swelling, or tenderness at the injection site. These reactions usually appear within hours of injection and resolve within a few days. Rotating injection sites among recommended areas (abdomen, thigh, upper arm), cleansing the skin before injection, and avoiding areas with visible blood vessels, inflammation, infection, or scarring can help minimize these reactions.
Allergic skin reactions require more careful attention. Signs of a potential allergic response include:
Widespread rash or hives appearing beyond the injection site
Intense itching affecting multiple body areas
Swelling of the face, lips, tongue, or throat (angioedema)
Skin reactions accompanied by difficulty breathing or swallowing
These symptoms may indicate hypersensitivity and warrant prompt medical evaluation. If anaphylaxis or angioedema occurs, the medication should be discontinued permanently and not restarted.
Some patients report skin changes associated with rapid weight loss, which is a therapeutic effect of GLP-1 medications used for weight management. Significant weight reduction can lead to decreased skin elasticity, increased skin laxity, dryness, and subjective changes in skin texture. Hair thinning or shedding may also occur with rapid weight loss. While not direct drug side effects, these changes occur in the context of treatment and may be perceived as medication-related.
Nutritional factors resulting from reduced food intake or altered eating patterns may also manifest with skin symptoms. Adequate protein intake supports skin integrity, while vitamins A, C, E, and essential fatty acids contribute to skin health. Patients experiencing persistent skin dryness, unusual texture changes, or delayed wound healing should discuss nutritional assessment with their healthcare provider, though a direct causal relationship between GLP-1 therapy and specific nutritional deficiencies has not been firmly established.
For patients experiencing injection site reactions, several practical strategies can minimize discomfort. Follow your medication's specific storage instructions; if refrigerated, allow the medication to reach room temperature before injection as permitted by the product label. Ensure proper injection technique, inserting the needle at the correct angle and avoiding areas with visible blood vessels, scars, or previous injection sites. Systematic rotation of injection sites prevents repeated trauma to the same area. Applying a cool compress after injection may reduce mild swelling or discomfort, though avoid applying ice directly to skin.
If generalized skin dryness or sensitivity develops during treatment, optimize skincare practices with gentle, fragrance-free cleansers and moisturizers. Avoid harsh exfoliants, alcohol-based products, or heavily fragranced cosmetics that may irritate sensitive skin. Apply moisturizer to damp skin after bathing to enhance hydration retention. Consider using a humidifier in dry environments, particularly during winter months.
Nutritional optimization is essential for maintaining skin health, especially when significant weight loss occurs. Ensure adequate protein intake (generally 0.8-1.0 grams per kilogram of body weight daily per US Dietary Guidelines, though patients with chronic kidney disease should follow their healthcare provider's specific recommendations). Maintain hydration with adequate fluid intake. Consider discussing your overall nutrition with your doctor or a registered dietitian if dietary intake of essential nutrients is compromised by reduced appetite or food volume.
For persistent or bothersome injection site reactions, discuss alternative injection techniques or sites with your healthcare provider. In some cases, switching to a different medication formulation may be appropriate if reactions are related to specific excipients. However, never discontinue or modify your medication regimen without medical guidance.
Document any skin changes with photographs and notes about timing, location, and associated symptoms. This information helps your healthcare provider assess whether symptoms represent expected injection site reactions, allergic responses, or unrelated dermatological conditions requiring separate evaluation. For persistent, unexplained, or worsening skin conditions, a dermatology referral may be appropriate.
Certain skin-related symptoms during GLP-1 treatment require prompt medical attention. Call 911 or seek immediate emergency care if you experience signs of a severe allergic reaction, including widespread hives, facial or throat swelling, difficulty breathing or swallowing, rapid heartbeat, or dizziness. These symptoms may indicate anaphylaxis, a medical emergency requiring urgent intervention. If you experience anaphylaxis or angioedema, the medication should be permanently discontinued and not restarted.
Contact your healthcare provider within 24 hours if you develop a widespread rash, persistent itching affecting multiple body areas, or skin reactions accompanied by fever, joint pain, or general malaise. These findings may suggest a systemic hypersensitivity reaction or other condition requiring evaluation. Similarly, if injection site reactions become progressively worse rather than improving, show signs of infection (increasing warmth, spreading redness, pus, or red streaking), or fail to resolve within several days, medical assessment is warranted.
Schedule a routine appointment to discuss skin changes that are persistent but not urgent, such as ongoing skin dryness unresponsive to moisturizers, changes in skin texture or elasticity concerning to you, or new skin lesions unrelated to injection sites. These symptoms may benefit from dermatological evaluation or nutritional assessment. Additionally, if you notice delayed wound healing, hair thinning, or easy bruising developing after starting therapy, discuss these findings with your provider, as they may indicate nutritional factors or other issues requiring attention.
Before your appointment, prepare a clear description of your symptoms, including when they started in relation to beginning therapy or dose changes, their location and appearance, any factors that worsen or improve them, and any over-the-counter treatments you have tried. Bring photographs if possible, as skin findings may not be present during your visit. This information enables your healthcare provider to determine whether symptoms represent expected medication effects, require symptomatic management, or necessitate further investigation or treatment modification.
GLP-1 receptor agonists are not officially linked to generalized sensitive skin according to FDA prescribing information. However, injection site reactions occur in 2-10% of patients, and rare allergic skin reactions including rash, hives, and itching have been documented.
Injection site reactions are the most common skin-related side effects, presenting as localized redness, swelling, bruising, or itching at the injection site. These reactions are typically mild, self-limiting, and resolve within a few days.
Seek immediate emergency care for signs of severe allergic reaction including facial swelling, difficulty breathing, or widespread hives. Contact your healthcare provider within 24 hours for widespread rash, persistent itching, or injection site reactions showing signs of infection or worsening rather than improving.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.