LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Semaglutide has emerged as a transformative medication for managing type 2 diabetes and chronic weight management, but determining who is a good candidate for semaglutide requires careful clinical evaluation. This glucagon-like peptide-1 receptor agonist, available as Ozempic, Wegovy, and Rybelsus, offers significant benefits for specific patient populations when prescribed appropriately. Understanding eligibility criteria, contraindications, and FDA-approved indications helps patients and healthcare providers make informed decisions about whether semaglutide therapy aligns with individual health goals and medical circumstances. This comprehensive guide examines the clinical factors that define appropriate candidacy for semaglutide treatment.
Quick Answer: Good candidates for semaglutide include adults with type 2 diabetes requiring improved glycemic control, adults with obesity (BMI ≥30) or overweight (BMI ≥27) with weight-related comorbidities, and patients committed to long-term lifestyle modifications alongside medication therapy.
Semaglutide is a glucagon-like peptide-1 receptor agonist (GLP-1 RA) approved by the US Food and Drug Administration for the treatment of type 2 diabetes mellitus and chronic weight management. Available under brand names including Ozempic, Wegovy, and Rybelsus, semaglutide represents a significant advancement in metabolic disease management. The medication is administered either as a once-weekly subcutaneous injection or as a daily oral tablet, depending on the formulation and indication.
The mechanism of action of semaglutide mimics the naturally occurring incretin hormone GLP-1, which plays a crucial role in glucose homeostasis and appetite regulation. When administered, semaglutide binds to GLP-1 receptors in pancreatic beta cells, stimulating glucose-dependent insulin secretion. This means insulin release occurs primarily when blood glucose levels are elevated, reducing the risk of hypoglycemia compared to some other diabetes medications. Simultaneously, semaglutide suppresses glucagon secretion from pancreatic alpha cells, further contributing to improved glycemic control.
Beyond its effects on pancreatic function, semaglutide acts on GLP-1 receptors in the central nervous system, particularly in areas regulating appetite and satiety. This action delays gastric emptying and promotes feelings of fullness, leading to reduced caloric intake. Clinical trials have demonstrated that semaglutide produces reductions in hemoglobin A1c levels in patients with type 2 diabetes, typically ranging from 1.0% to 1.8%, depending on the dose and patient population. For weight management, patients receiving the higher 2.4 mg dose (Wegovy) often experience significant weight loss, with average reductions of 10-15% of body weight in obesity treatment trials, while lower doses used for diabetes typically produce more modest weight loss. This dual effect makes semaglutide a valuable therapeutic option for metabolic health.
The FDA has approved semaglutide for distinct but related indications, each with specific dosing formulations and patient populations. Understanding these approved uses is essential for determining appropriate candidacy and ensuring evidence-based prescribing practices.
For type 2 diabetes mellitus, semaglutide is approved as an adjunct to diet and exercise to improve glycemic control in adults. The injectable formulation (Ozempic) is initiated at 0.25 mg once weekly and may be titrated up to a maximum maintenance dose of 2.0 mg weekly, depending on glycemic response and tolerability. The oral formulation (Rybelsus) is available in 3 mg, 7 mg, and 14 mg tablets taken once daily. Semaglutide may be used as monotherapy or in combination with other antidiabetic medications, including metformin, sulfonylureas, sodium-glucose cotransporter-2 (SGLT2) inhibitors, and insulin. Importantly, semaglutide is not indicated for the treatment of type 1 diabetes or diabetic ketoacidosis.
For chronic weight management, the higher-dose injectable formulation (Wegovy) is approved for adults with a body mass index (BMI) of 30 kg/m² or greater (obesity), or a BMI of 27 kg/m² or greater (overweight) in the presence of at least one weight-related comorbid condition. These comorbidities include hypertension, type 2 diabetes, or dyslipidemia. Wegovy is also approved for weight management in adolescents aged 12 years and older with a BMI at or above the 95th percentile for age and sex. The weight management dosing schedule begins at 0.25 mg weekly and escalates monthly to a maintenance dose of 2.4 mg weekly. In 2024, Wegovy received an additional FDA indication to reduce the risk of major adverse cardiovascular events (cardiovascular death, non-fatal myocardial infarction, or non-fatal stroke) in adults with established cardiovascular disease and either obesity or overweight.
It is important to note that semaglutide for weight management is indicated only as an adjunct to a reduced-calorie diet and increased physical activity, not as a standalone intervention. Patients should not use multiple semaglutide-containing products together or combine semaglutide with other GLP-1 receptor agonists.
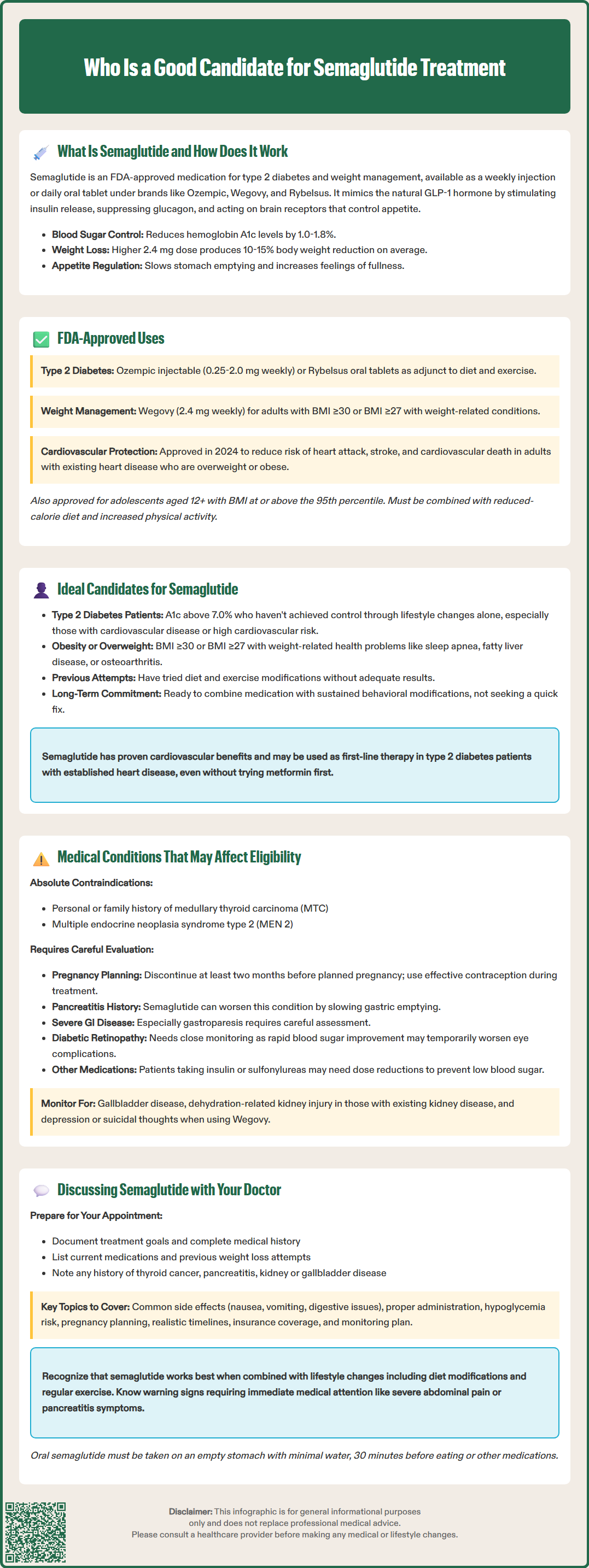
Determining appropriate candidacy for semaglutide requires comprehensive assessment of multiple clinical factors, including diagnosis, treatment goals, comorbidities, and patient preferences. Good candidates typically fall into well-defined clinical categories supported by robust evidence from randomized controlled trials.
For diabetes management, ideal candidates include adults with type 2 diabetes who have inadequate glycemic control despite lifestyle modifications, with or without other antidiabetic medications. Patients with hemoglobin A1c levels above target (generally >7.0% for most adults, though individualized targets may vary) who require additional glucose-lowering therapy represent appropriate candidates. According to the American Diabetes Association's Standards of Care, GLP-1 RAs with proven cardiovascular benefit, such as semaglutide, may be considered as first-line therapy in patients with type 2 diabetes who have established atherosclerotic cardiovascular disease or high cardiovascular risk, independent of metformin use. Ozempic has demonstrated cardiovascular benefits in patients with type 2 diabetes and established cardiovascular disease in the SUSTAIN-6 trial.
For weight management, good candidates include adults with obesity (BMI ≥30 kg/m²) or those who are overweight (BMI ≥27 kg/m²) with weight-related health complications. Patients who have attempted lifestyle modifications including dietary changes and increased physical activity without achieving adequate weight loss may benefit from pharmacologic intervention with semaglutide. Those with obesity-related comorbidities such as obstructive sleep apnea, nonalcoholic fatty liver disease, osteoarthritis, or polycystic ovary syndrome may experience improvements in these conditions as a result of significant weight reduction, though these are not FDA-approved indications for semaglutide. Candidates should demonstrate commitment to long-term lifestyle changes, as semaglutide is most effective when combined with sustained behavioral modifications. Patients seeking a comprehensive approach to metabolic health, rather than rapid short-term weight loss, are generally the most appropriate candidates for semaglutide therapy.
Several medical conditions and patient characteristics may contraindicate semaglutide use or require careful consideration and monitoring. Healthcare providers must conduct thorough screening to identify potential safety concerns before initiating therapy.
Semaglutide is absolutely contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with multiple endocrine neoplasia syndrome type 2 (MEN 2). In rodent studies, semaglutide caused thyroid C-cell tumors at clinically relevant exposures, and while the relevance to humans remains uncertain, the FDA-approved labeling includes a boxed warning regarding this risk. Semaglutide is also contraindicated in patients with a history of serious hypersensitivity to semaglutide or any of its components.
Semaglutide is contraindicated during pregnancy and should be discontinued at least two months before a planned pregnancy due to its long half-life. Weight loss medications are not recommended during pregnancy, and patients of reproductive potential should use effective contraception during treatment. Patients should discuss breastfeeding considerations with their healthcare provider.
Patients with a history of pancreatitis require careful evaluation before semaglutide initiation. While causality has not been definitively established, acute pancreatitis has been reported in clinical trials and post-marketing surveillance. Semaglutide should be discontinued if pancreatitis is suspected. Patients with severe gastrointestinal disease, particularly gastroparesis, may experience worsening symptoms due to semaglutide's effects on gastric emptying and may not be suitable candidates.
No dose adjustment is required for patients with renal impairment, including end-stage renal disease. However, gastrointestinal adverse effects may lead to dehydration and acute kidney injury, particularly in patients with pre-existing renal disease, so close monitoring is advised. Patients with diabetic retinopathy should be monitored carefully, as rapid improvement in glycemic control has been associated with temporary worsening of retinopathy, particularly in those with pre-existing retinopathy. Patients taking insulin or sulfonylureas may require dose reductions of these medications to prevent hypoglycemia when starting semaglutide. Additionally, patients should be monitored for gallbladder disease, as semaglutide has been associated with an increased risk of cholelithiasis and cholecystitis. For Wegovy specifically, monitoring for depression, suicidal thoughts, or unusual mood changes is recommended.
Initiating a conversation about semaglutide with your healthcare provider requires preparation and open communication about your health goals, medical history, and treatment preferences. A structured approach to this discussion can help ensure that all relevant factors are considered in determining whether semaglutide is appropriate for you.
Begin by clearly articulating your treatment goals and concerns. If you have type 2 diabetes, discuss your current glycemic control, including recent hemoglobin A1c values, and any challenges you face with your current medication regimen. If you are considering semaglutide for weight management, be prepared to discuss your weight history, previous weight loss attempts, and how excess weight affects your quality of life and overall health. Bring a comprehensive list of all current medications, including over-the-counter supplements, as drug interactions must be evaluated. Specifically mention if you are taking any other GLP-1 receptor agonists, as these should not be used concurrently with semaglutide. Disclose your complete medical history, particularly any personal or family history of thyroid cancer, pancreatitis, kidney disease, gallbladder disease, or gastrointestinal disorders.
Ask specific questions about what to expect from semaglutide therapy, including realistic timelines for seeing results, potential adverse effects, and how these will be monitored. Common adverse effects include nausea, vomiting, diarrhea, constipation, and abdominal pain, which typically diminish over time with gradual dose escalation. Inquire about the dosing schedule and administration technique for injectable formulations. For the oral formulation (Rybelsus), understand the specific administration requirements: it must be taken on an empty stomach with no more than 4 ounces of plain water, at least 30 minutes before eating, drinking, or taking other oral medications. If you take insulin or sulfonylureas, discuss the risk of hypoglycemia and how to monitor and manage low blood sugar.
Discuss pregnancy planning if applicable, as semaglutide should be discontinued at least two months before a planned pregnancy. Ask about the cost of therapy, insurance coverage, and available patient assistance programs, as medication affordability significantly impacts long-term adherence. Understand that semaglutide is not appropriate for everyone, and your doctor may recommend alternative therapies based on your individual circumstances. If semaglutide is prescribed, establish a clear monitoring plan, including follow-up appointments to assess efficacy, tolerability, and any necessary dose adjustments. Discuss warning signs that should prompt immediate medical attention, such as severe abdominal pain, signs of pancreatitis, or symptoms suggestive of thyroid tumors. Finally, recognize that successful treatment requires commitment to lifestyle modifications, including dietary changes and regular physical activity, as semaglutide is most effective as part of a comprehensive approach to metabolic health management.
Semaglutide for weight management (Wegovy) is FDA-approved only for adults with obesity (BMI ≥30) or overweight (BMI ≥27) with at least one weight-related comorbidity such as hypertension, type 2 diabetes, or dyslipidemia. It is not approved for cosmetic weight loss or patients who do not meet these clinical criteria.
No, you do not need diabetes to be prescribed semaglutide. While Ozempic and Rybelsus are approved for type 2 diabetes, Wegovy is specifically approved for chronic weight management in patients with obesity or overweight with weight-related health conditions, regardless of diabetes status.
Semaglutide is contraindicated in patients with personal or family history of medullary thyroid carcinoma, multiple endocrine neoplasia syndrome type 2, or serious hypersensitivity to the medication. It should not be used during pregnancy and requires careful evaluation in patients with history of pancreatitis, severe gastrointestinal disease, or diabetic retinopathy.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.