LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

How does GLP-1 make you feel? Most patients starting GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) or tirzepatide (Mounjaro, Zepbound) notice significant changes in appetite and digestion within days. The most common sensation is early satiety—feeling comfortably full after smaller portions—alongside gastrointestinal effects like nausea, bloating, or constipation. These medications work by mimicking a natural gut hormone that slows stomach emptying and reduces hunger signals in the brain. While side effects typically peak during the first 4–8 weeks, most patients adapt over time, with appetite regulation persisting as initial discomfort resolves. Understanding what to expect helps you navigate treatment safely and effectively.
Quick Answer: GLP-1 medications typically make you feel full earlier and reduce hunger by slowing stomach emptying and affecting brain appetite centers, though initial side effects like nausea and bloating are common.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications originally developed for type 2 diabetes management and now widely prescribed for chronic weight management. These medications include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda). Tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist. Understanding their mechanisms helps explain the physical sensations patients commonly experience.
GLP-1 medications work by mimicking a naturally occurring intestinal hormone that regulates blood glucose and appetite. When you eat, your gut releases native GLP-1, which stimulates insulin secretion from the pancreas, suppresses glucagon release, and slows gastric emptying. These medications amplify these physiological effects by binding to GLP-1 receptors throughout the body, including in the pancreas, gastrointestinal tract, and brain regions that control appetite and satiety. Tirzepatide additionally activates GIP receptors, which may contribute to its effects on appetite and metabolism.
Key contributors to how you feel include delayed gastric emptying—food remains in your stomach longer than usual, creating prolonged fullness—and effects on appetite centers in the hypothalamus, reducing hunger signals and food cravings. This dual action on both peripheral digestion and central appetite regulation explains why many patients report feeling satisfied with smaller portions and experiencing reduced interest in food.
These medications are typically administered by subcutaneous injection, either weekly (semaglutide, dulaglutide, tirzepatide) or daily (liraglutide), with dosing gradually increased over several weeks to minimize side effects. An oral formulation of semaglutide (Rybelsus) is also available for type 2 diabetes. The FDA has approved specific formulations for diabetes management and others for chronic weight management in adults with obesity or overweight with weight-related comorbidities.
Important safety information: These medications carry a boxed warning about the risk of thyroid C-cell tumors and are contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Weight management formulations are contraindicated during pregnancy.
Most patients beginning GLP-1 therapy experience noticeable changes in appetite and digestion within the first few doses. The most commonly reported sensation is early satiety—feeling full after eating much smaller portions than usual. Many patients describe this as a persistent comfortable fullness or lack of interest in food that differs from typical hunger suppression. This effect typically becomes apparent within the first week of treatment and may intensify as the dose increases.
Gastrointestinal effects are the most frequent side effects, with rates varying by medication and dose. For example, in clinical trials of semaglutide 2.4 mg (Wegovy), nausea occurred in approximately 44% of patients, while rates for tirzepatide and other GLP-1s vary:
Nausea: Often described as mild queasiness, particularly after eating, though some patients experience more pronounced nausea
Bloating and abdominal fullness: A sensation of delayed digestion or food sitting heavily in the stomach
Changes in bowel habits: Constipation affects approximately 15-30% of patients (varying by medication and dose), while some experience diarrhea or alternating patterns
Decreased appetite: Beyond simple fullness, many report a fundamental shift in food thoughts, with reduced cravings and less mental preoccupation with eating
Some patients report fatigue or low energy, particularly during the initial weeks. Fatigue is a labeled adverse reaction for some products (e.g., Wegovy) and may relate to reduced caloric intake, adjustment to metabolic changes, or direct medication effects.
Physical sensations at the injection site are generally minimal—most patients report only mild stinging or temporary redness. Systemic effects like headache occur in approximately 10–15% of patients but typically resolve within the first month of therapy.
Importantly, when used as monotherapy, these medications have a low risk of hypoglycemia. However, when combined with insulin or sulfonylureas, the risk of low blood sugar increases significantly, requiring careful monitoring and possible dose adjustments of those medications.
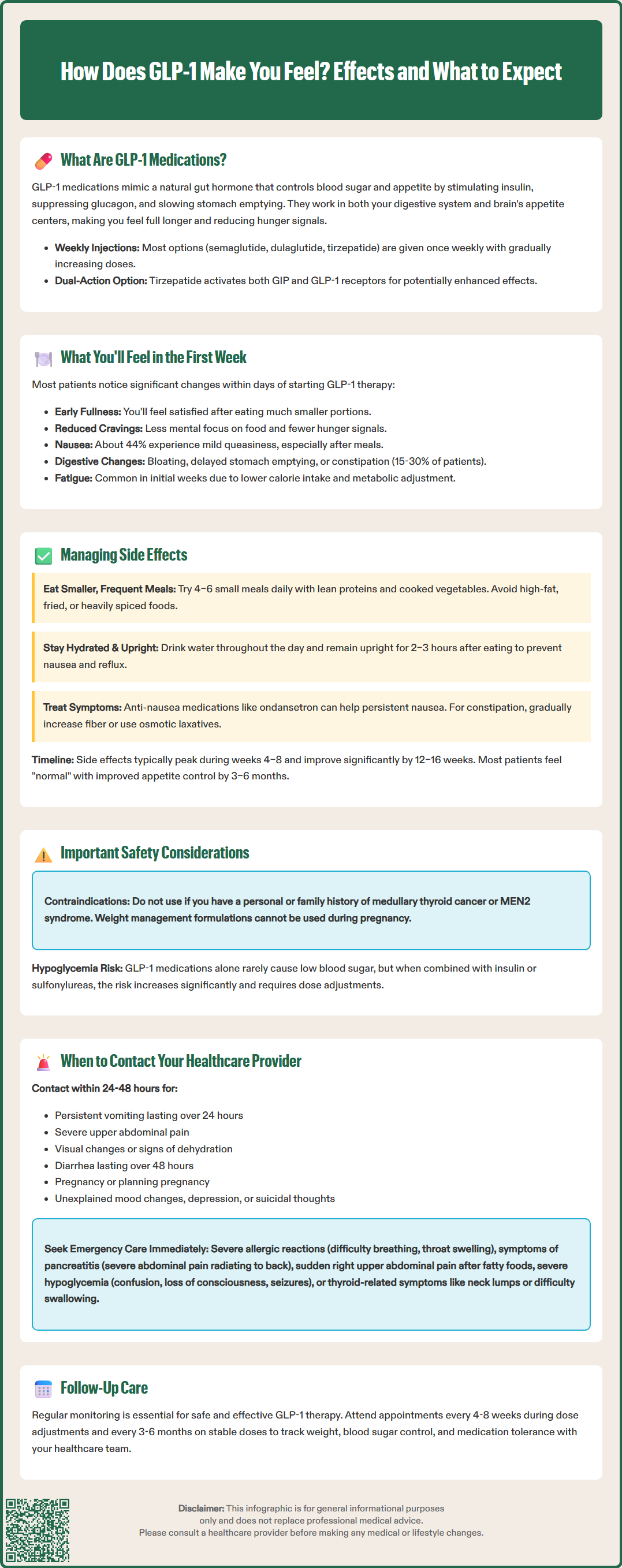
The majority of GLP-1-related side effects are most pronounced during dose initiation and escalation, with gradual improvement as your body adapts to the medication. According to clinical trials, gastrointestinal symptoms typically peak during the first 4–8 weeks of therapy, with substantial improvement for many patients by 12–16 weeks, though individual experiences vary based on the specific medication and titration schedule.
Practical strategies for managing common side effects include:
Eat smaller, more frequent meals: Rather than three large meals, consume 4–6 smaller portions throughout the day to avoid overwhelming your slowed digestive system
Choose easily digestible foods: Lean proteins, cooked vegetables, and simple carbohydrates are generally better tolerated than high-fat, fried, or heavily spiced foods
Stay well-hydrated: Adequate fluid intake helps prevent constipation and may reduce nausea; aim for sufficient water throughout the day (specific needs vary by individual and medical conditions)
Avoid lying down immediately after eating: Remaining upright for 2–3 hours after meals can reduce reflux and bloating sensations
Consider timing of injections: Some patients find adjusting the time of day for their injection based on personal tolerance helpful, though this is based on individual preference rather than clinical evidence
For persistent nausea, your healthcare provider may recommend short-term use of anti-nausea medications such as ondansetron. For constipation, increasing dietary fiber gradually (with adequate fluid intake), using osmotic laxatives like polyethylene glycol (PEG), or occasionally adding stimulant laxatives (senna, bisacodyl) may provide relief. It's important to address constipation proactively, as severe cases can exacerbate abdominal discomfort.
Over time, most patients report that the initial side effects resolve while the beneficial effects on appetite regulation persist. By 3–6 months, many individuals describe feeling "normal" with their new eating patterns, experiencing hunger at appropriate times but with better portion control and reduced cravings.
If side effects persist beyond the initial adaptation period, do not accelerate dose increases. Your provider may need to slow the escalation schedule or maintain a lower maintenance dose if higher doses produce intolerable symptoms while still achieving therapeutic goals.
While most GLP-1 side effects are manageable and self-limiting, certain symptoms warrant prompt medical evaluation. Understanding when to seek guidance ensures patient safety and optimal therapeutic outcomes.
Contact your healthcare provider within 24–48 hours if you experience:
Persistent vomiting: Inability to keep down fluids for more than 24 hours, which may lead to dehydration
Severe abdominal pain: Particularly sharp, constant pain in the upper abdomen that may radiate to the back, which could indicate pancreatitis
Visual changes: Blurred vision or difficulty focusing, especially in patients with pre-existing diabetic retinopathy
Signs of dehydration: Decreased urination, dark urine, dizziness upon standing, or extreme thirst
Persistent diarrhea: Lasting more than 48 hours or accompanied by fever
Pregnancy or planning pregnancy: Weight management formulations are contraindicated during pregnancy
Seek immediate emergency care for:
Severe allergic reactions: Difficulty breathing, throat swelling, widespread rash, or rapid heart rate
Symptoms of pancreatitis: Severe, persistent abdominal pain (often radiating to the back), accompanied by nausea and vomiting
Signs of gallbladder disease: Sudden severe pain in the right upper abdomen, particularly after eating fatty foods, with or without fever
Symptoms of hypoglycemia (in patients taking insulin or sulfonylureas concurrently): Severe shakiness, confusion, loss of consciousness, or seizures
Signs of intestinal obstruction: Severe abdominal distension, persistent inability to pass stool or gas, vomiting
Symptoms of acute kidney injury: Markedly decreased urine output, swelling of legs or feet, especially with severe dehydration
Thyroid-related symptoms: New lump or swelling in the neck, hoarseness, difficulty swallowing, or shortness of breath
Additionally, contact your provider if you experience unexplained mood changes, depression, or suicidal thoughts. The FDA is evaluating reports of suicidal thoughts or behaviors in patients taking these medications, though a causal relationship has not been established.
Routine follow-up appointments are essential for monitoring therapeutic response and adjusting treatment. Your provider should assess weight changes, glycemic control (if applicable), tolerance of current dose, and readiness for dose escalation. Most protocols recommend follow-up every 4–8 weeks during dose titration and every 3–6 months once on a stable maintenance dose. Open communication about how the medication makes you feel—both positive effects and concerning symptoms—enables your healthcare team to optimize your treatment plan and ensure safe, effective therapy.
Most patients notice changes in appetite and early satiety within the first week of starting GLP-1 therapy. Gastrointestinal side effects like nausea and bloating typically appear during the initial doses and peak within the first 4–8 weeks as the dose is gradually increased.
Yes, most GLP-1-related side effects, particularly gastrointestinal symptoms, improve substantially by 12–16 weeks as your body adapts to the medication. The beneficial effects on appetite regulation typically persist while initial discomfort resolves, though individual experiences vary.
Early satiety from GLP-1 medications is described as feeling comfortably full after eating much smaller portions than usual, often accompanied by reduced interest in food and decreased cravings. This sensation results from delayed gastric emptying and effects on brain appetite centers in the hypothalamus.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.