LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Restarting tirzepatide after a month requires careful clinical consideration to ensure safety and effectiveness. Tirzepatide (Mounjaro, Zepbound), a dual GIP/GLP-1 receptor agonist, is substantially eliminated from the body within 2–3 weeks of discontinuation. Patients may interrupt treatment due to side effects, supply shortages, financial constraints, or medical procedures. After a one-month break, healthcare providers typically recommend restarting at a lower dose—often 2.5 mg weekly—then gradually re-escalating to minimize gastrointestinal side effects while restoring metabolic benefits. Understanding the physiological changes during treatment gaps and following individualized resumption protocols helps optimize outcomes for both diabetes management and weight control.
Quick Answer: After a one-month break from tirzepatide, patients should typically restart at a lower dose (usually 2.5 mg weekly) and gradually re-escalate to minimize gastrointestinal side effects while restoring therapeutic benefits.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved for type 2 diabetes management and chronic weight management. Despite its efficacy, patients may discontinue treatment for various reasons and later consider resuming therapy.
Common reasons for temporary discontinuation include:
Gastrointestinal adverse effects – Nausea, vomiting, diarrhea, and constipation are the most frequently reported side effects, particularly during dose escalation. Some patients require a treatment break to allow symptoms to resolve.
Supply chain disruptions – Periodic shortages have affected tirzepatide availability, forcing involuntary treatment interruptions.
Financial constraints – High out-of-pocket costs may necessitate temporary discontinuation until insurance coverage or financial assistance becomes available.
Surgical procedures or acute illness – Healthcare providers may recommend individualizing tirzepatide management before procedures based on the patient's symptoms, procedure type, and anesthesia risk. Coordination with the surgical team is recommended.
Pregnancy planning or discovery – Tirzepatide is not recommended during pregnancy. Women who become pregnant or are planning conception should discontinue tirzepatide and discuss alternative diabetes therapies with pregnancy safety data. Weight loss medications should be avoided during pregnancy.
Many patients who achieve initial weight loss or glycemic targets may mistakenly believe they can maintain results without continued medication. However, tirzepatide works through ongoing pharmacological mechanisms rather than producing permanent metabolic changes. When patients recognize weight regain or worsening glucose control after discontinuation, they often seek guidance on safely restarting treatment.
Importantly, tirzepatide carries a boxed warning for risk of thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), and is contraindicated in patients with a personal or family history of MTC or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Patients should inform their healthcare provider of any thyroid nodules, neck mass, difficulty swallowing, or persistent hoarseness.
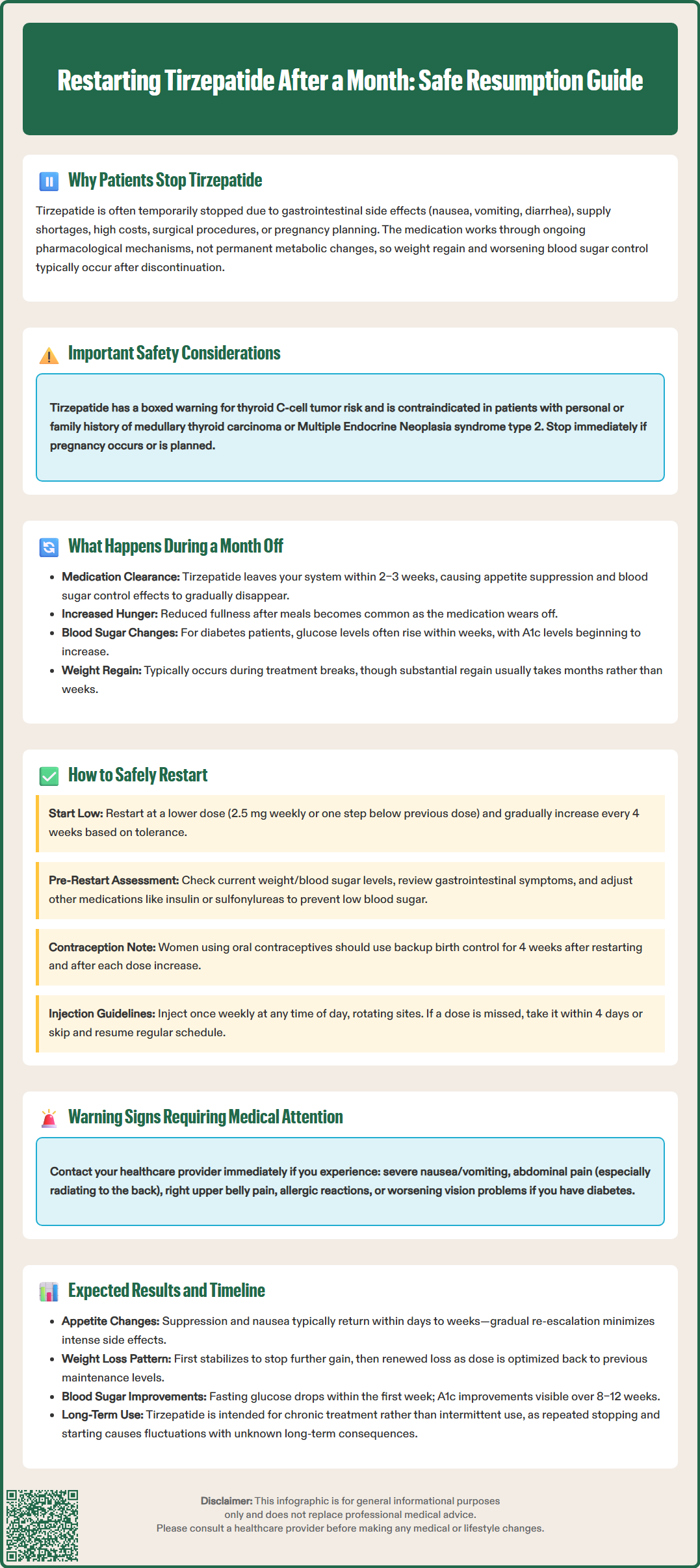
Tirzepatide has a half-life of approximately 5 days, meaning the medication is substantially eliminated from the body within 2–3 weeks after the last dose. During a month-long interruption, several physiological changes occur as the drug's effects dissipate.
Metabolic and hormonal changes include restoration of baseline gastric emptying rates, return of pre-treatment appetite signals, and loss of the medication's insulinotropic effects. The dual GIP/GLP-1 receptor agonism that suppresses appetite, enhances satiety, and improves insulin secretion gradually diminishes. Many patients report increased hunger and reduced fullness after meals as the medication's effects wear off, though the timing varies between individuals.
Weight regain is common during treatment interruptions. Clinical trial data from withdrawal studies (such as SURMOUNT-4) demonstrate that patients regain weight after discontinuing GLP-1 receptor agonists and related medications. The rate and extent of weight regain vary individually based on dietary habits, physical activity, and individual metabolic factors. Substantial weight regain typically occurs over longer periods (months to a year) rather than within a single month.
Glycemic control deterioration occurs in patients with type 2 diabetes. Hemoglobin A1c levels may begin rising within weeks of discontinuation, though significant changes typically require longer periods. Fasting glucose and postprandial glucose excursions often increase as tirzepatide's insulinotropic and glucagon-suppressing effects wane.
Cardiovascular and metabolic parameters may also shift. Blood pressure and lipid profiles that improved during treatment may trend toward baseline values, though the timeline and magnitude vary between individuals. These changes underscore that tirzepatide produces pharmacological rather than curative effects—benefits persist only with continued treatment. Patients should understand that a month-long gap typically necessitates careful consideration of resumption protocols, often including dose re-titration to minimize side effects.
Restarting tirzepatide after a one-month interruption requires clinical judgment and individualized decision-making. The FDA-approved prescribing information does not provide specific guidance for treatment resumption after breaks, so healthcare providers must balance efficacy with tolerability.
Dose selection considerations depend on several factors. After a month-long break, a conservative approach often involves restarting at a lower dose—typically the starting dose of 2.5 mg weekly or one step below the previous maintenance dose—then re-escalating according to the standard titration schedule. For Mounjaro (diabetes indication), dose increases occur in 2.5 mg increments up to 15 mg weekly. For Zepbound (weight management indication), doses increase from 2.5 mg to 5 mg, 7.5 mg, 10 mg, 12.5 mg, and 15 mg at 4-week intervals as tolerated.
The American Diabetes Association (ADA) and American College of Physicians (ACP) emphasize individualized treatment approaches for glucose-lowering medications, though specific guidance on treatment interruption and resumption is limited. Clinical judgment should incorporate the patient's previous tolerance, reason for discontinuation, current metabolic status, and treatment goals.
Pre-restart assessment should include:
Review of the reason for discontinuation and whether it has been adequately addressed
Current weight and glycemic status (if diabetic)
Assessment of gastrointestinal symptoms and any contraindications
Medication reconciliation to identify potential drug interactions
For patients taking insulin or sulfonylureas, consider dose reductions to prevent hypoglycemia
For women of childbearing potential using oral contraceptives, recommend backup contraception for 4 weeks after restarting and after each dose increase
Discussion of realistic expectations and commitment to continued treatment
Patient counseling is essential. Advise patients that tirzepatide can be administered subcutaneously at any time of day, with or without meals. Injection sites should be rotated. If a dose is missed, it should be administered within 4 days of the scheduled dose; if more than 4 days have passed, skip the missed dose and resume at the next scheduled time. Patients should report severe or persistent nausea, vomiting, abdominal pain (especially if radiating to the back, which may indicate pancreatitis), right upper quadrant pain (possible gallbladder disease), or signs of allergic reaction. Patients with diabetes and pre-existing retinopathy should be monitored for worsening retinopathy during rapid improvement in glycemic control.
Patients restarting tirzepatide after a one-month break should understand that response patterns may differ from their initial treatment course, though the medication's fundamental mechanisms remain unchanged.
Appetite suppression and gastrointestinal effects typically re-emerge as tirzepatide reaches therapeutic levels. Patients often notice reduced hunger and earlier satiety within days to weeks of resumption, though individual responses vary. Gastrointestinal side effects—particularly nausea—may be more pronounced than during initial treatment if restarting at a higher dose. This phenomenon occurs because tolerance to these effects can diminish during treatment gaps. Starting at a lower dose and re-escalating gradually minimizes this risk.
Weight loss trajectory after restarting generally follows a pattern of initial stabilization (stopping further weight regain), followed by renewed weight loss as the dose is optimized. Patients who restart at lower doses should not expect the same rate of weight loss achieved at their previous maintenance dose until re-escalation is complete. In clinical trials, tirzepatide produced dose-dependent weight loss, with higher doses (10 mg and 15 mg weekly) achieving greater reductions than lower doses. The timeline to return to previous weight loss varies based on the re-titration schedule and individual response.
Glycemic improvements in patients with type 2 diabetes occur relatively quickly, with fasting glucose reductions often observable within the first week and hemoglobin A1c improvements becoming apparent over 8–12 weeks. The insulinotropic effects of tirzepatide are glucose-dependent, meaning they activate when blood glucose is elevated, providing rapid benefit. Patients with pre-existing diabetic retinopathy should be monitored for worsening retinopathy during rapid improvement in glycemic control.
Long-term considerations include the recognition that tirzepatide is a chronic disease management medication rather than a short-term intervention. Patients who experience recurrent treatment interruptions may face fluctuations in weight and glucose control. There is limited data on the impact of repeated stopping and starting on long-term outcomes. Discussing strategies for treatment continuity—including addressing financial barriers, managing side effects proactively, and establishing realistic long-term goals—is essential for sustained benefit.
Most healthcare providers recommend restarting at 2.5 mg weekly or one step below your previous maintenance dose, then gradually increasing every 4 weeks to minimize gastrointestinal side effects while restoring therapeutic benefits.
Some weight regain is possible during a month off tirzepatide as the medication's appetite-suppressing effects diminish, though substantial regain typically occurs over longer periods depending on diet, activity level, and individual metabolism.
Appetite suppression typically returns within days to weeks of restarting, while glycemic improvements in diabetes patients often begin within the first week. Full therapeutic effects depend on reaching your optimal maintenance dose through gradual re-escalation.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.