LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
How long does it take for tirzepatide to work? Many patients beginning this dual GIP/GLP-1 receptor agonist wonder when they'll notice improvements in blood sugar control or weight loss. Tirzepatide, marketed as Mounjaro for type 2 diabetes and Zepbound for chronic weight management, works through a unique dual mechanism that affects both glucose regulation and appetite. While some effects begin within days, optimal results typically emerge over several months. Understanding the expected timeline helps patients maintain realistic expectations and stay committed to treatment. This article examines when tirzepatide starts working, factors influencing response time, and strategies to maximize therapeutic benefits.
Quick Answer: Tirzepatide begins lowering blood sugar within 1-2 weeks, with peak A1C reductions at 20-24 weeks, while initial weight loss typically starts within 2-4 weeks, with maximum effects occurring between 36-72 weeks.
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for two distinct indications: treatment of type 2 diabetes mellitus (Mounjaro) and chronic weight management (Zepbound) in adults with BMI ≥30 kg/m² or ≥27 kg/m² with at least one weight-related comorbidity. It is not indicated for type 1 diabetes. Tirzepatide represents the first dual incretin receptor agonist available in clinical practice.
The medication works through a dual mechanism of action. As a GIP receptor agonist, tirzepatide enhances insulin secretion and may potentially improve insulin sensitivity while reducing glucagon secretion, though these mechanisms continue to be studied. Simultaneously, its GLP-1 receptor agonist activity promotes glucose-dependent insulin release, suppresses inappropriate glucagon secretion, slows gastric emptying, and reduces appetite through central nervous system pathways. This dual action creates a synergistic effect that appears more potent than GLP-1 agonists alone.
Tirzepatide is administered as a once-weekly subcutaneous injection, typically in the abdomen, thigh, or upper arm. The medication is available in escalating doses ranging from 2.5 mg to 15 mg, allowing for gradual titration to optimize efficacy while minimizing gastrointestinal side effects. The pharmacokinetic profile shows steady-state concentrations are achieved after approximately four weeks of consistent dosing.
Clinical trials have demonstrated that tirzepatide produces substantial reductions in hemoglobin A1C (often exceeding 2 percentage points) in patients with type 2 diabetes. In obesity trials (SURMOUNT program), higher doses produced weight loss averaging 15-20% of body weight, while diabetes trials (SURPASS program) showed more modest but still significant weight reductions. These effects make tirzepatide valuable for patients with type 2 diabetes who also struggle with obesity.
Importantly, tirzepatide carries a boxed warning regarding thyroid C-cell tumors observed in rodent studies. It is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or in patients with Multiple Endocrine Neoplasia syndrome type 2.
Understanding the timeline for tirzepatide's effects requires distinguishing between different therapeutic outcomes, as glucose control and weight loss follow somewhat different trajectories. For glycemic control, many patients begin experiencing improvements in fasting glucose levels within the first 1-2 weeks of treatment, though individual responses vary considerably.
Hemoglobin A1C reductions—the gold standard for assessing diabetes control—become apparent at the first measurement point, typically 8-12 weeks after initiation. Based on SURPASS clinical trial data, peak A1C reductions generally occur between 20-24 weeks of treatment, though some patients continue to see incremental improvements up to 40 weeks. Most patients achieved their maximum glucose-lowering benefit by approximately six months of consistent therapy.
Weight loss follows a more gradual but sustained pattern. Most patients notice initial weight reduction within the first 2-4 weeks, often coinciding with reduced appetite and smaller portion sizes. Significant weight loss—defined as 5% or more of baseline body weight—typically occurs by 12-16 weeks. The most substantial weight reductions are generally observed between 36-72 weeks of treatment, with the SURMOUNT trials showing continued weight loss throughout the study duration. Weight loss trajectories and magnitudes differ between patients with obesity without diabetes (SURMOUNT trials) and those with type 2 diabetes (SURPASS trials), with the former typically showing greater percentage weight loss.
It is important to note that individual responses vary considerably. Some patients experience rapid initial improvements, while others require several months to achieve optimal results. Factors such as baseline metabolic status, adherence to lifestyle modifications, and dose escalation schedule all influence the timeline. Patients should maintain realistic expectations and understand that tirzepatide is designed for long-term metabolic improvement rather than immediate dramatic changes.
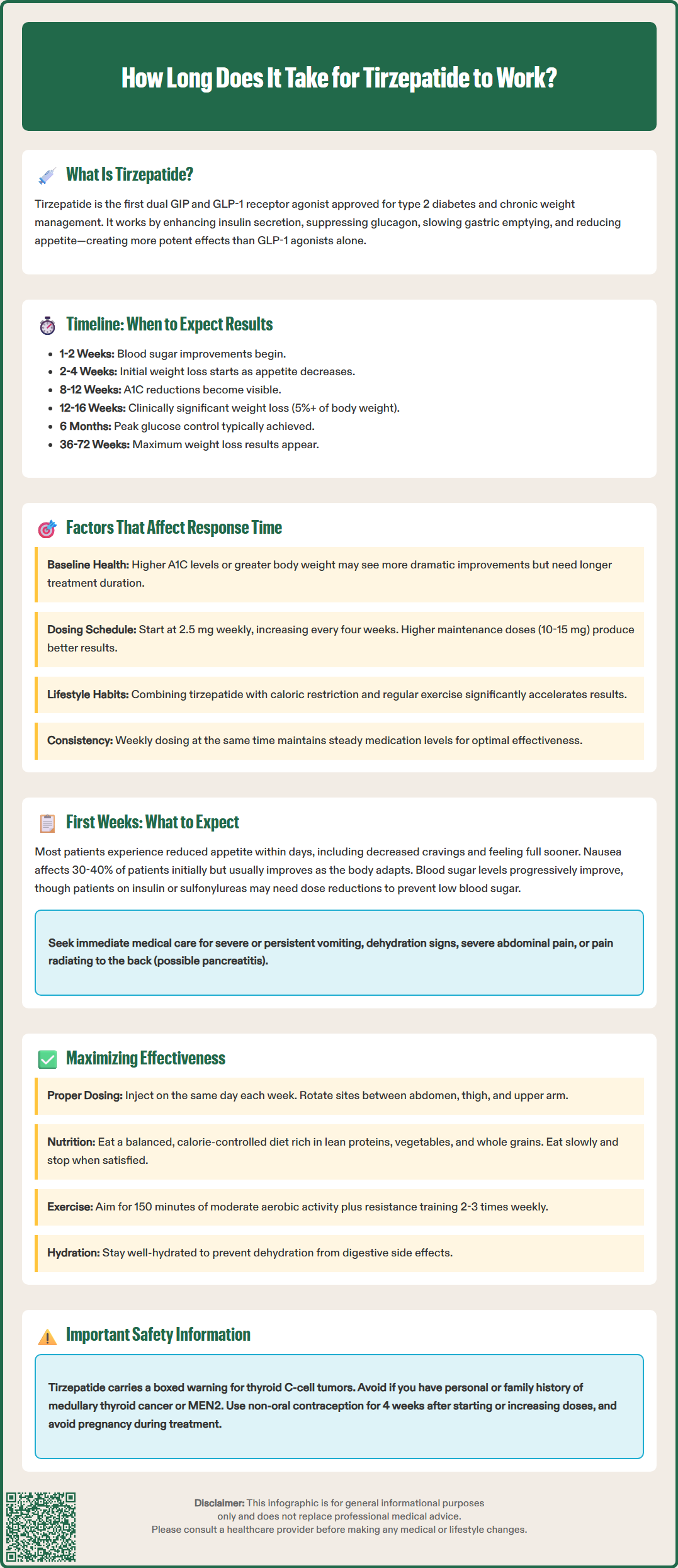
Multiple patient-specific and treatment-related factors influence how quickly and effectively tirzepatide produces clinical benefits. Baseline metabolic status plays a crucial role—patients with higher initial A1C levels (above 9%) often experience more dramatic absolute reductions, though they may take longer to reach target glucose levels. Similarly, individuals with greater baseline body weight typically lose more absolute pounds but may require extended treatment duration to achieve percentage-based weight loss goals.
Dose escalation strategy significantly impacts both efficacy and tolerability. The FDA-approved titration schedule begins with 2.5 mg weekly for four weeks, increasing by 2.5 mg increments every four weeks as tolerated. Patients who can advance to higher maintenance doses (10-15 mg) generally achieve superior outcomes compared to those who remain at lower doses due to side effects. However, aggressive dose escalation may trigger gastrointestinal adverse effects that compromise adherence and delay optimal results.
Concomitant medications can influence tirzepatide's effectiveness. Patients taking medications that promote weight gain (such as insulin, sulfonylureas, or certain antipsychotics) may experience attenuated weight loss, though glucose control typically improves regardless. When used with insulin or sulfonylureas, there is an increased risk of hypoglycemia that may necessitate dose adjustments of these medications. Additionally, tirzepatide may reduce the absorption of oral medications due to delayed gastric emptying, particularly affecting oral contraceptives, which may require alternative contraception methods for 4 weeks after initiation and each dose increase.
Lifestyle factors substantially modulate treatment response. Patients who combine tirzepatide with caloric restriction and regular physical activity consistently demonstrate faster and more pronounced improvements in both glucose control and weight loss. Conversely, poor medication adherence—missing doses or inconsistent injection timing—disrupts steady-state pharmacokinetics and delays therapeutic benefits. Gastrointestinal side effects, particularly nausea and vomiting, can impair nutritional intake and medication continuation, potentially slowing progress. Individual variability in response to incretin-based therapies is common and may reflect differences in underlying pathophysiology.
The initial weeks of tirzepatide therapy represent a critical adjustment period during which patients experience both therapeutic effects and potential side effects. Most patients notice reduced appetite within the first few days of their initial injection, often describing decreased food cravings, earlier satiety during meals, and reduced interest in snacking between meals. This appetite suppression stems from tirzepatide's effects on central appetite regulation and delayed gastric emptying.
Gastrointestinal side effects are the most common early experiences, with nausea affecting approximately 30-40% of patients during dose initiation and escalation, varying by dose level. Nausea is typically mild to moderate in severity and often improves with continued use as the body adapts. Other digestive symptoms may include occasional vomiting (reported in 8-24% of patients), diarrhea, constipation, or abdominal discomfort. The timing and duration of these symptoms vary between individuals. Patients should be counseled that gastrointestinal symptoms usually do not indicate treatment failure and often resolve with continued therapy.
Glucose monitoring during the first weeks reveals progressive improvements in fasting and postprandial glucose levels. Patients using continuous glucose monitors often observe flattening of glucose excursions and reduction in time spent above target range. Those taking sulfonylureas or insulin concurrently require careful monitoring for hypoglycemia. The American Diabetes Association recommends considering proactive reduction of insulin doses (particularly basal insulin, often by approximately 20% if A1C is <8% or there is high hypoglycemia risk) when initiating GLP-1 receptor agonists, with individualized adjustments and close monitoring.
Patients should maintain adequate hydration during the initial treatment period, as gastrointestinal side effects can increase dehydration risk, which may lead to acute kidney injury in severe cases. Eating smaller, more frequent meals and avoiding high-fat foods may help minimize nausea. Tirzepatide is not recommended for patients with severe gastrointestinal disease, including severe gastroparesis. Any severe or persistent vomiting, signs of dehydration, severe abdominal pain, or symptoms suggestive of pancreatitis (persistent severe abdominal pain radiating to the back) warrant immediate medical evaluation and possible suspension of treatment. Most patients find that the initial adjustment period, while sometimes uncomfortable, is manageable and leads to meaningful clinical improvements.
Optimizing tirzepatide therapy requires attention to both pharmacological and behavioral strategies. Adherence to the prescribed titration schedule is fundamental—the gradual dose escalation protocol (starting at 2.5 mg and increasing every four weeks) balances efficacy against tolerability. Patients should inject tirzepatide on the same day each week, though the specific time of day is flexible. According to the FDA label, if a dose is missed and the next scheduled dose is more than 4 days away, administer the missed dose as soon as possible. If less than 4 days away, skip the missed dose and administer the next dose on the regularly scheduled day.
Injection technique merits attention to detail. Rotating injection sites (abdomen, thigh, upper arm) helps prevent local reactions and ensures consistent absorption. The medication should be stored in the refrigerator until first use, though it may be kept at room temperature for up to 21 days. Patients should inspect the solution before each injection—it should be clear and colorless; any cloudiness or discoloration indicates the medication should not be used.
Dietary modifications significantly enhance tirzepatide's effectiveness. A balanced, calorie-controlled diet rich in lean proteins, vegetables, and whole grains supports both glucose control and weight loss. Adequate protein intake helps preserve lean muscle mass during weight reduction, though specific targets should be individualized, particularly for patients with kidney disease. Patients should eat slowly and stop when comfortably satisfied rather than completely full, as tirzepatide's effects on gastric emptying can cause discomfort with overeating. Limiting high-fat and fried foods may reduce gastrointestinal side effects.
Regular physical activity amplifies metabolic benefits. The U.S. Department of Health and Human Services and American Diabetes Association recommend at least 150 minutes of moderate-intensity aerobic activity weekly, combined with resistance training 2-3 times weekly. Exercise improves insulin sensitivity, supports weight loss, and helps maintain muscle mass. Patients should monitor for hypoglycemia during and after exercise, particularly if taking insulin or sulfonylureas concurrently.
Important safety considerations include: tirzepatide is not indicated for type 1 diabetes; pregnancy should be avoided during treatment (effective contraception is recommended); women using oral contraceptives should use an alternative or backup method for 4 weeks after initiation and each dose increase; and the medication is contraindicated in patients with a personal or family history of medullary thyroid carcinoma, Multiple Endocrine Neoplasia syndrome type 2, or a prior serious hypersensitivity reaction to tirzepatide. Regular follow-up with healthcare providers ensures appropriate dose titration and monitoring for adverse effects.
Most patients experience improvements in fasting glucose levels within 1-2 weeks of starting tirzepatide. Hemoglobin A1C reductions become apparent at 8-12 weeks, with peak reductions typically occurring between 20-24 weeks of consistent treatment.
Initial weight reduction typically begins within 2-4 weeks as appetite decreases and portion sizes reduce. Significant weight loss generally occurs by 12-16 weeks, with maximum effects observed between 36-72 weeks of treatment.
If your next scheduled dose is more than 4 days away, administer the missed dose as soon as possible. If less than 4 days remain until your next dose, skip the missed dose and resume your regular weekly schedule.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.