LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Bloating is one of the most common side effects experienced by patients taking GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) or tirzepatide (Mounjaro, Zepbound). These medications slow gastric emptying to improve blood sugar control and reduce appetite, but this mechanism can cause uncomfortable abdominal distension and fullness. Fortunately, targeted dietary modifications, lifestyle adjustments, and medical strategies can significantly reduce GLP-1-related bloating. Understanding why these symptoms occur and implementing evidence-based management techniques helps patients maintain their treatment regimen while minimizing discomfort and improving quality of life during therapy.
Quick Answer: GLP-1-related bloating can be reduced through smaller frequent meals, avoiding high-fat and gas-producing foods, eating slowly, gentle post-meal walking, and dose adjustment strategies under medical supervision.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists (e.g., semaglutide in Ozempic and Wegovy) and the dual GIP/GLP-1 receptor agonist tirzepatide (Mounjaro, Zepbound) work by mimicking naturally occurring hormones that regulate blood glucose and appetite. These medications slow gastric emptying—the rate at which food moves from the stomach into the small intestine—which contributes to increased satiety and improved glycemic control. However, this delayed gastric emptying is also the primary mechanism behind bloating and other gastrointestinal symptoms experienced by many patients.
When food remains in the stomach longer than usual, it can lead to feelings of fullness, abdominal distension, and bloating. According to FDA-approved prescribing information, gastrointestinal adverse effects occur commonly with these medications, with nausea reported in 16-44% of patients, vomiting in 6-24%, and abdominal pain or distension in 5-18%, depending on the specific medication and dosage. These symptoms typically emerge within the first few weeks of treatment or following dose increases.
Additionally, these medications may affect gut motility beyond the stomach, potentially altering the movement of gas and digestive contents through the intestines. The gastric-emptying effect often attenuates over time after dose stabilization. The severity of bloating varies considerably among individuals and may correlate with dietary choices, eating patterns, and the specific medication prescribed. Notably, these medications are not recommended for patients with severe gastroparesis or other significant gastrointestinal disorders, as stated in their FDA labeling.
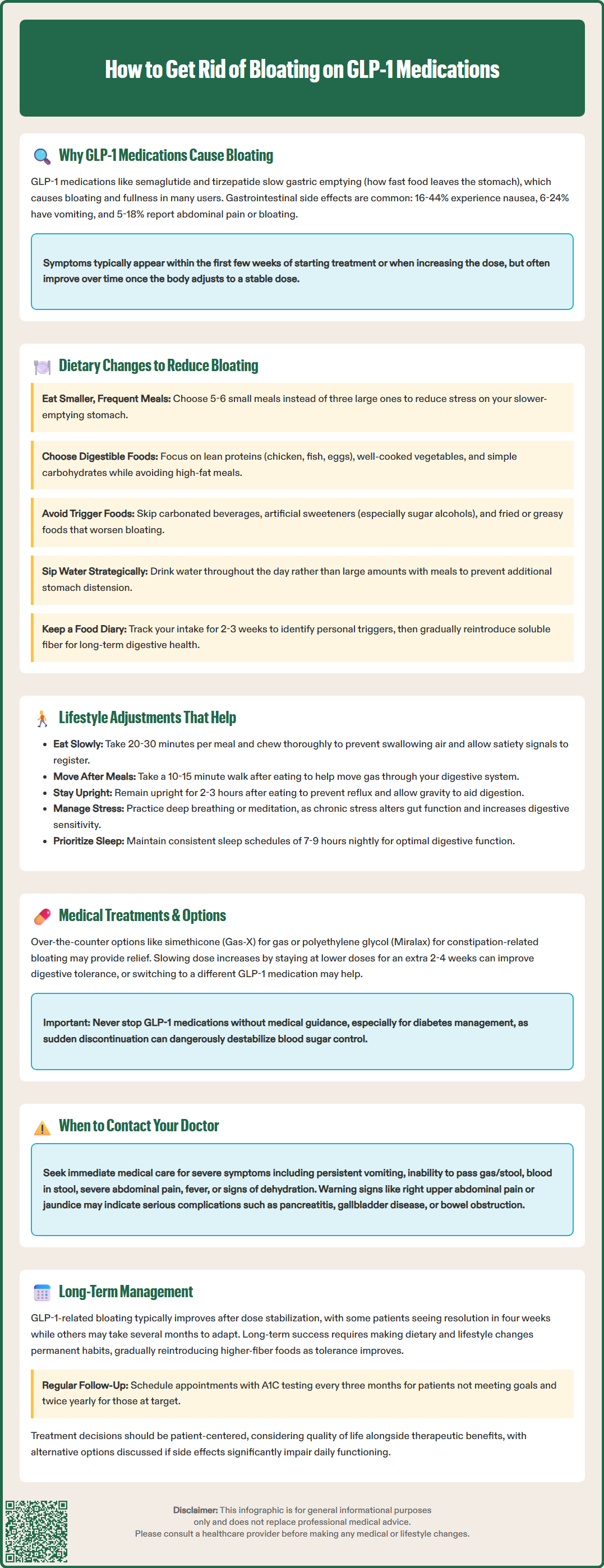
Modifying dietary habits may help manage GLP-1-related bloating. Given the delayed gastric emptying caused by these medications, consuming smaller, more frequent meals throughout the day rather than three large ones may reduce abdominal distension. Smaller portions place less mechanical stress on an already slower-emptying stomach.
Patients may find that easily digestible foods are better tolerated during GLP-1 therapy. Lean proteins such as chicken, fish, and eggs; well-cooked vegetables; and simple carbohydrates like white rice or refined grains are generally better tolerated than heavy, fatty, or highly processed foods. High-fat meals delay gastric emptying further, potentially compounding the medication's effect and worsening bloating. The American Diabetes Association recommends limiting saturated fat intake regardless, making this adjustment both symptom-focused and evidence-based for metabolic health.
Foods to minimize or avoid include:
Carbonated beverages, which introduce additional gas
High-fiber foods initially (beans, cruciferous vegetables, whole grains), though fiber remains important long-term
Artificial sweeteners, particularly sugar alcohols (sorbitol, xylitol), which can ferment in the gut
Dairy products if lactose intolerance is present or suspected
Fried or greasy foods that slow digestion
Hydration remains essential, but patients should sip water throughout the day rather than consuming large volumes with meals, which can increase stomach distension. Keeping a food diary for two to three weeks can help identify specific triggers, as individual tolerance varies. Gradual reintroduction of soluble fiber (such as oats or psyllium) after initial symptom control supports long-term digestive health and may help prevent constipation, which can contribute to bloating. For persistent symptoms, a short-term trial of a low-FODMAP diet under the guidance of a registered dietitian may be beneficial for some patients.
Beyond dietary modifications, several lifestyle strategies can help reduce bloating associated with GLP-1 medications. Eating slowly and chewing thoroughly—taking at least 20-30 minutes per meal—allows the satiety signals enhanced by these medications to register before overeating occurs. Rapid eating also causes aerophagia (swallowing air), which contributes to gas and bloating. Patients should put utensils down between bites and focus on the meal without distractions like television or smartphones.
Physical activity may help manage GLP-1 side effects. Gentle movement, particularly walking for 10-15 minutes after meals, may help reduce symptoms for some people by promoting movement of gas through the digestive system. While vigorous exercise immediately after eating may worsen discomfort, regular moderate-intensity activity—at least 150 minutes weekly per the U.S. Department of Health and Human Services Physical Activity Guidelines—supports overall gastrointestinal function and metabolic health. Yoga poses that gently compress the abdomen or stretching exercises may provide symptomatic relief for some patients.
Posture and timing considerations also matter. Remaining upright for at least two to three hours after eating prevents reflux and allows gravity to assist digestion. Patients should avoid lying down immediately after meals, which can trap gas and worsen bloating. Wearing loose-fitting clothing around the abdomen reduces external pressure that might exacerbate discomfort.
Stress management deserves attention, as the gut-brain axis significantly influences gastrointestinal symptoms. Chronic stress can alter gut motility and increase visceral hypersensitivity—heightened awareness of normal digestive sensations. Techniques such as deep breathing exercises, progressive muscle relaxation, or mindfulness meditation may reduce both stress and its gastrointestinal manifestations. Sleep quality also affects digestive function, making consistent sleep schedules (7-9 hours nightly) an important component of comprehensive symptom management.
When lifestyle and dietary modifications provide insufficient relief, several medical interventions may help manage GLP-1-related bloating. Over-the-counter simethicone (Gas-X, Mylicon) can reduce gas bubbles in the gastrointestinal tract, though evidence for its effectiveness is limited. Some patients find relief with digestive enzymes taken with meals, particularly those containing alpha-galactosidase (Beano) for carbohydrate digestion, though these have limited evidence and are not FDA-approved specifically for GLP-1 side effects.
For constipation-related bloating, which is common with these medications, polyethylene glycol (Miralax) or stool softeners may be helpful if not contraindicated for the individual patient.
Prescribers may consider dose adjustment strategies if bloating significantly impairs quality of life. Slowing the titration schedule—increasing doses more gradually than standard protocols—often improves gastrointestinal tolerance. For example, remaining at a lower dose for an additional two to four weeks before escalating may allow the digestive system to adapt. In some cases, switching to a different medication with a different pharmacokinetic profile may be appropriate, as individual responses vary.
Patients should contact their healthcare provider promptly if they experience:
Severe, persistent abdominal pain that worsens or differs from typical bloating
Inability to pass gas or have bowel movements (possible obstruction)
Persistent vomiting that prevents adequate hydration or medication adherence
Unintentional weight loss beyond expected therapeutic effects
Blood in stool or black, tarry stools
Fever accompanying gastrointestinal symptoms
Right upper quadrant pain or yellowing of skin/eyes (possible gallbladder disease)
Severe constipation with abdominal distension (possible ileus/obstruction)
Signs of dehydration (excessive thirst, dark urine, dizziness)
These symptoms may indicate complications such as pancreatitis, gallbladder disease, bowel obstruction, or acute kidney injury—all noted in FDA prescribing information as potential risks. GLP-1 medications are not recommended for patients with severe gastroparesis; patients with known motility disorders should discuss this with their healthcare provider. While bloating alone rarely necessitates medication discontinuation, persistent severe symptoms warrant thorough evaluation to exclude serious pathology and optimize the treatment regimen. Patients should never discontinue therapy without medical guidance, particularly when prescribed for diabetes management, as abrupt cessation can destabilize glycemic control.
For most patients, GLP-1-related bloating often improves after dose stabilization, though timelines vary considerably between individuals. Some patients experience resolution within four weeks while others may take several months to adapt. Clinical trial data suggest that gastrointestinal adverse effects typically peak during dose escalation and diminish with continued therapy at stable doses. Maintaining realistic expectations about this adaptation period helps patients persist through initial discomfort to achieve long-term metabolic benefits.
Sustainable long-term strategies involve integrating the dietary and lifestyle modifications discussed earlier into permanent habits rather than temporary measures. As tolerance improves, patients can gradually reintroduce higher-fiber foods and expand dietary variety while monitoring symptoms. Working with a registered dietitian familiar with these medications can provide personalized guidance that balances symptom management with nutritional adequacy—particularly important for patients on these medications long-term for obesity management.
Regular follow-up with prescribing clinicians remains essential for monitoring both therapeutic response and adverse effects. The American Diabetes Association recommends A1C testing every three months for patients not at goal or after therapy changes, and at least twice yearly for those meeting targets. These appointments provide opportunities to adjust management strategies, address emerging concerns, and reinforce adherence.
Some patients may experience persistent mild bloating that becomes their "new normal" on therapy. In these cases, the clinical decision involves weighing ongoing symptoms against therapeutic benefits—improved glycemic control, weight loss, and potential cardiovascular benefits demonstrated in specific medications. Semaglutide, liraglutide, and dulaglutide have demonstrated cardiovascular benefits in clinical trials, with Wegovy (semaglutide 2.4 mg) recently receiving FDA approval for cardiovascular risk reduction in adults with established cardiovascular disease and obesity. For patients with type 2 diabetes, these substantial benefits often justify tolerating mild persistent symptoms. However, quality of life considerations remain paramount, and alternative therapeutic options should be discussed if side effects significantly impair daily functioning despite comprehensive management strategies. Patient-centered decision-making, incorporating individual preferences and treatment goals, guides optimal long-term therapy management.
For most patients, GLP-1-related bloating improves after dose stabilization, typically within 4 weeks to several months. Symptoms usually peak during dose escalation and diminish with continued therapy at stable doses.
Avoid carbonated beverages, high-fat or fried foods, artificial sweeteners (especially sugar alcohols), and initially limit high-fiber foods like beans and cruciferous vegetables. Focus on lean proteins, well-cooked vegetables, and easily digestible carbohydrates.
Contact your healthcare provider immediately if you experience severe persistent abdominal pain, inability to pass gas or have bowel movements, persistent vomiting, blood in stool, fever with gastrointestinal symptoms, or signs of dehydration. These may indicate serious complications requiring prompt evaluation.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.