LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

How long for GLP-1 to kick in depends on what effect you're measuring and which medication you're taking. GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy), liraglutide (Victoza, Saxenda), and dulaglutide (Trulicity) work through multiple mechanisms to control blood glucose and reduce appetite. Initial effects on blood sugar often appear within 1-2 weeks, while appetite suppression may begin even sooner for some patients. However, reaching optimal therapeutic response typically requires 12-20 weeks as your dose gradually increases according to FDA-approved titration schedules. Understanding this timeline helps set realistic expectations as you begin treatment for type 2 diabetes or chronic weight management.
Quick Answer: GLP-1 medications typically show initial effects on blood glucose within 1-2 weeks and appetite suppression within days to weeks, but reaching full therapeutic response requires 12-20 weeks as doses gradually increase.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications originally developed for type 2 diabetes management. Some are now also FDA-approved for chronic weight management. These medications include semaglutide (Ozempic, Wegovy, Rybelsus), liraglutide (Victoza, Saxenda), and dulaglutide (Trulicity). Tirzepatide (Mounjaro, Zepbound) works through a related but distinct mechanism as a dual GIP/GLP-1 receptor agonist. These medications mimic naturally occurring hormones that your body produces in response to food intake.
The mechanism of action involves several physiological pathways. These medications bind to their respective receptors throughout the body, particularly in the pancreas, brain, and gastrointestinal tract. In the pancreas, they stimulate glucose-dependent insulin secretion, meaning insulin is released only when blood glucose levels are elevated, which reduces the risk of hypoglycemia compared to some other diabetes medications. Simultaneously, these medications suppress glucagon secretion, a hormone that raises blood glucose levels.
Beyond glycemic control, these medications initially slow gastric emptying, though this effect may diminish over time with long-acting formulations. They also act on appetite centers in the hypothalamus, reducing hunger signals. Most formulations are administered via subcutaneous injection (except oral semaglutide), typically weekly or daily depending on the specific medication, with dosing gradually increased over several weeks to minimize gastrointestinal side effects and optimize therapeutic response.
Importantly, these medications carry a boxed warning about the risk of thyroid C-cell tumors and are contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2).
The timeline for GLP-1 medications to "kick in" varies depending on which therapeutic effect you're measuring and the specific medication used. For blood glucose control in patients with type 2 diabetes, initial effects can often be observed within the first 1-2 weeks of treatment as the medication begins influencing insulin and glucagon secretion. However, reaching optimal glycemic control typically requires 12-16 weeks, particularly as the dose is gradually titrated upward according to FDA-approved protocols.
For appetite suppression and weight loss, the timeline differs somewhat. Some patients report reduced hunger and earlier satiety within the first week of treatment, though this varies considerably among individuals. Clinically significant weight loss—generally defined as 5% or more of baseline body weight—typically becomes apparent after reaching the maintenance dose, which may take 16-20 weeks depending on the specific medication and titration schedule.
It's important to understand that these medications follow a gradual dose escalation schedule to minimize side effects, particularly nausea and gastrointestinal discomfort. Most protocols start at a low dose and increase at regular intervals (typically every 4 weeks). This means you may not experience the full therapeutic effect until you reach the maintenance dose. The American Diabetes Association's Standards of Care emphasizes that patience during this titration period is essential for both efficacy and tolerability.
Steady-state drug levels—when the medication reaches consistent concentrations in your body—vary by product: liraglutide reaches steady state in approximately 2-3 days, while weekly formulations like semaglutide take 4-5 weeks and dulaglutide about 2-4 weeks at any given dose.
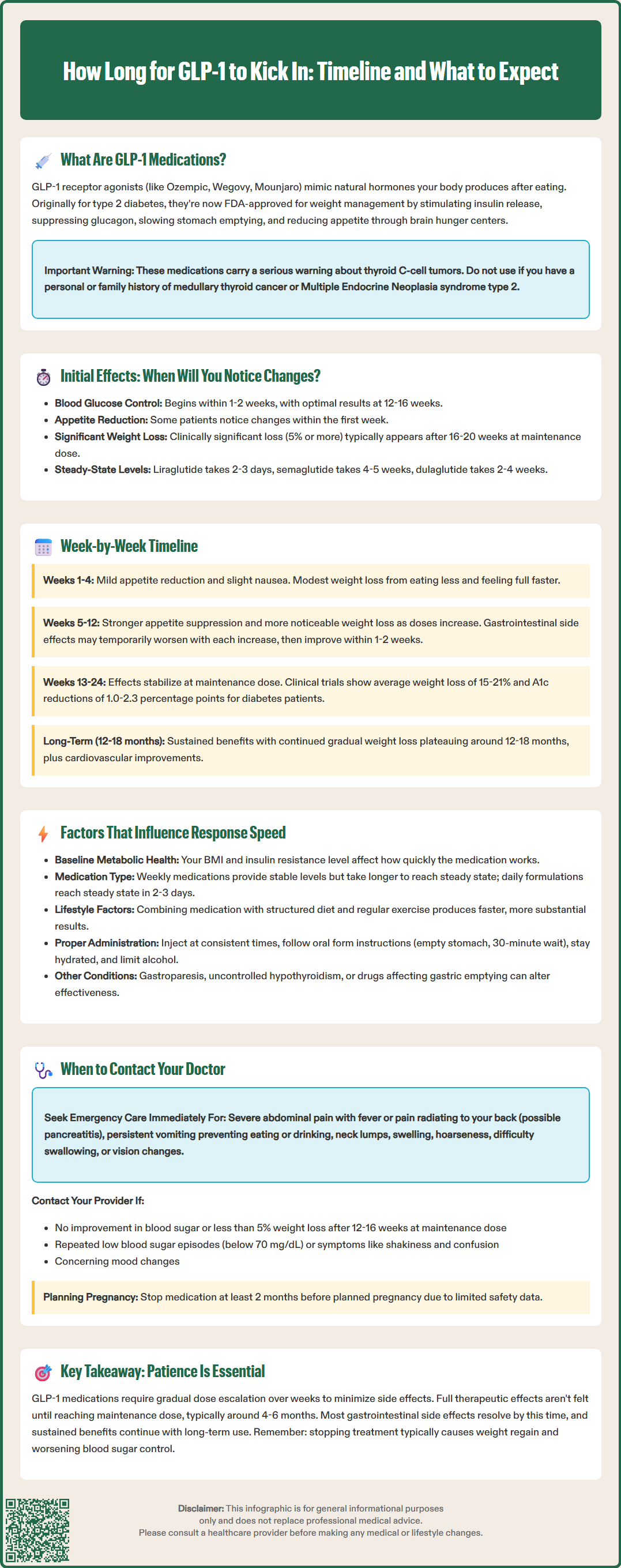
Weeks 1-4 (Initial Dose): During the first month, most patients begin at the lowest therapeutic dose. You may notice mild appetite reduction and slight nausea, particularly after meals. Blood glucose levels may begin to improve if you have diabetes. Weight loss during this period is typically modest, primarily due to reduced caloric intake. Some patients experience increased satiety, finding they feel full more quickly during meals. Gastrointestinal side effects like mild nausea, occasional bloating, or changes in bowel habits are common but usually manageable.
Weeks 5-12 (Dose Escalation): As your dose increases according to your prescribed titration schedule, therapeutic effects become more pronounced. Appetite suppression typically intensifies. Weight loss often becomes more noticeable during this phase, though the amount varies by individual and medication. For diabetes management, blood glucose control continues to improve, though the full effect on hemoglobin A1c won't be captured until your next quarterly lab work. Gastrointestinal side effects may temporarily worsen with each dose increase but generally improve within 1-2 weeks as your body adjusts.
Weeks 13-24 (Approaching or Reaching Maintenance Dose): As you approach or reach your maintenance dose (timing varies by product—Wegovy typically by week 17, others on different schedules), the medication's effects stabilize. Weight loss typically continues, with clinical trials showing that semaglutide 2.4 mg (Wegovy) produces average weight loss of approximately 15% by week 68, while tirzepatide (Zepbound) has demonstrated weight loss of approximately 15-21% across different doses by week 72. For diabetes patients, A1c reductions of approximately 1.0-1.5 percentage points are common with GLP-1 receptor agonists, while tirzepatide has shown reductions of up to 2.0-2.3 percentage points in clinical trials. Most gastrointestinal side effects have resolved or become minimal by this stage.
Beyond 6 Months: Long-term studies demonstrate that these medications continue to provide sustained benefits with ongoing treatment. Weight loss may continue gradually before plateauing, typically around 12-18 months. Cardiovascular benefits, including blood pressure reduction and improved lipid profiles, become more apparent with extended use. Clinical trials have shown that discontinuing treatment typically results in gradual weight regain and worsening glycemic control, underscoring that these are chronic disease management tools rather than short-term interventions.
Individual Metabolic Factors: Your baseline metabolic health significantly influences response time. Patients with higher baseline body mass index (BMI) or more severe insulin resistance may experience different response patterns compared to those with milder metabolic dysfunction. While genetic variations in receptor expression may theoretically affect response, this is not currently used in clinical decision-making. Response may vary across age groups, though evidence for consistent age-related differences in onset of action is limited.
Medication-Specific Characteristics: Different formulations have varying pharmacokinetic properties that affect onset of action. Weekly medications like semaglutide and dulaglutide have longer half-lives, taking longer to reach steady-state concentrations but offering more stable drug levels throughout the week. Daily formulations like liraglutide reach steady state more quickly—typically within 2-3 days—but require consistent daily administration. Tirzepatide, which activates both GLP-1 and GIP receptors, may produce different effects compared to pure GLP-1 agonists. Oral semaglutide (Rybelsus) requires specific administration (taking on an empty stomach with water and waiting 30 minutes before eating) to ensure proper absorption.
Lifestyle and Adherence Factors: Your dietary habits and physical activity level can significantly impact how quickly you notice effects. Patients who combine medication with structured dietary changes and regular exercise typically experience faster and more substantial results. Proper injection technique and consistent timing also matter—injecting at the same time each week (for weekly formulations) helps maintain stable drug levels. Adequate hydration is important for managing side effects. Alcohol consumption may interfere with glycemic control and can exacerbate gastrointestinal side effects.
Concurrent Medications and Medical Conditions: Other medications can influence effectiveness. For instance, medications that speed gastric emptying may partially counteract some effects, while those that slow it may intensify side effects. Severe gastrointestinal disease, particularly gastroparesis, may alter both efficacy and tolerability and requires careful consideration. Thyroid function also plays a role in metabolic response, and uncontrolled hypothyroidism may blunt weight loss effects. Patients taking multiple medications for diabetes should work closely with their healthcare provider to optimize the overall regimen, as dose adjustments of other agents may be necessary as these medications take effect.
Inadequate Therapeutic Response: Contact your healthcare provider if you experience minimal or no improvement in target outcomes after reaching your maintenance dose for 12-16 weeks. For diabetes management, this means persistently elevated blood glucose readings or an A1c that hasn't decreased significantly. For weight management, lack of at least 5% weight loss by 12 weeks at the maintenance dose warrants discussion about alternative strategies or dose optimization. However, remember that response varies, and your provider will consider multiple factors including adherence, lifestyle modifications, and individual metabolic characteristics before making changes.
Severe or Persistent Side Effects: While mild gastrointestinal symptoms are expected initially, certain symptoms require prompt medical attention. If you experience severe, persistent nausea or vomiting that prevents adequate fluid or food intake, contact your provider. For severe abdominal pain, particularly if accompanied by fever or radiating to the back, stop the medication immediately and seek emergency care, as this may indicate pancreatitis—a rare but serious adverse effect. Persistent diarrhea or constipation lasting more than a few days should be reported. Signs of gallbladder problems, including right upper abdominal pain, jaundice, or clay-colored stools, warrant urgent assessment, as these medications can increase gallstone risk, particularly during rapid weight loss. Rare cases of intestinal obstruction have been reported with some agents.
Hypoglycemia Symptoms: If you're taking these medications alongside insulin or sulfonylureas, contact your provider if you experience repeated episodes of low blood glucose (below 70 mg/dL) or symptoms such as shakiness, sweating, confusion, or rapid heartbeat. Dose adjustments of your other diabetes medications may be necessary as your glycemic control improves. Even without concurrent medications, unexplained hypoglycemia symptoms should be reported and investigated.
Other Warning Signs: Seek immediate medical attention for symptoms of thyroid tumors, including a lump or swelling in the neck, hoarseness, difficulty swallowing, or shortness of breath. These medications are contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2. Changes in vision should be evaluated, particularly in patients with pre-existing diabetic retinopathy. While the FDA continues to monitor reports of suicidal thoughts, their 2024 safety communication found no clear evidence linking these medications to suicidal ideation; nevertheless, report any concerning mood changes promptly. If you're planning pregnancy, contact your provider well in advance, as these medications should be discontinued (semaglutide at least 2 months before planned conception) due to limited safety data in pregnancy. Regular follow-up appointments are essential for monitoring response, adjusting doses, and screening for potential complications throughout your treatment course.
GLP-1 medications typically begin lowering blood glucose within 1-2 weeks of starting treatment, though optimal glycemic control usually requires 12-16 weeks as the dose is gradually increased. Hemoglobin A1c reductions of 1.0-2.3 percentage points are commonly seen in clinical trials.
Some patients report reduced hunger and earlier satiety within the first week of GLP-1 treatment, though individual response varies considerably. Appetite suppression typically intensifies during weeks 5-12 as your dose increases according to the prescribed titration schedule.
Contact your healthcare provider if you experience minimal improvement after reaching maintenance dose for 12-16 weeks, including persistently elevated blood glucose or lack of at least 5% body weight reduction. Your provider will evaluate adherence, lifestyle factors, and consider dose optimization or alternative strategies.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.