LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
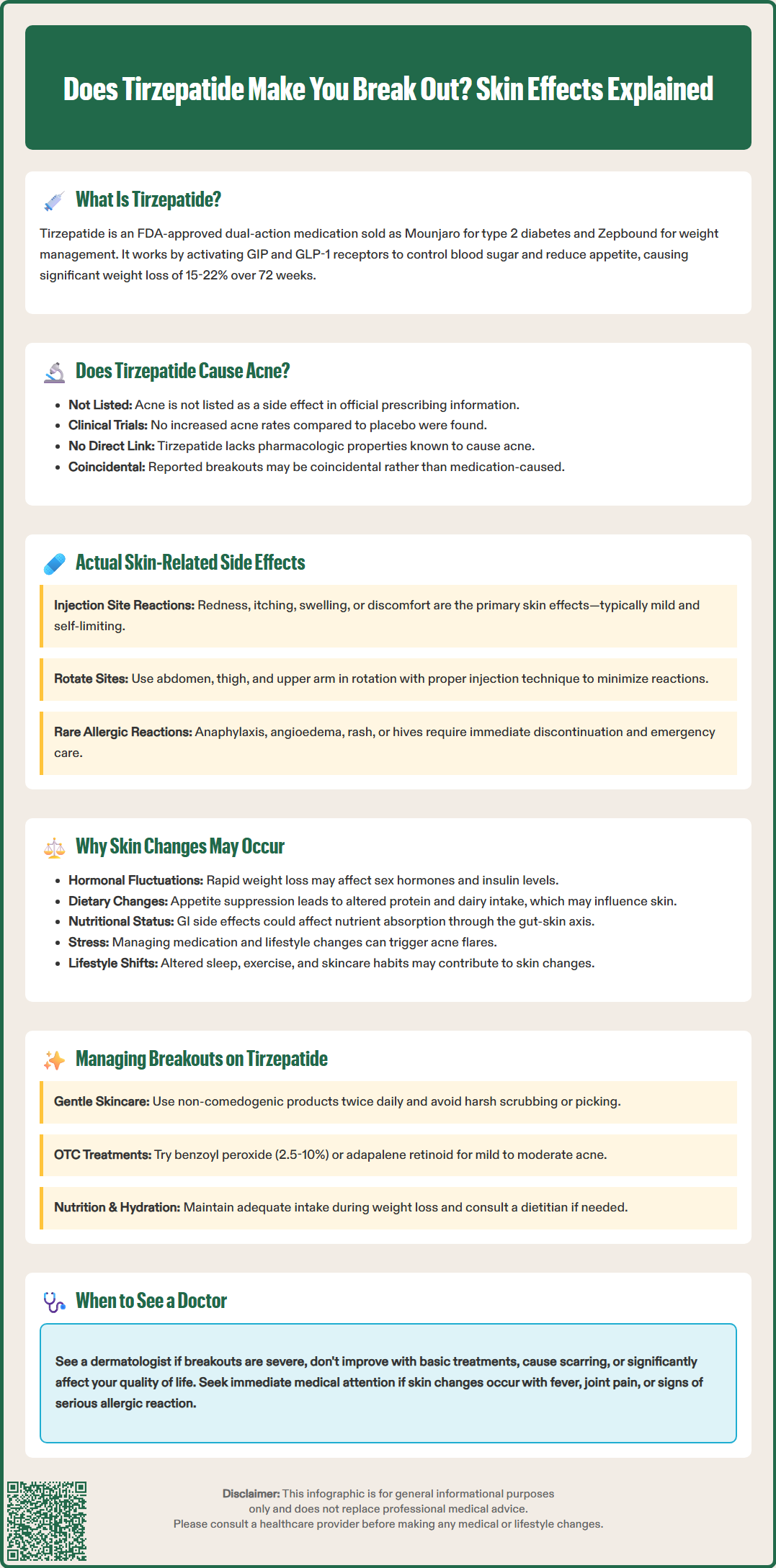
Does tirzepatide make you break out? This question concerns many patients starting this dual GIP/GLP-1 receptor agonist for type 2 diabetes or weight management. Tirzepatide, marketed as Mounjaro and Zepbound, is FDA-approved for improving glycemic control and supporting weight loss. While the medication offers significant metabolic benefits, patients sometimes report skin changes during treatment. Understanding the relationship between tirzepatide and skin health helps clinicians provide evidence-based guidance. This article examines whether tirzepatide directly causes acne, reviews documented dermatologic effects, and offers practical management strategies for patients experiencing breakouts during therapy.
Quick Answer: Acne is not listed as an adverse reaction in FDA prescribing information for tirzepatide, and clinical trials did not identify breakouts as significant adverse events.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Marketed under the brand names Mounjaro (for diabetes) and Zepbound (for weight management), tirzepatide represents a newer incretin-based therapy for metabolic conditions.
The medication works through a dual mechanism of action. By activating both GIP and GLP-1 receptors, tirzepatide enhances insulin secretion in a glucose-dependent manner, suppresses glucagon release, slows gastric emptying, and reduces appetite. This combined approach leads to improved glycemic control and substantial weight loss in clinical trials. The FDA-approved dosing begins at 2.5 mg subcutaneously once weekly, with gradual titration up to a maximum of 15 mg weekly based on therapeutic response and tolerability.
Clinical trials have demonstrated that tirzepatide significantly reduces hemoglobin A1c levels in patients with type 2 diabetes, with many achieving target glycemic goals. In weight management studies, patients experienced average weight reductions of 15-22% of body weight over 72 weeks. Zepbound is indicated for adults with a BMI ≥30 kg/m² or ≥27 kg/m² with at least one weight-related comorbidity.
The American Diabetes Association recognizes GLP-1 receptor agonists and dual GIP/GLP-1 receptor agonists as preferred agents for many patients with type 2 diabetes, particularly those with established cardiovascular disease, heart failure, or chronic kidney disease, where these agents may be used independent of metformin therapy. Unlike some other GLP-1 receptor agonists, tirzepatide does not yet have established cardiovascular outcome benefits, with studies ongoing.
As with any medication, understanding the full safety profile is essential for both prescribers and patients. While tirzepatide has shown favorable efficacy outcomes, patients frequently inquire about potential dermatologic effects, including whether the medication can cause acne or skin breakouts.
Acne is not listed as an adverse reaction in the US Prescribing Information for either Mounjaro or Zepbound. The pivotal SURPASS clinical trial program for diabetes and the SURMOUNT trials for weight management did not identify acne or acneiform eruptions as significant adverse events occurring at rates higher than placebo.
However, anecdotal reports from patients and online forums suggest that some individuals experience skin changes, including breakouts, after initiating tirzepatide therapy. It is important to distinguish between true causation and coincidental association. Many factors can contribute to acne development, and the temporal relationship between starting a medication and experiencing skin changes does not necessarily indicate a direct pharmacologic effect.
The mechanism by which tirzepatide might theoretically influence skin health remains unclear. Unlike some medications with known acnegenic properties—such as corticosteroids, lithium, or certain anticonvulsants—tirzepatide does not have obvious pharmacologic properties that would directly promote acne formation. While limited research exists on the effects of GLP-1 receptor agonists on skin physiology, there is no established evidence that these medications directly alter sebum production or other key factors in acne pathogenesis.
Clinicians should approach patient reports of breakouts with tirzepatide by conducting a thorough assessment. This includes evaluating the timing of symptom onset, characterizing the skin changes (true acne versus other dermatologic conditions), reviewing concurrent medications and skincare products, and considering alternative explanations. While individual susceptibility to medication-related skin changes varies, the current evidence does not support a direct causal relationship between tirzepatide and acne development.
The most commonly reported adverse effects of tirzepatide involve the gastrointestinal system rather than the skin. According to FDA labeling, the most frequent side effects include nausea (occurring in 12-29% of patients depending on dose), diarrhea (13-23%), vomiting (6-13%), constipation (6-11%), and abdominal pain (6-9%). These rates vary by dose and between diabetes and obesity populations. These gastrointestinal effects are typically mild to moderate in severity and tend to diminish over time as patients develop tolerance.
Regarding dermatologic effects specifically documented in clinical trials, injection site reactions are the primary skin-related adverse events associated with tirzepatide. These reactions may include erythema (redness), pruritus (itching), swelling, or discomfort at the subcutaneous injection site. Such reactions are generally mild and self-limiting, resolving within a few days without specific intervention. Patients can minimize injection site reactions by rotating injection sites among the abdomen, thigh, and upper arm (upper arm injections may require administration by another person per Instructions for Use), and by ensuring proper injection technique.
Other skin-related considerations include potential allergic reactions, though these are rare. Hypersensitivity reactions can manifest as rash, urticaria (hives), or pruritus. Serious hypersensitivity reactions, including anaphylaxis and angioedema, have been reported with GLP-1 receptor agonists, though they remain uncommon. Patients experiencing signs of serious allergic reactions—such as difficulty breathing, facial swelling, or widespread rash—should discontinue tirzepatide immediately and seek emergency medical attention.
It is worth noting that rapid weight loss itself, which commonly occurs with tirzepatide therapy, can affect skin health in various ways. Significant weight reduction may lead to changes in skin texture, elasticity, and appearance. Additionally, nutritional deficiencies that sometimes accompany rapid weight loss or reduced caloric intake could theoretically impact skin health, though this would be an indirect rather than direct medication effect.
Several hypothetical explanations exist for why some patients report skin breakouts or changes while taking tirzepatide, even in the absence of a direct pharmacologic mechanism. Understanding these factors helps clinicians provide appropriate counseling and management strategies.
Hormonal fluctuations related to weight loss may potentially contribute. Adipose tissue is metabolically active and influences hormone levels, particularly sex hormones and insulin. Rapid weight loss could theoretically disrupt hormonal balance in ways that might influence skin health, though this is not established as a direct effect of tirzepatide. Some patients may experience changes in menstrual patterns during significant weight loss, which could coincidentally affect skin appearance.
Dietary modifications often accompany tirzepatide therapy. The medication's appetite-suppressing effects lead many patients to alter their eating patterns substantially. Some patients may adopt high-protein diets or change dairy consumption patterns. The American Academy of Dermatology notes that the relationship between diet and acne is complex, with limited evidence suggesting potential associations between certain dietary factors and acne in some individuals, though causality remains unclear.
Gastrointestinal effects of tirzepatide may indirectly impact overall health. Nausea and altered gut motility are common side effects that could affect nutritional status. While the gut-skin axis is an emerging area of research, direct connections between tirzepatide-induced GI effects and skin changes remain speculative and not established in clinical studies.
Stress and lifestyle factors should not be overlooked. Starting a new medication, managing diabetes or weight loss, and experiencing gastrointestinal side effects can be stressful. Psychological stress is a well-established trigger for acne flares and other skin conditions. Furthermore, changes in sleep patterns, exercise routines, or skincare habits during treatment may contribute to skin changes that patients attribute to the medication itself.
For patients experiencing skin breakouts while taking tirzepatide, a systematic approach to management is appropriate. First, clinicians should conduct a thorough assessment to characterize the skin changes and identify potential contributing factors. This includes reviewing the patient's complete medication list, skincare routine, dietary changes, and any recent life stressors. Distinguishing true acne vulgaris from other conditions such as rosacea, folliculitis, or allergic reactions is essential for appropriate treatment.
Basic skincare recommendations form the foundation of management. Patients should use gentle, non-comedogenic cleansers twice daily and avoid harsh scrubbing or over-washing, which can exacerbate inflammation. Oil-free, non-comedogenic moisturizers help maintain skin barrier function without clogging pores. Patients should be advised to avoid touching or picking at their face, which can worsen inflammation and increase infection risk.
Topical treatments for mild to moderate acne include benzoyl peroxide (2.5-10%), which has antibacterial and anti-inflammatory properties, and topical retinoids such as adapalene (available over-the-counter at 0.1% concentration), which normalize follicular keratinization. Topical retinoids are contraindicated during pregnancy due to potential teratogenic effects. Salicylic acid-containing products can help with comedonal acne. For inflammatory acne, topical antibiotics like clindamycin may be appropriate, though these should be combined with benzoyl peroxide to reduce antibiotic resistance and limited in duration.
Nutritional optimization deserves attention, particularly in patients experiencing significant weight loss. Ensuring adequate intake of essential nutrients supports skin health. Patients should maintain adequate hydration and consider consultation with a registered dietitian to ensure nutritional adequacy during weight loss. Supplements should be used cautiously—avoid high-dose vitamin A supplements due to toxicity risk, and do not exceed recommended daily allowances for zinc without medical supervision, as excessive zinc can lead to copper deficiency.
When to seek dermatologic consultation: Patients should be referred to dermatology if breakouts are severe, persistent despite basic interventions, causing scarring, or significantly impacting quality of life. Dermatologists can provide prescription-strength treatments, including oral antibiotics, hormonal therapies (for appropriate candidates), or isotretinoin for severe cases. Isotretinoin requires enrollment in the FDA's iPLEDGE program due to its teratogenic potential and is absolutely contraindicated during pregnancy. Importantly, if skin changes are accompanied by systemic symptoms such as fever, joint pain, or signs of serious allergic reaction, prompt medical evaluation is warranted. The decision to continue or discontinue tirzepatide should be individualized, weighing the medication's metabolic benefits against the severity and impact of skin symptoms.
No, acne is not listed as an adverse reaction in FDA prescribing information for Mounjaro or Zepbound, and clinical trials did not identify acne as occurring at rates higher than placebo.
The primary skin-related effects are mild injection site reactions including redness, itching, and swelling at the subcutaneous injection site, which typically resolve within a few days.
Do not discontinue tirzepatide without consulting your healthcare provider. The decision should be individualized, weighing metabolic benefits against skin symptoms, and many breakouts can be managed with appropriate skincare or dermatologic treatment.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.