LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

How long does it take for GLP-1 to leave your system? The answer depends on which specific medication you're taking. GLP-1 receptor agonists—medications used for type 2 diabetes and weight management—have elimination times ranging from hours to several weeks after your last dose. Short-acting formulations like exenatide (Byetta) clear within 12–24 hours, while long-acting options such as semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound) can take 4–5 weeks to fully eliminate. Understanding your medication's half-life and clearance timeline is essential for managing side effects, planning procedures, and transitioning to alternative therapies.
Quick Answer: GLP-1 receptor agonists take anywhere from 12 hours to 10 weeks to leave your system, depending on the specific medication and its half-life.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily used to manage type 2 diabetes and, more recently, for chronic weight management. These medications mimic the action of naturally occurring GLP-1, an incretin hormone produced in the intestines in response to food intake. Understanding how these drugs work provides essential context for their elimination from the body.
GLP-1 receptor agonists bind to and activate GLP-1 receptors located throughout the body, particularly in pancreatic beta cells, the gastrointestinal tract, and the central nervous system. In the pancreas, activation stimulates glucose-dependent insulin secretion, meaning insulin is released only when blood glucose levels are elevated, which reduces the risk of hypoglycemia compared to some other diabetes medications. Simultaneously, these medications suppress glucagon secretion from pancreatic alpha cells, further contributing to improved glycemic control.
Beyond glycemic effects, GLP-1 receptor agonists slow gastric emptying, which prolongs the sensation of fullness after meals and contributes to reduced caloric intake. Central nervous system effects include appetite suppression through actions on hypothalamic centers that regulate hunger and satiety. These combined mechanisms explain both the glucose-lowering and weight-reducing properties of this medication class.
Currently available GLP-1 receptor agonists in the United States include exenatide (Byetta, Bydureon BCise), liraglutide (Victoza, Saxenda), dulaglutide (Trulicity), semaglutide (Ozempic, Wegovy, Rybelsus), and tirzepatide (Mounjaro, Zepbound), though tirzepatide is technically a dual GIP/GLP-1 receptor agonist. Each formulation has distinct pharmacokinetic properties that determine how long the medication remains active in the body after administration or discontinuation.
Importantly, most GLP-1 receptor agonists carry a boxed warning about the risk of thyroid C-cell tumors and are contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2).
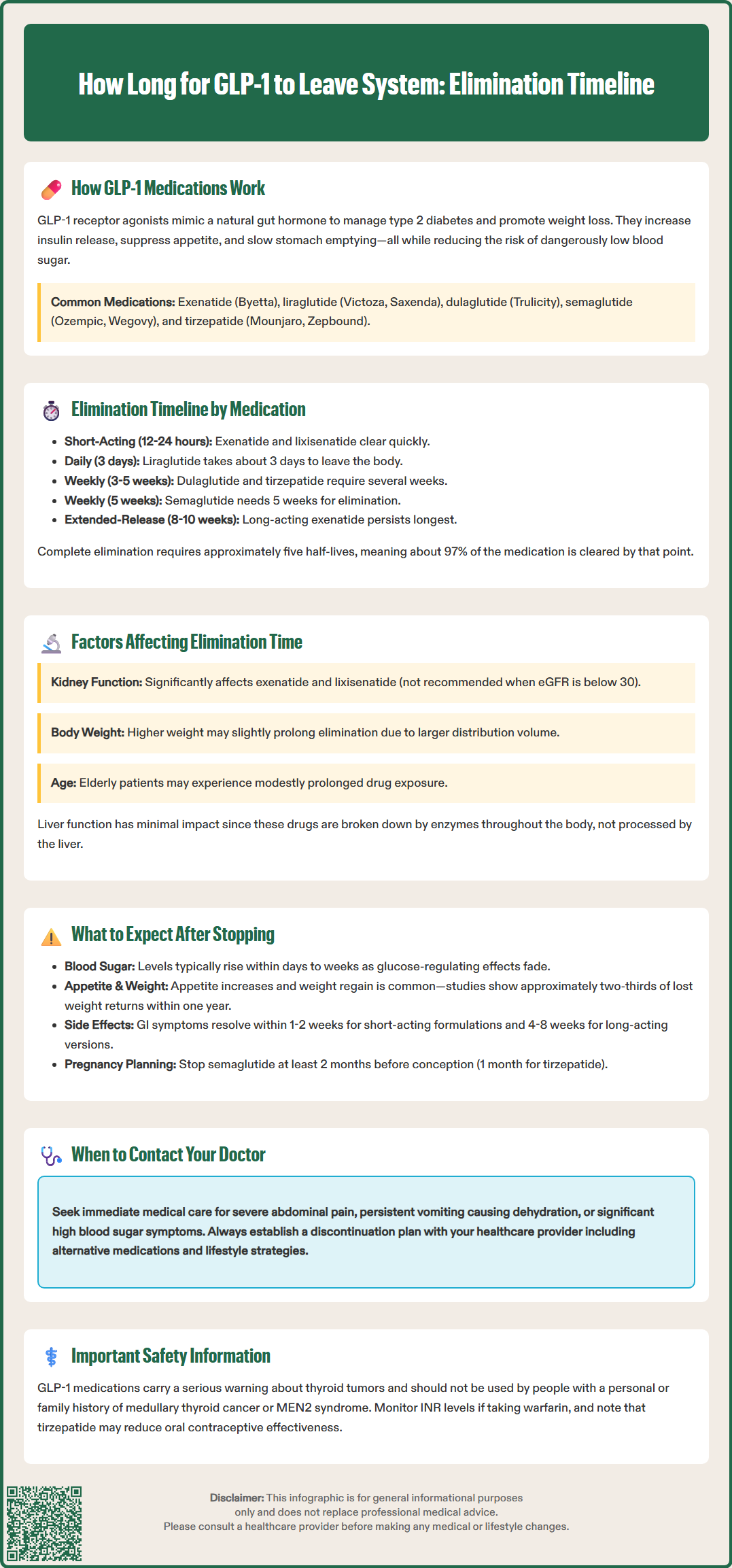
The half-life of a medication—the time required for the body to eliminate half of the drug's concentration—is the primary determinant of how long a GLP-1 receptor agonist remains in your system. Different formulations within this class have dramatically different half-lives, ranging from hours to days, which directly impacts their dosing frequency and elimination timeline.
Short-acting GLP-1 receptor agonists include immediate-release exenatide (Byetta) with a half-life of approximately 2.4 hours. Lixisenatide (Adlyxin), which is FDA-approved but no longer marketed in the US, has a half-life of about 3 hours. These medications are administered once or twice daily and are generally eliminated from the system within 12-24 hours after the last dose. Liraglutide (Victoza, Saxenda), administered once daily, has an intermediate half-life of approximately 13 hours and typically clears from the body within 3 days (about 5 half-lives) of discontinuation.
Long-acting formulations have substantially longer half-lives due to modifications that slow absorption and degradation. Extended-release exenatide (Bydureon BCise) has an apparent terminal half-life of approximately 2 weeks due to its depot formulation, with drug concentrations potentially persisting for 8-10 weeks after discontinuation. Dulaglutide (Trulicity), administered weekly, has a half-life of approximately 5 days, meaning it takes roughly 3-4 weeks (about 5 half-lives) for 97% elimination. Semaglutide (Ozempic, Wegovy) has a half-life of approximately 7 days, requiring approximately 5 weeks for 97% clearance from the body after the final injection. Tirzepatide (Mounjaro, Zepbound) has a half-life of approximately 5 days, with elimination taking about 4-5 weeks after the last dose.
As a general principle, it takes approximately five half-lives for a medication to be considered essentially eliminated from the body (representing about 97% clearance). The oral formulation of semaglutide (Rybelsus) follows similar elimination kinetics to the injectable form despite the different route of administration. Patients should understand that even after symptoms or effects diminish, measurable drug levels may persist for several weeks depending on the specific formulation used.
While the inherent pharmacokinetic properties of each GLP-1 receptor agonist largely determine elimination time, several patient-specific factors can influence how quickly or slowly these medications clear from the body. Understanding these variables helps clinicians and patients anticipate individual variation in drug clearance.
Renal function significantly affects elimination for certain GLP-1 receptor agonists. Exenatide and lixisenatide are primarily cleared through the kidneys, while liraglutide, dulaglutide, semaglutide, and tirzepatide undergo proteolytic degradation throughout the body with minimal renal excretion of intact drug. According to FDA labeling, exenatide is not recommended in patients with estimated glomerular filtration rate (eGFR) below 30 mL/min/1.73 m². Liraglutide, dulaglutide, semaglutide, and tirzepatide do not require dose adjustment based on renal function, though patients with impaired kidney function should be monitored for potential dehydration-related renal events.
Body weight and composition can influence the volume of distribution for GLP-1 medications, potentially affecting elimination kinetics. Patients with higher body mass may have larger volumes of distribution, which could theoretically prolong elimination time, though this effect is generally modest compared to other factors. Age-related changes in kidney function and body composition mean that elderly patients may experience slightly prolonged drug exposure, though specific dose adjustments based solely on age are typically not required.
Hepatic function plays a minimal role in GLP-1 elimination, as these medications are primarily degraded by proteolytic enzymes throughout the body rather than hepatic metabolism. According to FDA labeling, no dose adjustments are generally required for patients with hepatic impairment. Drug-drug interactions are uncommon with GLP-1 receptor agonists because they are not metabolized by cytochrome P450 enzymes. However, their effect on gastric emptying can alter the absorption of oral medications administered concurrently. For example, tirzepatide may reduce the effectiveness of oral contraceptives, and patients taking warfarin with any GLP-1 receptor agonist should consider more frequent INR monitoring when starting or stopping therapy.
Patients should inform their healthcare providers about any kidney disease, significant weight changes, or other medications they are taking, as these factors may influence both the therapeutic effects and elimination timeline of GLP-1 receptor agonists.
Discontinuing GLP-1 receptor agonist therapy leads to predictable physiological changes as drug levels decline and the pharmacological effects diminish. The timeline and magnitude of these changes depend on the specific medication, duration of treatment, and individual patient factors. Understanding what to expect can help patients and clinicians manage the transition appropriately.
Glycemic control changes typically occur within days to weeks after stopping GLP-1 therapy. As drug levels fall, the glucose-dependent insulin secretion and glucagon suppression effects wane, often resulting in rising blood glucose levels. For patients using GLP-1 medications for type 2 diabetes, hemoglobin A1c may increase after discontinuation if no alternative therapy is initiated, with the magnitude varying based on individual factors and baseline therapy. Patients should increase home glucose monitoring frequency during the transition period and work with their healthcare provider to adjust or initiate alternative diabetes medications as needed. The American Diabetes Association recommends reassessing glycemic control within 3 months of any significant medication change.
Appetite and weight changes are among the most noticeable effects after stopping GLP-1 therapy. As gastric emptying returns to normal and central appetite suppression diminishes, patients typically experience increased hunger and may resume previous eating patterns. Clinical trial data from the STEP 1 extension study showed that after discontinuing semaglutide 2.4 mg, approximately two-thirds of weight loss was regained within one year. This is not a failure of willpower but rather reflects the medication's role in appetite regulation and the body's metabolic adaptation.
Gastrointestinal symptoms that some patients experience while on GLP-1 therapy—such as nausea, reduced appetite, or altered bowel habits—generally resolve as the medication clears from the system, typically within 1-2 weeks for short-acting formulations and within 4-8 weeks for long-acting preparations, corresponding to their elimination timelines.
Special considerations include pregnancy planning and perioperative management. For patients planning pregnancy, semaglutide should be discontinued at least 2 months before a planned pregnancy due to the long half-life, while tirzepatide may persist for approximately 1 month. Patients should discuss perioperative management with their healthcare team, as these medications can affect gastric emptying and may need to be temporarily discontinued before certain procedures.
Patients should seek immediate medical attention for severe abdominal pain (possible pancreatitis), persistent vomiting leading to dehydration, or symptoms of significant hyperglycemia. A structured discontinuation plan should include strategies for maintaining glycemic control and weight management, such as initiating alternative medications, intensifying lifestyle modifications, and scheduling appropriate follow-up appointments.
Semaglutide (Ozempic, Wegovy) has a half-life of approximately 7 days and takes about 5 weeks (five half-lives) for 97% clearance from the body after the final injection.
Yes, short-acting GLP-1 medications like exenatide (Byetta) with a 2.4-hour half-life clear within 12–24 hours, while long-acting formulations can take 4–10 weeks to fully eliminate.
Kidney function significantly affects exenatide and lixisenatide clearance, but medications like semaglutide, tirzepatide, dulaglutide, and liraglutide undergo proteolytic degradation and do not require renal dose adjustments.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.