LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Many patients with fatty liver disease wonder whether weight loss injections are safe and effective for their condition. Fatty liver disease, now termed metabolic dysfunction-associated steatotic liver disease (MASLD), affects approximately 25% of US adults and is closely linked to obesity. Weight loss of 7-10% can significantly improve liver health, but achieving this through lifestyle changes alone proves challenging. GLP-1 receptor agonists like semaglutide (Wegovy, Ozempic) and tirzepatide (Zepbound, Mounjaro) offer substantial weight reduction and may provide specific benefits for liver health. Understanding the safety, efficacy, and monitoring requirements of these medications in fatty liver disease is essential for informed treatment decisions.
Quick Answer: Weight loss injections, particularly GLP-1 receptor agonists, are generally safe for patients with fatty liver disease and may offer specific hepatic benefits beyond weight reduction.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Fatty liver disease, medically termed hepatic steatosis, occurs when excess fat accumulates in liver cells. The condition exists in two primary forms: metabolic dysfunction-associated steatotic liver disease (MASLD, formerly known as non-alcoholic fatty liver disease or NAFLD), which affects individuals who consume little to no alcohol, and alcoholic fatty liver disease. MASLD has become increasingly prevalent in the United States, affecting approximately 25% of adults, with rates closely paralleling the obesity epidemic.
The spectrum of MASLD ranges from simple steatosis—where fat accumulation causes minimal inflammation—to metabolic dysfunction-associated steatohepatitis (MASH, formerly NASH), characterized by inflammation and liver cell damage that can progress to cirrhosis. Many patients remain asymptomatic until advanced disease develops, making incidental diagnosis through imaging or elevated liver enzymes common during routine health assessments.
Weight loss represents the cornerstone of MASLD management. Clinical evidence demonstrates that losing 7-10% of body weight can significantly reduce liver fat content, improve inflammation markers, and potentially reverse early fibrosis. However, achieving and maintaining this degree of weight loss through lifestyle modification alone proves challenging for many patients. This difficulty has generated considerable interest in pharmacological weight loss interventions, including injectable medications.
The emergence of highly effective weight loss injections, particularly GLP-1 receptor agonists, has transformed obesity treatment. These medications offer substantial weight reduction—often 15-20% of body weight—raising important questions about their safety and efficacy specifically in patients with fatty liver disease. While these medications are FDA-approved for obesity (BMI ≥30 kg/m² or ≥27 kg/m² with weight-related complications) and/or type 2 diabetes, they are not specifically approved for MASLD/MASH treatment. Understanding the relationship between these treatments and liver health is essential for both patients and healthcare providers making informed treatment decisions.
Weight loss injections primarily consist of glucagon-like peptide-1 (GLP-1) receptor agonists, including semaglutide (marketed as Wegovy for weight management and Ozempic for diabetes) and tirzepatide (Zepbound for weight management, Mounjaro for diabetes). These medications mimic naturally occurring hormones that regulate appetite, glucose metabolism, and energy balance.
The mechanism of action involves multiple physiological pathways. GLP-1 receptor agonists bind to receptors in the brain's appetite centers, particularly the hypothalamus, reducing hunger signals and increasing satiety after meals. This leads to decreased caloric intake without the conscious effort typically required for dietary restriction. Additionally, these medications slow gastric emptying, prolonging the feeling of fullness after eating and reducing the frequency of hunger between meals.
Beyond appetite regulation, GLP-1 receptor agonists improve glucose homeostasis by enhancing insulin secretion in response to meals and suppressing inappropriate glucagon release. This glucose-dependent mechanism means insulin secretion occurs primarily when blood sugar is elevated, reducing hypoglycemia risk compared to some other diabetes medications. When used with insulin or sulfonylureas, dose adjustments of these medications may be needed to prevent hypoglycemia.
Tirzepatide represents a dual agonist, activating both GLP-1 and glucose-dependent insulinotropic polypeptide (GIP) receptors, which may explain its particularly robust weight loss effects. Clinical trials demonstrate average weight loss of 15-22% with tirzepatide compared to 10-15% with semaglutide, though individual responses vary considerably.
These medications require subcutaneous injection, typically weekly, with gradual dose escalation to minimize gastrointestinal side effects. Wegovy (semaglutide) starts at 0.25 mg weekly, increasing monthly to a target dose of 2.4 mg. Zepbound (tirzepatide) begins at 2.5 mg weekly, with monthly increases to a maintenance dose of 5, 10, or 15 mg. Due to its effects on gastric emptying, tirzepatide may reduce the effectiveness of oral contraceptives; backup contraception is recommended during initiation and dose escalation periods. Importantly, GLP-1 and GIP agonists should not be used concurrently.
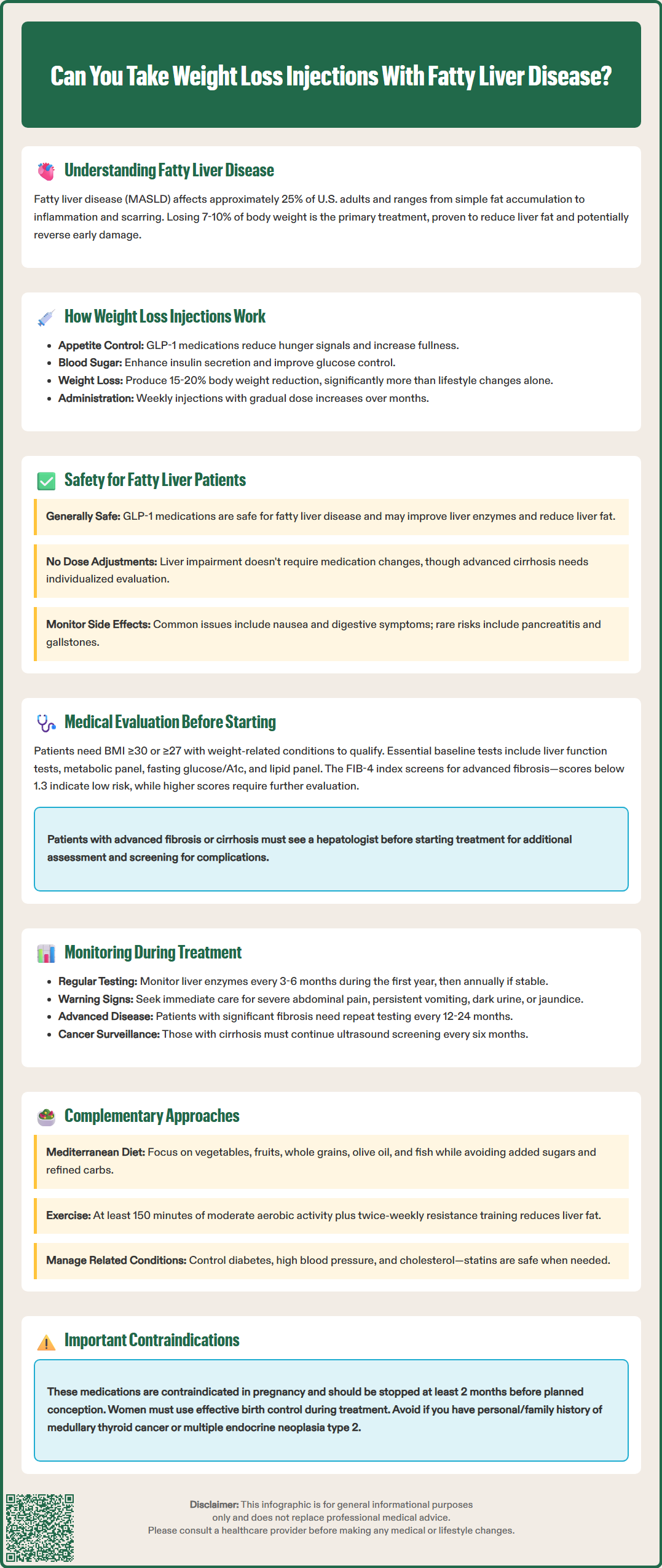
Current evidence suggests that GLP-1 receptor agonists are not only safe for patients with fatty liver disease but may offer specific hepatic benefits beyond weight loss alone. Multiple clinical trials have demonstrated improvements in liver enzyme levels, hepatic fat content, and markers of liver inflammation in patients treated with these medications. Importantly, there is no established contraindication to using weight loss injections in patients with MASLD or MASH.
A pivotal consideration is that the weight loss achieved with these medications directly addresses the primary pathophysiological driver of MASLD. Studies using magnetic resonance imaging and liver biopsy have shown significant reductions in hepatic steatosis with GLP-1 receptor agonist therapy. Research suggests these medications may have beneficial effects on liver inflammation, though evidence for direct anti-fibrotic effects remains preliminary.
The FDA-approved labeling for semaglutide and tirzepatide does not list liver disease as a contraindication, and no dose adjustments are required for hepatic impairment. However, patients with decompensated cirrhosis—characterized by complications such as ascites, variceal bleeding, or hepatic encephalopathy—require careful individualized assessment, as clinical trial data in this population remains limited. For patients with compensated liver disease, including those with biopsy-proven MASH, these medications appear safe and potentially beneficial.
Common adverse effects include gastrointestinal symptoms (nausea, diarrhea, constipation), which typically improve with continued use. Rare but serious risks include pancreatitis, gallbladder disease (including gallstones and cholecystitis), and potential thyroid C-cell tumors (observed in rodent studies but not conclusively demonstrated in humans). Patients should be counseled to report right upper quadrant pain, which could indicate gallbladder complications. Severe dehydration from gastrointestinal symptoms may lead to acute kidney injury, so adequate hydration is important.
These medications are contraindicated during pregnancy, and women of reproductive potential should use effective contraception during treatment. Semaglutide should be discontinued at least 2 months before a planned pregnancy. Patients with severe gastroparesis should use these medications with caution, as they may worsen symptoms.
Comprehensive medical assessment is essential before initiating weight loss injection therapy, particularly for patients with known or suspected fatty liver disease. The evaluation should begin with a thorough medical history, including alcohol consumption patterns, medication review (especially hepatotoxic agents), metabolic disease history, and family history of liver disease. Physical examination should assess for signs of chronic liver disease, though these are often absent in early MASLD.
Eligibility for weight loss injections typically requires a BMI ≥30 kg/m² or ≥27 kg/m² with at least one weight-related complication (such as hypertension, dyslipidemia, type 2 diabetes, or MASLD). For women of reproductive potential, pregnancy testing and contraception planning are essential, as these medications are contraindicated during pregnancy.
Laboratory evaluation forms the foundation of pre-treatment assessment. A comprehensive metabolic panel including liver function tests (ALT, AST, alkaline phosphatase, bilirubin, albumin) establishes baseline hepatic function. Additional testing should include fasting glucose or hemoglobin A1c, lipid panel, complete blood count, and thyroid function. For patients with elevated liver enzymes, further workup may include hepatitis B and C serologies, iron studies, autoimmune markers, and ceruloplasmin to exclude alternative causes of liver disease.
Non-invasive assessment of liver fibrosis has become increasingly important in MASLD management. The FIB-4 index, calculated from age, platelet count, and transaminase levels, provides a simple screening tool for advanced fibrosis. Scores below 1.3 (or below 2.0 for patients over age 65) generally indicate low risk, while higher scores suggest increased probability of advanced fibrosis warranting further evaluation. Vibration-controlled transient elastography (FibroScan) offers direct measurement of liver stiffness as a surrogate for fibrosis when FIB-4 results are indeterminate.
Patients with evidence of advanced fibrosis or cirrhosis should undergo evaluation by a hepatologist before starting weight loss injections. This specialist assessment may include additional imaging, consideration of liver biopsy, and screening for complications such as esophageal varices. Contraindications to GLP-1 receptor agonists include personal or family history of medullary thyroid carcinoma, multiple endocrine neoplasia syndrome type 2, and severe gastroparesis. Patients with a history of pancreatitis require careful risk-benefit discussion, though this is not an absolute contraindication.
Systematic monitoring of liver health during weight loss injection therapy ensures early detection of any adverse effects while documenting therapeutic benefits. A practical approach includes regular assessment of liver enzymes and metabolic parameters during treatment.
Liver enzyme monitoring typically occurs at regular intervals, every 3-6 months during the first year of treatment, then annually if stable. Most patients experience improvement or normalization of previously elevated transaminases as weight loss progresses. Some patients may experience fluctuations in liver enzymes during weight loss. Persistent or progressive elevation of liver enzymes, particularly if accompanied by elevated bilirubin or decreased albumin, warrants prompt evaluation for alternative causes or medication-related hepatotoxicity.
Clinical assessment at each follow-up visit should include evaluation of weight loss progress, medication tolerance, and symptoms potentially related to liver disease (fatigue, right upper quadrant discomfort, jaundice). Patients should be educated about warning signs requiring immediate medical attention, including severe abdominal pain (potential pancreatitis or gallbladder disease), persistent vomiting, dark urine, or yellowing of skin or eyes. Monitoring renal function is advisable, particularly in patients experiencing significant gastrointestinal symptoms that could lead to dehydration.
For patients with established MASH or significant fibrosis at baseline, more intensive monitoring may be appropriate. Repeat non-invasive fibrosis assessment (FIB-4 or FibroScan) at 12-24 month intervals can track disease progression or improvement. Some specialists recommend repeat liver imaging to document reduction in hepatic steatosis, though this is not universally required. Patients with cirrhosis require ongoing surveillance for hepatocellular carcinoma with ultrasound (with or without alpha-fetoprotein) every six months, regardless of weight loss treatment.
Documentation of metabolic improvements—including changes in hemoglobin A1c, lipid profiles, and blood pressure—provides additional evidence of treatment benefit and may motivate continued adherence to therapy. For patients with diabetes, monitoring for retinopathy is important, as rapid improvement in glycemic control with GLP-1 receptor agonists has been associated with temporary worsening of diabetic retinopathy in some cases.
While weight loss injections offer powerful pharmacological intervention, comprehensive fatty liver management requires a multifaceted approach addressing lifestyle, nutrition, and metabolic health. These complementary strategies enhance the effectiveness of injectable medications and provide options for patients who cannot access or tolerate pharmacotherapy.
Dietary modification remains fundamental to MASLD treatment. The Mediterranean diet, characterized by high consumption of vegetables, fruits, whole grains, legumes, nuts, and olive oil with moderate fish intake, has demonstrated particular benefit for liver health. This dietary pattern reduces hepatic steatosis and improves insulin sensitivity independent of weight loss. Patients should minimize intake of added sugars, particularly fructose-containing beverages, refined carbohydrates, and saturated fats. Some evidence suggests that coffee consumption (2-3 cups daily) may offer hepatoprotective effects, though the mechanism remains unclear.
Physical activity provides benefits beyond caloric expenditure. Both aerobic exercise and resistance training reduce liver fat content, even without significant weight loss. Current recommendations suggest at least 150 minutes of moderate-intensity aerobic activity weekly, combined with resistance training twice weekly. For patients unable to achieve this target initially, any increase in physical activity offers benefit, and gradual progression should be encouraged.
Bariatric surgery is an effective option for patients with BMI ≥40 kg/m² or ≥35 kg/m² with obesity-related complications. Studies show significant improvement in MASH histology, including fibrosis regression, following bariatric procedures.
Pharmacological alternatives include resmetirom (Rezdiffra), which received FDA approval in 2024 for noncirrhotic MASH with F2-F3 fibrosis. This medication requires specialist management. Vitamin E (800 IU daily) may benefit non-diabetic patients with biopsy-proven MASH, though long-term safety concerns exist regarding potential increased risks of hemorrhagic stroke and prostate cancer. Pioglitazone improves liver histology in MASH but causes weight gain. For patients with diabetes and MASLD, SGLT2 inhibitors may offer metabolic and cardiovascular benefits while potentially improving liver health.
Management of metabolic comorbidities—including diabetes, hypertension, and dyslipidemia—is essential, as these conditions both contribute to and result from MASLD. Statins are safe in patients with fatty liver disease and should be used when indicated for cardiovascular risk reduction. Regular follow-up with primary care providers ensures comprehensive management of these interconnected conditions, optimizing both liver and overall health outcomes.
Yes, GLP-1 receptor agonists like semaglutide and tirzepatide are generally safe for patients with fatty liver disease and are not contraindicated in MASLD. Clinical evidence suggests these medications may actually improve liver health by reducing hepatic fat content and inflammation markers, though patients with decompensated cirrhosis require individualized specialist assessment.
Before starting weight loss injections, you need comprehensive laboratory evaluation including liver function tests (ALT, AST, bilirubin, albumin), metabolic panel, hemoglobin A1c, lipid panel, and non-invasive fibrosis assessment using the FIB-4 score. Patients with evidence of advanced fibrosis should undergo hepatologist evaluation before treatment initiation.
Liver enzyme monitoring typically occurs every 3-6 months during the first year of treatment, then annually if results remain stable. Most patients experience improvement in previously elevated liver enzymes as weight loss progresses, though persistent or progressive elevation warrants prompt evaluation for alternative causes.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.