LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide (Mounjaro for type 2 diabetes, Zepbound for weight management) is an FDA-approved dual GIP/GLP-1 receptor agonist that significantly suppresses appetite while promoting weight loss. While this appetite reduction facilitates caloric restriction, it creates a nutritional challenge: many patients struggle to consume adequate protein despite increased physiological needs during active weight loss. Evidence-based guidelines recommend 1.2 to 1.6 grams of protein per kilogram of ideal body weight daily—substantially higher than standard dietary recommendations—to preserve lean muscle mass, maintain metabolic rate, and optimize body composition. Understanding how to meet these protein targets while managing reduced appetite is essential for treatment success and long-term health outcomes.
Quick Answer: Patients taking tirzepatide should consume 1.2 to 1.6 grams of protein per kilogram of ideal body weight daily to preserve lean muscle mass during weight loss.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). For weight management, Zepbound is indicated for adults with a BMI ≥30 kg/m² or ≥27 kg/m² with at least one weight-related comorbidity, to be used alongside diet and physical activity. This medication works by mimicking naturally occurring incretin hormones that regulate blood sugar and appetite. The dual mechanism enhances insulin secretion when glucose levels are elevated, suppresses glucagon release in a glucose-dependent manner, and slows gastric emptying, though this effect may attenuate over time with continued therapy.
The appetite-suppressing effects of tirzepatide are substantial and clinically significant. Patients commonly report early satiety, reduced hunger between meals, and decreased food cravings. These effects result from the medication's action on appetite centers in the hypothalamus and its impact on gastric motility. Clinical trials such as SURMOUNT-1 have demonstrated average weight loss of 15-21% of body weight over 72 weeks (depending on dose), with much of this effect attributed to reduced caloric intake.
While appetite suppression facilitates weight loss, it creates a nutritional challenge. Many patients find it difficult to consume adequate calories and nutrients, particularly protein. The reduced appetite may lead to unintentional undereating, and the delayed gastric emptying can cause feelings of fullness that persist for hours after small meals. Some patients report that certain foods may feel particularly difficult to consume, though individual tolerance varies.
Understanding these appetite changes is essential for optimizing nutrition during treatment. The goal is to leverage the medication's benefits while ensuring adequate protein intake to preserve lean body mass and support metabolic health throughout the weight loss journey.
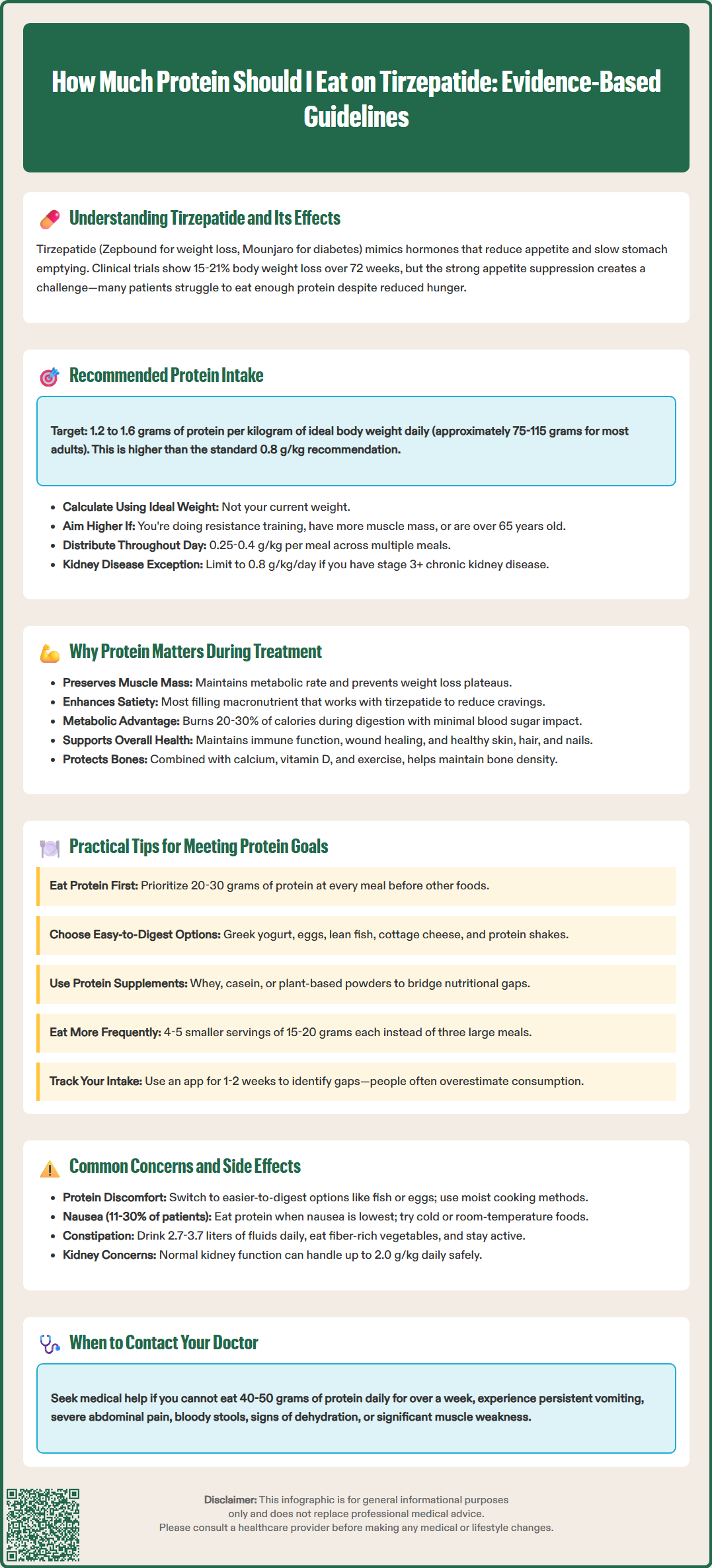
There is no official FDA-mandated protein requirement specifically for tirzepatide users, but clinical guidelines from organizations like the Obesity Medicine Association and American Association of Clinical Endocrinology recommend higher protein intake during pharmacologic weight loss compared to standard dietary recommendations. The general US dietary reference intake for protein is 0.8 grams per kilogram of body weight daily for adults, but this baseline may be insufficient during active weight loss.
For patients taking tirzepatide, evidence-based recommendations suggest 1.2 to 1.6 grams of protein per kilogram of ideal body weight daily during hypocaloric weight loss. This translates to approximately 75-115 grams daily for most adults, though needs vary significantly based on height, frame size, and activity level. Some clinicians use an alternative calculation of 0.6 to 0.8 grams per pound of ideal body weight, which yields similar targets. Ideal body weight can be calculated using standard formulas (e.g., Devine formula) or determined with healthcare provider assistance.
Patients with higher lean body mass, those engaged in resistance training, or individuals with significant weight loss goals may benefit from protein intake at the upper end of this range. Intake up to 2.0 g/kg ideal body weight may be appropriate short-term for some individuals with normal kidney function under clinical supervision. Older adults (over 65 years) should particularly prioritize adequate protein (1.2-1.5 g/kg/day) to prevent sarcopenia during weight loss.
Important considerations for calculating your protein needs:
Use ideal or adjusted body weight rather than current weight for calculations
Distribute protein across multiple meals (0.25-0.4 g/kg per meal)
Prioritize protein intake early in the day when appetite may be better
If you have chronic kidney disease (CKD stage 3 or higher), follow ADA/KDIGO guidelines of approximately 0.8 g/kg/day unless otherwise directed by your nephrologist
Work with a registered dietitian for personalized recommendations
These targets aim to preserve lean muscle mass, support metabolic rate, and optimize body composition changes during weight loss. Individual needs should be determined with healthcare provider guidance based on your specific medical conditions and treatment goals.
Adequate protein intake during tirzepatide treatment serves multiple critical physiological functions that directly impact treatment success and long-term health outcomes. Understanding these mechanisms helps patients prioritize protein despite reduced appetite.
Preservation of lean body mass is the primary concern during rapid weight loss. Without adequate protein, the body catabolizes muscle tissue alongside fat stores. Research on hypocaloric diets consistently shows that higher protein intake (1.2-1.6 g/kg) preserves significantly more lean mass compared to standard protein intake. Since muscle tissue is metabolically active, preserving it helps maintain resting metabolic rate and prevents the metabolic adaptation that can impede continued weight loss or contribute to weight regain.
Satiety and appetite regulation represent another key benefit. Protein is the most satiating macronutrient, triggering release of satiety hormones including peptide YY and cholecystokinin. While tirzepatide already suppresses appetite, adequate protein helps patients feel satisfied with smaller portions and may reduce cravings for less nutritious foods. This synergistic effect can improve dietary adherence.
Metabolic and glycemic benefits are particularly relevant for patients with type 2 diabetes. Protein has minimal direct impact on blood glucose compared to carbohydrates, potentially leading to lower postprandial glucose excursions. Protein also has a higher thermic effect of food (20-30% of calories consumed) compared to carbohydrates (5-10%) or fats (0-3%), meaning the body expends more energy digesting and metabolizing protein.
Additional benefits include supporting immune function, wound healing, hormone production, and maintenance of skin, hair, and nail health—all of which can be compromised during rapid weight loss. Adequate protein, along with sufficient calcium, vitamin D, and resistance exercise, also supports bone health, which is particularly important as weight loss can affect bone mineral density.
Meeting protein targets while experiencing significant appetite suppression requires strategic planning and practical approaches. The following evidence-based strategies can help patients optimize protein intake despite reduced hunger.
Prioritize protein at every meal. Make protein the first food you consume when appetite is present. Front-loading meals with protein ensures you meet minimum requirements even if you cannot finish the entire meal. Aim for 0.25-0.4 grams of protein per kilogram of body weight per meal (higher for older adults), typically 20-30 grams for most adults.
Choose protein-dense, easily digestible options:
Greek yogurt (15-20g per cup) or skyr
Eggs (6-7g per large egg)
Lean poultry, fish, or seafood
Cottage cheese (14g per half cup)
Protein shakes or smoothies when solid food feels difficult
Lean ground turkey or chicken
Tofu or tempeh for plant-based options
Utilize protein supplements strategically. When solid food intake is limited, high-quality protein powders (whey, casein, or plant-based blends) can help bridge nutritional gaps. Mix with unsweetened almond milk or water for a lighter option that may be better tolerated. Protein shakes can provide 20-30 grams of protein in a more easily consumed form, particularly useful between meals or when nausea is present.
Time your protein intake appropriately. Many patients report better appetite earlier in the day. Consider a protein-rich breakfast and lunch, with lighter options in the evening. Avoid drinking large amounts of liquid before meals, as this can worsen early satiety.
Prepare smaller, more frequent protein servings. Rather than three large meals, consider 4-5 smaller eating occasions with 15-20 grams of protein each. This approach may feel more manageable with reduced gastric capacity.
Track your intake initially. Use a food tracking app for 1-2 weeks to assess actual protein consumption. Many patients overestimate their intake when appetite is suppressed. Objective tracking helps identify gaps and adjust strategies accordingly.
If you take insulin or sulfonylureas: Discuss with your healthcare provider about potential dose adjustments, as reduced food intake may increase hypoglycemia risk.
Patients taking tirzepatide frequently encounter specific challenges related to protein intake and digestion. Understanding these concerns and appropriate management strategies is essential for treatment success.
Difficulty tolerating dense proteins is a commonly reported challenge. Some patients find that red meat, chicken breast, and other dense protein sources may feel particularly heavy or cause discomfort due to delayed gastric emptying. Management strategies include choosing more easily digestible proteins (fish, eggs, Greek yogurt), cutting meat into very small pieces, cooking proteins with moisture (braising, slow-cooking), and avoiding dry or tough preparations. If solid proteins remain difficult, liquid protein sources (shakes, bone broth with added protein powder) can serve as temporary alternatives.
Nausea affecting protein intake occurs in approximately 11-30% of patients (per FDA labeling), particularly during dose escalation. Nausea may worsen with protein-rich foods. To manage this, consume protein during times of day when nausea is minimal, choose cold or room-temperature proteins which may be better tolerated, incorporate ginger or peppermint tea, and consider anti-nausea medications if symptoms are severe. Notify your healthcare provider if nausea prevents adequate nutrition for more than a few days.
Constipation with high-protein intake can occur, especially when protein displaces fiber-rich foods and fluid intake decreases. Ensure adequate hydration (approximately 3.7 liters daily for men and 2.7 liters daily for women from all sources, including food), include fiber-rich vegetables alongside protein sources, consider a fiber supplement if needed, and maintain physical activity to support bowel motility.
Concerns about kidney function occasionally arise with higher protein intake. For patients with normal kidney function, protein intake up to 2.0 g/kg body weight is generally considered safe for short-term use with appropriate monitoring. However, patients with chronic kidney disease (particularly stage 3 or higher or those with albuminuria) should follow ADA/KDIGO guidelines of approximately 0.8 g/kg/day unless otherwise directed by their nephrologist. Patients with diabetes should have kidney function assessed before significantly increasing protein intake.
When to seek medical advice:
Inability to consume more than 40-50 grams of protein daily for more than one week
Persistent nausea or vomiting lasting more than 24 hours
Signs of dehydration (dark urine, dizziness, extreme thirst)
Severe or constant abdominal pain
Black or bloody stools
Persistent constipation not responding to over-the-counter measures after 3 days
Signs of muscle loss (significant weakness, difficulty with usual activities)
Your healthcare provider may recommend working with a registered dietitian specializing in obesity medicine to develop an individualized nutrition plan that optimizes protein intake while managing medication side effects.
Multiply your ideal body weight in kilograms by 1.2 to 1.6 grams, or use 0.6 to 0.8 grams per pound of ideal body weight. For most adults, this translates to approximately 75-115 grams of protein daily, though individual needs vary based on height, activity level, and medical conditions.
Yes, high-quality protein shakes are an effective strategy when solid food intake is limited due to appetite suppression. They can provide 20-30 grams of protein in an easily consumed form and are particularly useful between meals or when nausea is present.
For patients with normal kidney function, protein intake of 1.2-1.6 g/kg ideal body weight is generally safe and beneficial. However, patients with chronic kidney disease stage 3 or higher should follow ADA/KDIGO guidelines of approximately 0.8 g/kg/day and have kidney function assessed before significantly increasing protein intake.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.