LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does tirzepatide make you hungry? This is a common question among patients prescribed this medication for type 2 diabetes or weight management. Tirzepatide (Mounjaro, Zepbound) is a dual GIP and GLP-1 receptor agonist designed to reduce appetite and promote satiety, not increase hunger. While most patients experience appetite suppression, some report unexpected hunger during treatment. Understanding why this occurs and how to manage it is essential for treatment success. This article explores tirzepatide's effects on appetite, reasons for paradoxical hunger responses, and evidence-based strategies to optimize your therapy.
Quick Answer: Tirzepatide is designed to reduce appetite and promote satiety, not increase hunger, through its dual GIP and GLP-1 receptor agonist mechanism.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). It's prescribed as an adjunct to diet and physical activity for adults with type 2 diabetes or for weight management in adults with a BMI ≥30 kg/m², or ≥27 kg/m² with at least one weight-related comorbidity. The medication works primarily by mimicking naturally occurring incretin hormones that regulate blood glucose and appetite. Under normal circumstances, tirzepatide is designed to reduce appetite and promote satiety, not increase hunger.
The mechanism involves several pathways in appetite regulation. GLP-1 receptor activation in the hypothalamus and brainstem reduces hunger signals and slows gastric emptying, leading to prolonged feelings of fullness after meals. The GIP component enhances insulin secretion and may contribute to glucose metabolism, though its specific role in appetite regulation is still being fully characterized. Together, these actions typically result in decreased caloric intake and gradual weight loss, which are well-documented effects in clinical trials such as SURMOUNT-1 and SURPASS studies.
Many patients experience appetite suppression during tirzepatide therapy, particularly during the initial weeks of treatment and following dose escalations. Common gastrointestinal side effects include nausea and decreased appetite. The medication's half-life of approximately five days allows for once-weekly subcutaneous administration, though individual responses may vary throughout the dosing interval.
It is important to understand that tirzepatide's primary pharmacological action is appetite reduction rather than stimulation. When patients report increased hunger while taking this medication, it typically represents an atypical response that warrants clinical evaluation rather than an expected drug effect.
While increased hunger is not a recognized adverse effect of tirzepatide, some patients do report experiencing unexpected appetite increases during treatment. Several factors may explain this paradoxical response, though there is no official established link between tirzepatide and increased hunger in the prescribing information.
Dosing and individual response variability may contribute to hunger experiences. Patients who are early in their titration schedule (starting at 2.5 mg weekly) may not yet experience full appetite suppression. Additionally, some individuals may notice variations in appetite throughout the weekly dosing interval, though this is based on anecdotal reports rather than established clinical evidence.
Metabolic adaptation and caloric restriction can trigger compensatory hunger signals. As patients lose weight on tirzepatide, the body may activate counter-regulatory mechanisms to defend against further weight loss. Hormones such as ghrelin (the "hunger hormone") may increase, while leptin levels decline with fat mass reduction. This physiological response represents the body's attempt to restore energy balance rather than a direct drug effect.
Psychological factors and eating patterns also play significant roles. Some patients may misinterpret other sensations (such as nausea, anxiety, or habitual eating cues) as hunger. Others may experience changes in appetite patterns due to improved glycemic control—when blood glucose stabilizes, the frequency of hypoglycemic episodes (which typically cause intense hunger) may decrease, potentially normalizing overall appetite patterns.
Medication interactions or underlying conditions should be considered. Certain medications (such as corticosteroids, antipsychotics, or antihistamines) can increase appetite independently. Thyroid disorders, psychiatric conditions, or inadequately controlled diabetes may also manifest as increased hunger despite tirzepatide therapy.
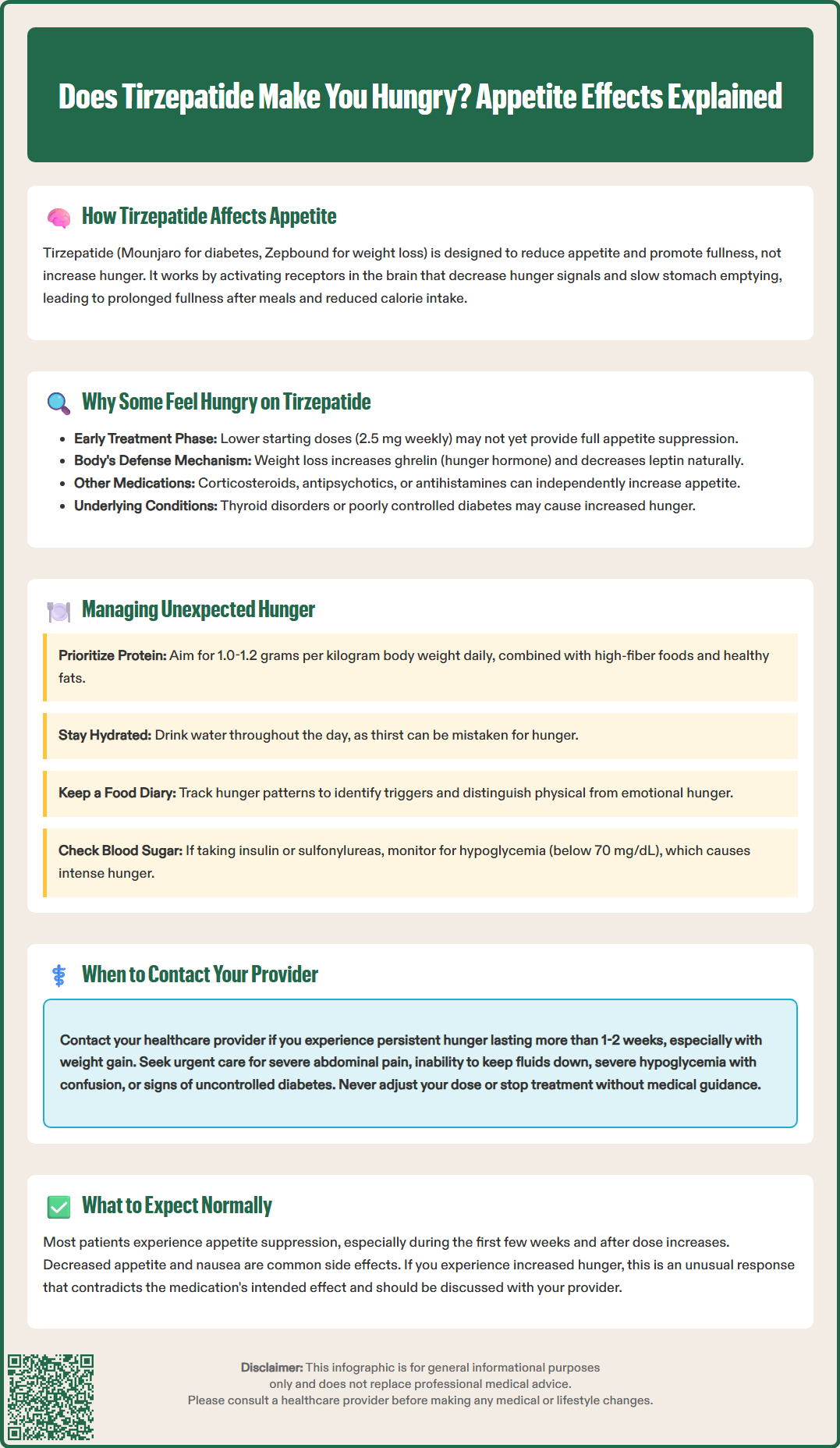
If you experience unexpected hunger while taking tirzepatide, several evidence-based strategies can help manage appetite while maintaining treatment efficacy. These approaches should be implemented in consultation with your healthcare provider to ensure they align with your overall treatment plan.
Optimize meal composition and timing by focusing on nutrient-dense, high-satiety foods. Prioritize adequate protein intake (generally 1.0-1.2 grams per kilogram of body weight daily for most adults) at each meal, as protein provides superior satiety compared to carbohydrates or fats. Note that protein needs should be individualized, and those with kidney disease should follow their provider's guidance. Include high-fiber foods such as vegetables, legumes, and whole grains, which slow gastric emptying and promote fullness. Healthy fats from sources like avocados, nuts, and olive oil can also enhance satiety. Consider eating smaller, more frequent meals rather than three large meals if this pattern better controls hunger.
Maintain adequate hydration, as thirst is sometimes misinterpreted as hunger. Individual fluid needs vary based on activity level, climate, and overall health. Drinking water before meals may also promote earlier satiety.
Review your medication timing and dosing schedule with your healthcare provider. Tirzepatide should be administered once weekly, and if changing the day of administration, ensure at least 3 days between doses during the transition. Your provider may evaluate whether dose adjustment according to the FDA-approved titration schedule is appropriate based on your response and tolerance.
Monitor for hypoglycemia, particularly if you take tirzepatide alongside insulin or sulfonylureas. Low blood glucose (below 70 mg/dL) can trigger intense hunger and should be addressed through medication adjustment rather than increased food intake alone. If hypoglycemia occurs, treat with 15 grams of fast-acting carbohydrate and recheck glucose after 15 minutes.
Address behavioral and environmental factors by keeping a food and hunger diary to identify triggers. Distinguish between physical hunger and emotional or habitual eating. Stress management techniques, adequate sleep (7–9 hours nightly), and regular physical activity all support healthy appetite regulation independent of medication effects.
While mild appetite fluctuations during tirzepatide therapy may not require immediate intervention, certain situations warrant prompt communication with your healthcare provider to ensure treatment safety and efficacy.
Contact your provider if you experience persistent or severe hunger that interferes with your ability to maintain appropriate caloric intake or achieve treatment goals. Unexplained increased appetite lasting more than one to two weeks, especially if accompanied by weight gain, may indicate inadequate dosing, medication tolerance, or an underlying medical condition requiring evaluation. Your provider can assess whether dose adjustment, additional investigations, or alternative treatment strategies are needed.
Seek urgent medical attention for:
Severe, persistent abdominal pain (with or without vomiting), which could indicate pancreatitis
Right upper quadrant pain, jaundice, or fever, which may suggest gallbladder disease
Inability to keep fluids down or signs of dehydration
Severe hypoglycemia (blood glucose <54 mg/dL) with confusion, loss of consciousness, or inability to self-treat
Symptoms like excessive thirst, frequent urination, unexplained weight loss despite increased appetite, or persistent fatigue, which may indicate inadequate diabetes control
Report any signs of hypoglycemia (blood glucose <70 mg/dL), particularly if you take insulin or sulfonylureas with tirzepatide. Symptoms include shakiness, sweating, confusion, rapid heartbeat, or intense hunger. Recurrent hypoglycemia requires medication adjustment to prevent serious complications.
Discuss appetite changes before making treatment modifications. Never adjust your tirzepatide dose or discontinue therapy without medical guidance, as abrupt changes may affect glycemic control and weight management outcomes. Remember that tirzepatide carries a boxed warning and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Report any neck mass, hoarseness, or difficulty swallowing promptly.
Your healthcare team can perform appropriate investigations, including hemoglobin A1c testing, thyroid function studies, or medication reviews, to identify and address the underlying cause of unexpected appetite changes while optimizing your tirzepatide therapy for maximum benefit and safety.
No, increased hunger is not a recognized side effect of tirzepatide. The medication is designed to reduce appetite through GIP and GLP-1 receptor activation, and most patients experience appetite suppression rather than increased hunger.
Unexpected hunger may occur due to early titration phases with lower doses, metabolic adaptation as the body responds to weight loss, psychological factors, medication interactions, or underlying conditions. This represents an atypical response rather than the medication's intended effect.
Contact your healthcare provider if you experience persistent hunger lasting more than one to two weeks, unexplained weight gain, signs of hypoglycemia, severe abdominal pain, or symptoms suggesting inadequate diabetes control. Never adjust your dose without medical guidance.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.