LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Experiencing weight gain while taking tirzepatide can be frustrating and confusing, especially when this medication is specifically prescribed for weight management. Tirzepatide (Zepbound, Mounjaro) is a dual GIP/GLP-1 receptor agonist that typically promotes significant weight loss by reducing appetite and slowing gastric emptying. However, several factors—including medication interactions, metabolic adaptation, lifestyle variables, and underlying medical conditions—can interfere with expected results or cause paradoxical weight gain. Understanding why this occurs is essential for optimizing your treatment and achieving your health goals. This article explores the common reasons for weight gain on tirzepatide and when to seek medical guidance.
Quick Answer: Weight gain on tirzepatide can occur due to fluid retention, metabolic adaptation, inadequate dosing, medication interactions, lifestyle factors, or underlying medical conditions that counteract the medication's appetite-suppressing effects.
The medication acts on receptors in the brain's appetite centers, particularly the hypothalamus, to reduce hunger and increase feelings of fullness after eating. By activating GLP-1 receptors, tirzepatide slows gastric emptying, meaning food stays in your stomach longer, which contributes to prolonged satiety. This gastric emptying effect is most pronounced after the first dose and typically decreases with continued dosing. The GIP component enhances insulin secretion when blood glucose is elevated and may also influence fat metabolism, though its exact contribution to weight loss in humans is still being studied.
Clinical trials have demonstrated substantial weight loss with tirzepatide. In the SURMOUNT-1 trial, participants without diabetes lost an average of 15-22% of their body weight over 72 weeks, depending on the dose (5-15mg). Weight loss tends to be lower in people with type 2 diabetes. Individual responses vary considerably. The medication requires weekly subcutaneous injection and gradual dose escalation to minimize gastrointestinal side effects. Understanding this mechanism is important because it clarifies that tirzepatide facilitates weight loss primarily by reducing appetite and food intake rather than directly burning fat or significantly increasing metabolism. When weight gain occurs despite treatment, it suggests that factors may be interfering with these intended effects or that other physiological processes are at play.
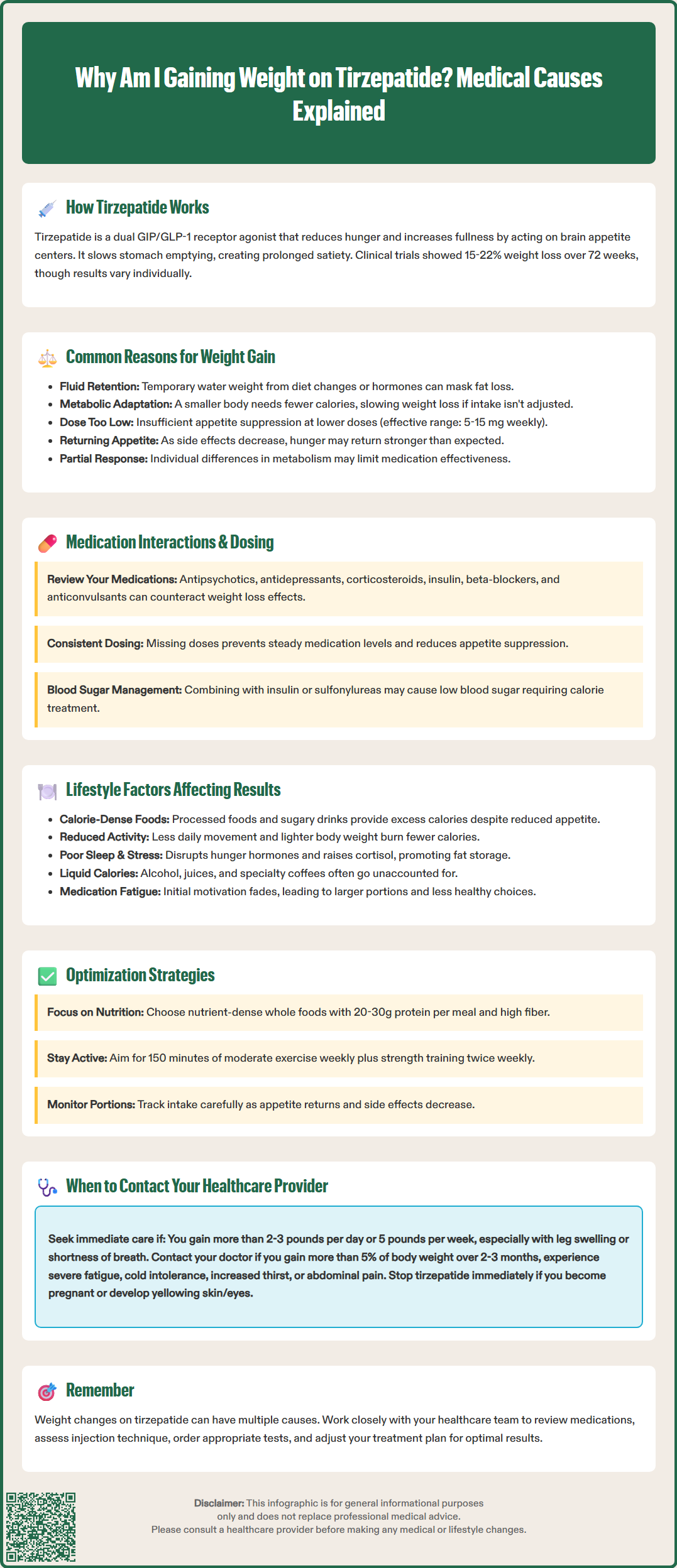
Weight gain while taking tirzepatide is possible but not typical, and can occur for several physiological and medication-related reasons. One potential explanation is fluid fluctuations, which may manifest as temporary water weight gain. While tirzepatide itself is not specifically associated with edema in FDA labeling, changes in diet, sodium intake, or concurrent medications might cause fluid shifts that can mask fat loss on the scale, even when body composition is improving. Other common causes of transient weight fluctuations include menstrual cycle changes, constipation, and glycogen repletion (which binds water).
Metabolic adaptation represents another consideration. As you lose weight, your body's basal metabolic rate naturally decreases because a smaller body requires fewer calories to maintain basic functions. This adaptive thermogenesis can slow weight loss over time and, if caloric intake isn't adjusted accordingly, may contribute to weight stabilization or modest regain. Some patients may interpret this plateau as treatment failure when it actually reflects normal physiological adaptation.
Inadequate dosing can also limit tirzepatide's effectiveness. The medication requires gradual titration from 2.5 mg weekly up to maintenance doses of 5-15 mg weekly. Patients who remain on lower doses may not experience the full appetite-suppressing effects needed for continued weight loss. Additionally, some individuals may be partial responders to GLP-1-based therapies due to various factors that aren't fully understood, including differences in individual metabolism and hormone signaling.
Finally, gastrointestinal side effects that improve over time may paradoxically lead to weight gain. Early in treatment, nausea and reduced appetite often cause rapid weight loss. As tolerance develops and these symptoms resolve, some patients find their appetite returns more robustly than expected, potentially leading to increased food intake if not monitored carefully. This rebound effect requires conscious attention to portion sizes and food choices.
Several medication-related factors can interfere with tirzepatide's weight loss effects or contribute to weight gain. Concomitant medications known to promote weight gain may counteract tirzepatide's benefits. These include certain antipsychotics (olanzapine, quetiapine, risperidone), mood stabilizers (lithium, valproate), some antidepressants (mirtazapine, paroxetine, amitriptyline), corticosteroids (prednisone), certain diabetes medications (insulin, sulfonylureas, thiazolidinediones), some beta-blockers (propranolol, metoprolol), and anticonvulsants (gabapentin, pregabalin). If you started or increased doses of these medications while on tirzepatide, they may be contributing to weight gain.
Tirzepatide can affect the absorption of oral medications due to delayed gastric emptying. While this doesn't directly cause weight gain, it may alter the effectiveness of other treatments. For oral contraceptives, the FDA label recommends using a non-oral or backup method for 4 weeks after initiating tirzepatide and after each dose increase. For medications with narrow therapeutic windows, discuss timing of administration with your healthcare provider. Insulin and sulfonylurea interactions deserve special mention: these medications can cause hypoglycemia when combined with tirzepatide, and treating low blood sugar with carbohydrates adds calories that may offset weight loss efforts.
Dosing inconsistencies can significantly impact results. Missing doses or irregular administration patterns may prevent steady therapeutic levels, reducing appetite suppression. Conversely, some patients may not tolerate dose escalation due to side effects and remain on subtherapeutic doses. The FDA-approved dosing schedule involves gradual increases every four weeks, but individual tolerance varies. Some patients require slower titration or may not reach the higher maintenance doses (10-15 mg) where weight loss effects are most pronounced. For proper injection technique, always follow the Instructions for Use provided with your medication to ensure optimal delivery.
While tirzepatide reduces appetite, weight loss ultimately depends on maintaining a caloric deficit, and several lifestyle factors can undermine this balance. Dietary composition and quality matter significantly. Some patients compensate for reduced meal frequency by consuming calorie-dense foods—such as processed snacks, sugary beverages, or high-fat items—during smaller eating windows. Even with reduced appetite, consuming foods high in refined carbohydrates and unhealthy fats can provide excess calories. The American Diabetes Association recommends focusing on nutrient-dense whole foods, lean proteins, vegetables, and whole grains to maximize satiety. Prioritizing adequate protein (20-30g per meal) and fiber can help maintain fullness between meals.
Physical activity levels play a crucial role in weight management. Reduced appetite may lead to decreased energy levels, causing some patients to become more sedentary. This reduction in non-exercise activity thermogenesis (NEAT)—the calories burned through daily movement—can significantly impact total energy expenditure. The US Physical Activity Guidelines recommend at least 150 minutes of moderate-intensity activity weekly plus muscle-strengthening activities twice weekly. Additionally, weight loss itself reduces the energy cost of physical activity, as moving a lighter body requires fewer calories. Without intentional exercise or movement, this creates a scenario where caloric expenditure decreases while intake may not decline proportionally.
Sleep quality and stress management represent often-overlooked factors. Poor sleep disrupts hormones that regulate hunger (ghrelin and leptin), potentially overriding tirzepatide's appetite-suppressing effects. Chronic stress elevates cortisol, which promotes fat storage, particularly visceral adiposity, and can trigger emotional eating behaviors. Some patients may also experience medication fatigue—a psychological phenomenon where the initial motivation and dietary vigilance wane over time, leading to gradual increases in portion sizes and less healthy food choices.
Finally, alcohol consumption can contribute to weight gain. Alcoholic beverages provide empty calories (7 calories per gram of alcohol) and may increase appetite while lowering inhibitions around food choices. Some patients who successfully reduce food intake may not account for liquid calories from alcohol, juices, or specialty coffee drinks, which can substantially impact overall caloric balance.
Certain patterns of weight gain while taking tirzepatide warrant prompt medical evaluation. Contact your healthcare provider if you experience rapid weight gain—defined as more than 2-3 pounds in a day or 5 pounds in a week—particularly if accompanied by swelling in your legs, ankles, or abdomen, shortness of breath, or difficulty breathing when lying flat. These symptoms may indicate fluid retention from heart failure or other serious conditions requiring immediate assessment.
You should also seek medical advice if you experience persistent weight gain despite adherence to your prescribed regimen and lifestyle modifications. Gaining more than 5% of your body weight over 2-3 months while consistently taking tirzepatide and following dietary recommendations suggests the need for medication reassessment. Your provider may need to evaluate for underlying conditions such as hypothyroidism, Cushing's syndrome, polycystic ovary syndrome, or other hormonal imbalances that can cause weight gain independent of tirzepatide therapy.
New or worsening symptoms accompanying weight changes require evaluation. These include severe fatigue, cold intolerance, constipation, depression, or changes in menstrual patterns, which may indicate thyroid dysfunction. Additionally, increased thirst, frequent urination, or unexplained hunger despite taking tirzepatide could suggest inadequate diabetes control or other metabolic issues. Abdominal pain, persistent nausea, or vomiting may indicate pancreatitis—a rare but serious adverse effect requiring immediate medical attention. Upper right abdominal pain, fever, or yellowing of the skin/eyes could indicate gallbladder disease, which occurs more frequently with weight loss medications. Severe gastrointestinal symptoms with signs of dehydration (markedly decreased urination, dizziness) require urgent evaluation due to risk of acute kidney injury.
Importantly, tirzepatide carries a boxed warning for risk of thyroid C-cell tumors and is contraindicated in people with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2. If you become pregnant while taking tirzepatide, contact your provider immediately as the medication should be discontinued.
Finally, discuss weight concerns with your provider if you're considering medication adjustments or additions. Your healthcare team can review your complete medication list for potential interactions, assess whether dose escalation is appropriate, evaluate your injection technique, and determine if additional investigations such as thyroid function tests or metabolic panels are warranted. They may also refer you to a registered dietitian or endocrinologist for specialized management. Remember that weight management is complex and multifactorial—open communication with your healthcare team is essential for optimizing your treatment outcomes and addressing any underlying issues that may be affecting your response to tirzepatide.
Tirzepatide's effectiveness may appear to diminish due to metabolic adaptation, where your body requires fewer calories as you lose weight, or due to tolerance development where gastrointestinal side effects resolve and appetite returns. Dose optimization and lifestyle adjustments can help maintain weight loss momentum.
Medications that commonly promote weight gain include certain antipsychotics, antidepressants (particularly mirtazapine and paroxetine), corticosteroids, insulin, sulfonylureas, some beta-blockers, and anticonvulsants like gabapentin. These may counteract tirzepatide's weight loss effects when taken concurrently.
Contact your healthcare provider immediately for rapid weight gain (more than 2-3 pounds daily or 5 pounds weekly), especially with swelling, breathing difficulty, or chest discomfort. Also seek evaluation for persistent weight gain exceeding 5% of body weight over 2-3 months despite medication adherence and lifestyle modifications.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.