LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

GLP-1 medications like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound) deliver remarkable weight loss but create a critical nutritional challenge: maintaining adequate protein intake. Understanding how much protein to eat on GLP-1 therapy is essential for preserving lean muscle mass during rapid weight loss. While these medications suppress appetite effectively, they can inadvertently lead to insufficient protein consumption, increasing the risk of muscle loss alongside fat reduction. This comprehensive guide provides evidence-based protein recommendations, practical strategies, and expert insights to help patients and healthcare providers optimize nutrition during GLP-1 treatment.
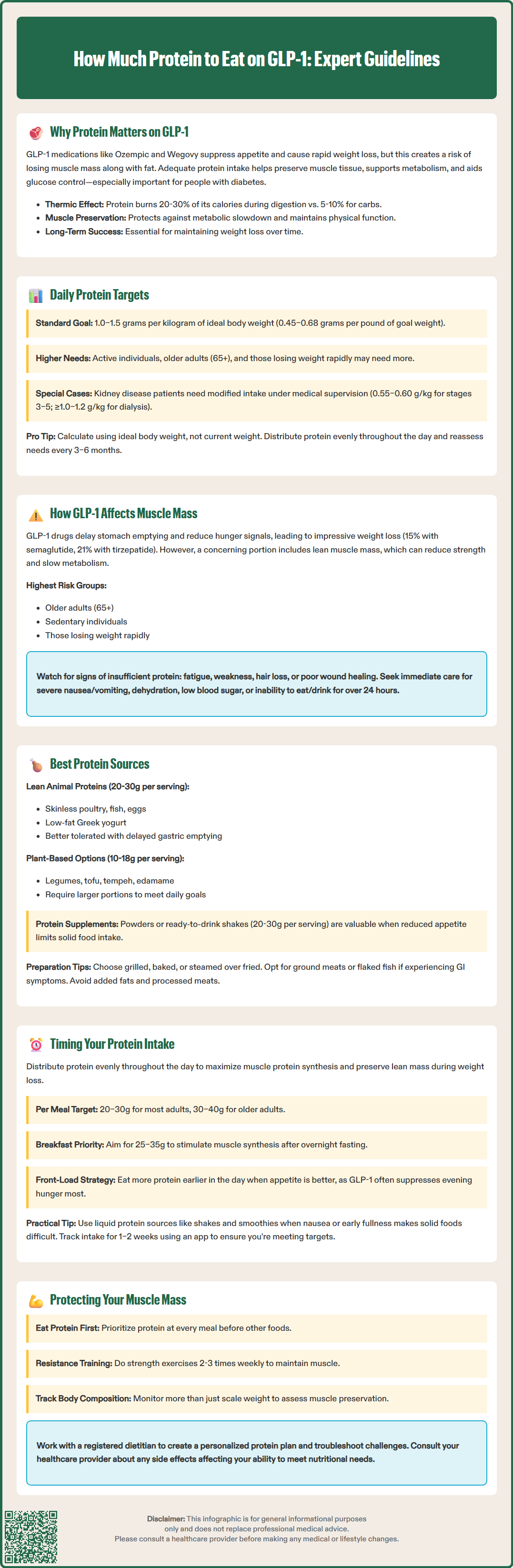
Quick Answer: Patients taking GLP-1 medications should aim for 1.0–1.5 grams of protein per kilogram of ideal body weight daily (approximately 0.45–0.68 grams per pound) to preserve lean muscle mass during weight loss.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
GLP-1 receptor agonists—including semaglutide (Ozempic, Wegovy) and liraglutide (Victoza, Saxenda)—along with tirzepatide (Mounjaro, Zepbound), a dual GIP/GLP-1 receptor agonist, have transformed the management of type 2 diabetes and obesity. These medications work by mimicking incretin hormones, which enhance insulin secretion, suppress glucagon release, and significantly reduce appetite through delayed gastric emptying and central nervous system effects. While this appetite suppression facilitates substantial weight loss, it also creates a clinical challenge: ensuring adequate protein intake to preserve lean body mass.
Protein becomes critically important during GLP-1 therapy because rapid weight loss—particularly when exceeding 1–2 pounds per week—increases the risk of losing muscle mass alongside fat tissue. Clinical studies suggest that a significant proportion of weight lost during caloric restriction can come from lean tissue. This loss of muscle mass can reduce metabolic rate, impair physical function, and compromise long-term weight maintenance. For patients with diabetes, preserving muscle is especially important because skeletal muscle plays a key role in glucose disposal and insulin sensitivity.
The standard dietary reference intake for protein in adults is 0.8 grams per kilogram of body weight per day, but this baseline recommendation may be insufficient for individuals undergoing significant weight loss on GLP-1 medications. Expert consensus suggests that patients taking GLP-1 receptor agonists or dual GIP/GLP-1 receptor agonists may benefit from 1.0–1.5 grams of protein per kilogram of ideal or adjusted body weight daily to support lean muscle mass preservation.
For practical application, this translates to approximately 0.45–0.68 grams per pound of goal body weight. For example, a patient with a goal weight of 180 pounds should aim for roughly 80–120 grams of protein daily. Some obesity medicine specialists suggest higher intakes for specific populations, particularly patients who are physically active, older adults at higher risk for sarcopenia, or those losing weight rapidly. The American Diabetes Association emphasizes individualized nutrition therapy rather than fixed protein targets, and protein goals should be adjusted based on kidney function, activity level, and rate of weight loss.
Patients with chronic kidney disease require special consideration. For CKD stages 3–5 (non-dialysis), the Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines typically recommend 0.55–0.60 g/kg/day (0.6–0.8 g/kg in diabetes). Patients on dialysis generally require higher protein intake (≥1.0–1.2 g/kg). All patients with CKD should work with a registered dietitian and nephrologist to determine appropriate protein levels.
Key considerations for protein targets:
Use ideal body weight (IBW) or adjusted body weight for calculations, not current weight in patients with obesity
Distribute protein across meals rather than concentrating in one sitting
Monitor for signs of inadequate intake: fatigue, weakness, hair loss, or poor wound healing
Reassess needs every 3–6 months as weight changes
Consult with a registered dietitian for personalized recommendations
GLP-1 receptor agonists and dual GIP/GLP-1 receptor agonists exert their appetite-suppressing effects through multiple mechanisms. These medications delay gastric emptying (though this effect may diminish somewhat with chronic use), which prolongs the sensation of fullness after meals. They also act on receptors in the hypothalamus and brainstem, reducing hunger signals and food-seeking behavior. Additionally, these medications may alter food preferences, with many patients reporting reduced cravings for high-fat and high-sugar foods. While these effects are therapeutically beneficial for weight loss, they can inadvertently lead to inadequate overall caloric and protein intake.
Clinical trials have documented substantial weight loss with these medications—typically 15% of body weight with semaglutide 2.4 mg (STEP 1 trial) and approximately 21% with tirzepatide 15 mg (SURMOUNT-1 trial) at 72 weeks. Body composition analyses from clinical studies indicate that a portion of weight lost may be lean mass rather than fat mass. This is concerning because loss of skeletal muscle can lead to decreased strength, reduced functional capacity, and a lower resting metabolic rate, potentially making weight regain more likely after medication discontinuation.
The risk of muscle loss is particularly pronounced in certain populations: older adults (age 65+) who already face age-related sarcopenia, sedentary individuals without resistance training stimulus for muscle preservation, and patients losing weight very rapidly. Early satiety and food aversions—common side effects of these medications—can make it challenging to consume adequate protein-rich foods, especially in the first weeks after dose escalation.
Strategies to mitigate muscle loss include:
Prioritizing protein at each meal before other macronutrients
Incorporating resistance training at least 2–3 times weekly
Monitoring body composition, not just scale weight
Working with your healthcare provider if side effects prevent adequate nutrition—never adjust medication doses on your own
Contact your healthcare provider immediately if you experience:
Severe or persistent nausea, vomiting, or abdominal pain
Signs of dehydration (extreme thirst, dizziness, dark urine)
Low blood sugar symptoms (if taking insulin or sulfonylureas)
Inability to eat or drink for more than 24 hours
Selecting appropriate protein sources is essential for patients on GLP-1 therapy, particularly given the reduced appetite and early satiety these medications produce. The goal is to maximize protein density—grams of protein per volume of food—while choosing options that are well-tolerated and nutrient-dense.
High-quality animal proteins provide complete amino acid profiles and are efficiently absorbed. Lean options are generally better tolerated when gastric emptying is delayed:
Poultry: Skinless chicken or turkey breast (26–30g protein per 3.5 oz serving)
Fish and seafood: Salmon, cod, shrimp, tuna (20–25g per 3.5 oz)
Eggs: Whole eggs or egg whites (6g per large egg, 3.6g per white)
Low-fat dairy: Greek yogurt (15–20g per 6 oz), cottage cheese (14g per ½ cup), skim milk (8g per cup)
Lean beef or pork: Sirloin, tenderloin, or pork loin (22–26g per 3.5 oz)
Plant-based proteins are valuable for patients who prefer vegetarian options or want to diversify protein sources, though they may require larger portions to meet protein goals:
Legumes: Lentils, chickpeas, black beans (15–18g per cooked cup)
Soy products: Tofu (10g per ½ cup), tempeh (15g per ½ cup), edamame (17g per cup)
Nuts and seeds: Almonds, peanut butter, chia seeds (6–8g per ¼ cup, though calorie-dense)
Whole grains: Quinoa (8g per cooked cup), though primarily a carbohydrate source
Protein supplements can be particularly useful when solid food intake is limited:
Whey or plant-based protein powders (20–30g per scoop)
Ready-to-drink protein shakes
Protein-fortified foods like high-protein yogurt or milk
Patients should be counseled to choose lean preparations—grilled, baked, or steamed rather than fried—and to be mindful of added fats that can exacerbate nausea or early satiety. Be cautious with processed meats, which can be high in sodium. Those with lactose intolerance should select lactose-free dairy options or plant alternatives. Texture matters: some patients find ground meats or flaked fish easier to tolerate than dense cuts of meat when experiencing medication-related gastrointestinal effects.
The distribution of protein intake across the day is as important as total daily amount for optimizing muscle protein synthesis and preservation during GLP-1 therapy. Research on protein metabolism suggests that consuming protein in evenly distributed doses throughout the day is more effective for maintaining lean mass than concentrating intake in one or two large meals.
Evidence suggests that approximately 20–30 grams of high-quality protein per meal is needed to effectively stimulate muscle protein synthesis in most adults. Older adults may require slightly more—closer to 30–40 grams per meal—due to "anabolic resistance," a reduced sensitivity to the muscle-building effects of protein. Consuming protein beyond these amounts at a single meal does not proportionally increase muscle synthesis; instead, the excess is typically used for energy or converted to other compounds.
Practical timing strategies for GLP-1 patients:
Breakfast: Aim for 25–35g protein to break the overnight fast and stimulate morning muscle synthesis. Examples include Greek yogurt with nuts, a protein smoothie, or eggs with turkey sausage.
Lunch and dinner: Target 25–35g protein at each meal, prioritizing protein-rich foods first when appetite is limited.
Snacks: Include 10–15g protein in one or two snacks if total daily goals aren't met through meals alone. Options include string cheese, protein bars, or a small protein shake.
Post-exercise: Consuming 20–30g protein within a few hours after resistance training may enhance muscle recovery and adaptation.
Special considerations for GLP-1 patients:
Many patients report that appetite is lowest in the evening, particularly if they take their medication in the morning or early afternoon. In such cases, front-loading protein intake earlier in the day—when appetite may be relatively better—can help achieve daily targets. Some patients find that liquid protein sources (shakes, smoothies) are better tolerated than solid foods when nausea or early satiety is prominent.
Healthcare providers should encourage patients to track protein intake for at least 1–2 weeks using a food diary or mobile app to ensure they're meeting targets. Regular follow-up with a registered dietitian experienced in obesity medicine can provide personalized guidance and troubleshooting for patients struggling to maintain adequate protein intake while on GLP-1 therapy.
Most patients on GLP-1 medications should aim for 1.0–1.5 grams of protein per kilogram of ideal body weight daily, which translates to approximately 0.45–0.68 grams per pound of goal weight. For example, someone with a goal weight of 180 pounds should target 80–120 grams of protein daily.
GLP-1 medications significantly suppress appetite, which can lead to inadequate protein consumption during rapid weight loss. Without sufficient protein, patients risk losing substantial muscle mass alongside fat tissue, which can reduce metabolic rate, impair physical function, and compromise long-term weight maintenance.
When nausea or early satiety occurs, protein-dense options that are easier to tolerate include Greek yogurt, protein shakes or smoothies, eggs, flaked fish like tuna or salmon, and lean ground poultry. Liquid protein sources are often better tolerated than dense solid foods when gastrointestinal side effects are prominent.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.