LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Is compounded semaglutide effective for weight loss and diabetes management? This question has become increasingly relevant as compounded versions of this GLP-1 medication have emerged during shortages of FDA-approved brands like Ozempic and Wegovy. While compounded semaglutide contains a similar active ingredient, it lacks the rigorous testing and FDA approval that pharmaceutical-grade products undergo. Understanding the differences between compounded and FDA-approved formulations is essential for patients and healthcare providers making informed treatment decisions. This article examines the available evidence, safety concerns, regulatory distinctions, and expert perspectives on compounded semaglutide effectiveness.
Quick Answer: Compounded semaglutide has not been proven effective through clinical trials, as no peer-reviewed studies have evaluated these formulations for bioequivalence or therapeutic outcomes compared to FDA-approved products.
Compounded semaglutide refers to custom-prepared formulations of the glucagon-like peptide-1 (GLP-1) receptor agonist semaglutide, created by compounding pharmacies rather than pharmaceutical manufacturers. These preparations emerged primarily in response to shortages of FDA-approved brand-name products (Ozempic and Wegovy).
Importantly, FDA-approved semaglutide products use semaglutide base, while compounded versions often use semaglutide sodium or semaglutide acetate salt forms. The FDA considers these salt forms to be different active ingredients that have not been proven bioequivalent to the approved formulation.
The mechanism of action for compounded semaglutide theoretically mirrors that of FDA-approved formulations. Semaglutide works by mimicking the naturally occurring GLP-1 hormone, which regulates blood glucose and appetite through multiple pathways. It stimulates insulin secretion in a glucose-dependent manner, suppresses glucagon release, slows gastric emptying, and acts on central nervous system receptors to reduce appetite and food intake. These combined effects lead to improved glycemic control in type 2 diabetes and significant weight reduction.
Compounded versions are typically prepared as subcutaneous injections, similar to brand-name products, though formulations may vary. Some compounding pharmacies produce lyophilized (freeze-dried) powder that requires reconstitution before injection, while others provide ready-to-use solutions. The dosing regimen generally follows the FDA-approved escalation schedule, starting at lower doses (0.25 mg weekly) and gradually increasing to therapeutic levels.
It is important to understand that compounded medications are not FDA-approved products. They are prepared under Section 503A or 503B of the Federal Food, Drug, and Cosmetic Act. Under these regulations, compounding pharmacies generally cannot make copies of commercially available drugs unless specific criteria are met, such as the medication being on the FDA Drug Shortage List. Patients should verify they are receiving products from a state-licensed pharmacy or FDA-registered 503B outsourcing facility and avoid formulations with nonstandard additives like vitamin B12 or peptides such as BPC-157.
Key contraindications for all semaglutide formulations include personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Semaglutide should be discontinued at least 2 months before a planned pregnancy, and it is not indicated for type 1 diabetes or for weight loss in the case of Ozempic.
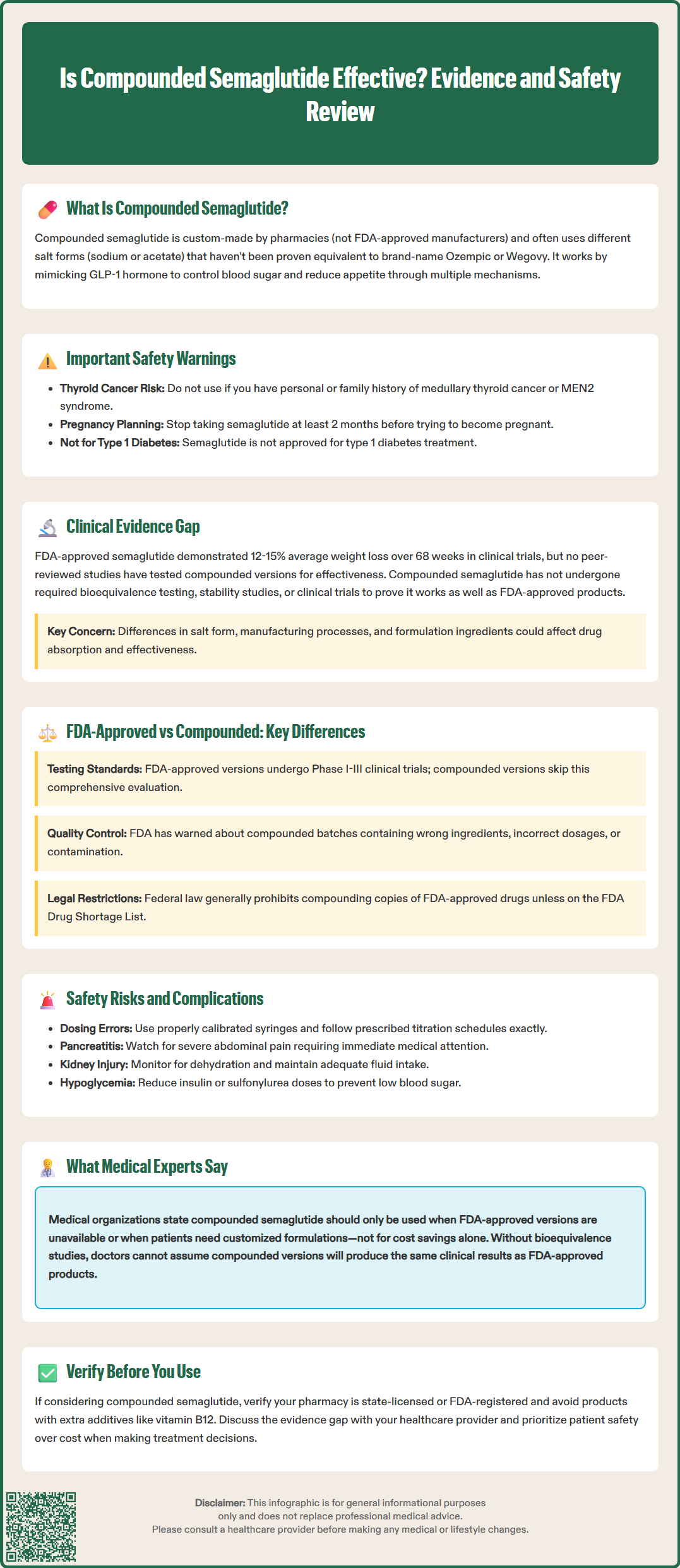
There is no peer-reviewed clinical trial data specifically evaluating the efficacy of compounded semaglutide formulations. The evidence supporting semaglutide's effectiveness comes exclusively from studies of FDA-approved products manufactured under stringent pharmaceutical standards. The landmark STEP (Semaglutide Treatment Effect in People with obesity) trials demonstrated that pharmaceutical-grade semaglutide 2.4 mg weekly produced average weight loss of 12-15% of body weight over 68 weeks, significantly outperforming placebo.
The critical question is whether compounded versions deliver equivalent therapeutic outcomes. This remains uncertain because compounded preparations have not undergone the rigorous testing required for FDA approval, including bioequivalence studies, stability testing, and clinical efficacy trials. No pharmacokinetic or bioequivalence data exist comparing compounded formulations to FDA-approved products. Variations in salt form (semaglutide sodium vs. semaglutide base), manufacturing processes, storage conditions, and formulation excipients could theoretically affect drug absorption, bioavailability, and clinical effectiveness.
Anecdotal reports and patient testimonials suggest some individuals experience weight loss with compounded semaglutide, but these accounts lack the scientific rigor necessary to establish efficacy. Without controlled studies measuring actual drug concentrations, pharmacokinetic profiles, and standardized outcome measures, it is impossible to confirm that compounded versions produce comparable results to FDA-approved products.
Healthcare providers should counsel patients that while the active pharmaceutical ingredient may be chemically similar, there is no guarantee that compounded semaglutide will deliver the same therapeutic benefits demonstrated in clinical trials. The American Society of Health-System Pharmacists (ASHP) emphasizes that compounded medications should not be considered interchangeable with FDA-approved products without appropriate evidence. Patients considering compounded semaglutide should understand this evidence gap and discuss realistic expectations with their healthcare provider.
FDA-approved semaglutide products (Ozempic for type 2 diabetes, Wegovy for weight management) undergo extensive premarket evaluation including chemistry, manufacturing, and controls review; preclinical studies; and Phase I-III clinical trials involving thousands of participants. This process ensures consistent drug quality, purity, potency, and stability. Each batch is manufactured under current Good Manufacturing Practice (cGMP) regulations with rigorous quality control testing.
Compounded semaglutide, by contrast, is not FDA-approved and does not undergo this comprehensive evaluation. Compounding pharmacies operate under different regulatory standards depending on their classification. Section 503A facilities compound medications for individual patient prescriptions and are primarily regulated by state pharmacy boards. Section 503B outsourcing facilities register with the FDA and must follow cGMP standards but still do not require premarket approval or efficacy demonstration for their compounded products.
It's important to understand that federal law generally prohibits compounding "essentially a copy" of an FDA-approved drug unless specific criteria are met, such as the medication being on the FDA Drug Shortage List or a documented patient-specific medical need for a customized formulation.
Key differences include quality assurance protocols, product consistency, and regulatory oversight. FDA-approved products must demonstrate batch-to-batch consistency, appropriate sterility for injectable products, and stability throughout the labeled shelf life. Compounded preparations may vary between batches and pharmacies, and there is limited independent verification of potency, sterility, or stability. The FDA has issued warnings about compounded semaglutide products containing incorrect ingredients, incorrect amounts of active ingredient, or contamination.
Another significant difference involves the active ingredient form. FDA-approved semaglutide products use semaglutide base, while compounded versions often use semaglutide sodium or semaglutide acetate. The FDA considers these salt forms to be different active ingredients that have not been proven bioequivalent to the approved formulation. Additionally, FDA-approved products come with comprehensive prescribing information, including detailed safety data, drug interaction profiles, and contraindications derived from extensive clinical experience. Compounded versions lack this evidence base, making risk-benefit assessment more challenging for both clinicians and patients.
The safety profile of compounded semaglutide remains inadequately characterized due to the absence of systematic post-market surveillance and adverse event reporting comparable to FDA-approved medications. While the known adverse effects of pharmaceutical-grade semaglutide are well-documented—including nausea, vomiting, diarrhea, constipation, and abdominal pain—the risk profile of compounded versions may differ due to formulation variables, impurities, or inconsistent potency.
The FDA has issued multiple warnings regarding compounded semaglutide products. Concerns include dosing errors from unclear labeling, contamination during compounding, use of incorrect salt forms, and products containing no active ingredient or excessive amounts. Dosing errors are particularly dangerous with semaglutide because the medication requires careful dose escalation to minimize gastrointestinal side effects and reduce the risk of more serious complications.
A specific safety concern involves dosing-unit confusion with multi-dose vials. Patients should never use "units" without clear mg equivalence, should use properly calibrated syringes (not insulin syringes unless specifically directed), and should follow the labeled titration schedule without accelerating dose increases.
All semaglutide formulations carry a boxed warning for thyroid C-cell tumors (seen in rodent studies) and are contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Semaglutide is not indicated for type 1 diabetes and should be discontinued at least 2 months before a planned pregnancy.
Patients should be monitored for serious adverse effects including pancreatitis (severe persistent abdominal pain), gallbladder disease (right upper quadrant pain, fever, jaundice), acute kidney injury (especially with dehydration from gastrointestinal side effects), diabetic retinopathy complications (sudden visual changes), and hypersensitivity reactions. When used with insulin or sulfonylureas, dose reductions of these medications should be considered to reduce hypoglycemia risk. Patients should not combine semaglutide with other GLP-1 receptor agonists.
Patients using compounded semaglutide should be monitored closely for adverse effects and therapeutic response. Healthcare providers should establish clear protocols for dose escalation, provide comprehensive patient education about warning signs requiring immediate medical attention, and maintain regular follow-up. Patients should be advised to report any unexpected symptoms and understand that the safety profile of their specific compounded product may not match published data for FDA-approved semaglutide. Referral to endocrinology or obesity medicine specialists should be considered for complex cases or when adverse effects occur.
Medical professional organizations and regulatory authorities have expressed significant concerns about compounded semaglutide, primarily centered on the lack of efficacy and safety data. Medical organizations emphasize that compounded medications should only be used when FDA-approved alternatives are unavailable or when a patient has a documented medical need for a customized formulation—not simply for cost savings or convenience.
Endocrinology experts note that while compounded semaglutide may contain a similar active pharmaceutical ingredient, this does not guarantee therapeutic equivalence. Without bioequivalence studies, clinicians cannot assume compounded versions will produce the same clinical outcomes as FDA-approved products. Professional medical organizations recommend that healthcare providers prioritize FDA-approved GLP-1 receptor agonists whenever possible and carefully document the rationale when prescribing compounded alternatives.
The FDA has been explicit in its position, stating that compounded drugs pose higher risks than FDA-approved drugs because they are not FDA-approved and do not undergo premarket review for safety, effectiveness, or quality. In 2023 and 2024, the FDA issued warnings to healthcare providers and patients about the risks of compounded semaglutide, particularly emphasizing concerns about dosing errors and product quality.
Clinical pharmacologists highlight that even minor differences in formulation can affect drug absorption and bioavailability. Without pharmacokinetic studies demonstrating that compounded semaglutide achieves similar blood concentrations to FDA-approved products, effectiveness remains theoretical rather than proven. The consensus among medical experts is that while compounded semaglutide may have a role during genuine drug shortages, it should not be considered a first-line option or an equivalent substitute for FDA-approved semaglutide products. Patients and providers should engage in shared decision-making that acknowledges these uncertainties and prioritizes patient safety above cost considerations alone.
There is no clinical evidence proving compounded semaglutide is as effective as FDA-approved products. Without bioequivalence studies, healthcare providers cannot confirm that compounded versions deliver the same therapeutic outcomes demonstrated in clinical trials of Ozempic and Wegovy.
Compounded semaglutide carries additional safety risks compared to FDA-approved products, including potential dosing errors, contamination, variable potency, and use of different salt forms. The FDA has issued warnings about quality concerns with compounded semaglutide products.
Medical experts recommend compounded semaglutide only when FDA-approved alternatives are genuinely unavailable due to shortages or when a documented patient-specific medical need exists for a customized formulation. Cost savings alone is not considered an appropriate reason to choose compounded over FDA-approved products.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.