LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide (Mounjaro, Zepbound) is an FDA-approved dual GIP/GLP-1 receptor agonist for type 2 diabetes and chronic weight management. Proper administration is critical for safety and efficacy. The medication is specifically formulated for subcutaneous injection only—never intramuscularly or intravenously. Injecting tirzepatide into muscle tissue instead of subcutaneous fat may alter absorption kinetics, potentially affecting therapeutic outcomes and adverse effect profiles. Understanding correct injection technique and the importance of subcutaneous delivery ensures patients achieve optimal glycemic control and weight management while minimizing risks associated with improper administration.
Quick Answer: Tirzepatide must be injected subcutaneously only, as intramuscular injection has not been studied and may alter drug absorption, efficacy, and safety profiles.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus (under the brand name Mounjaro) and chronic weight management (as Zepbound). This novel medication works by enhancing insulin secretion in a glucose-dependent manner, suppressing glucagon release, slowing gastric emptying, and reducing appetite through central nervous system pathways.
According to the FDA-approved prescribing information, tirzepatide is specifically formulated and indicated for subcutaneous injection only. The medication is supplied in single-dose prefilled pens containing 2.5 mg, 5 mg, 7.5 mg, 10 mg, 12.5 mg, or 15 mg doses. The recommended starting dose for type 2 diabetes is 2.5 mg once weekly, with gradual titration every four weeks based on glycemic response and tolerability, up to a maximum of 15 mg weekly. For chronic weight management, the same starting dose and titration schedule apply.
The approved injection sites include the abdomen, thigh, or upper arm. Upper arm injections should be administered by a caregiver. Patients should rotate injection sites with each dose to reduce local irritation and avoid using the same site repeatedly. Tirzepatide should be administered on the same day each week, and the day of weekly administration can be changed if necessary, provided at least three days (72 hours) have elapsed between doses.
If a dose is missed, it should be administered within 4 days of the scheduled dose. If more than 4 days have passed, skip the missed dose and administer the next dose on the regularly scheduled day.
It is critical that healthcare providers educate patients on proper administration technique during initiation. The medication must never be administered intravenously or intramuscularly, as these routes have not been studied and may alter the drug's pharmacokinetic profile, efficacy, and safety.
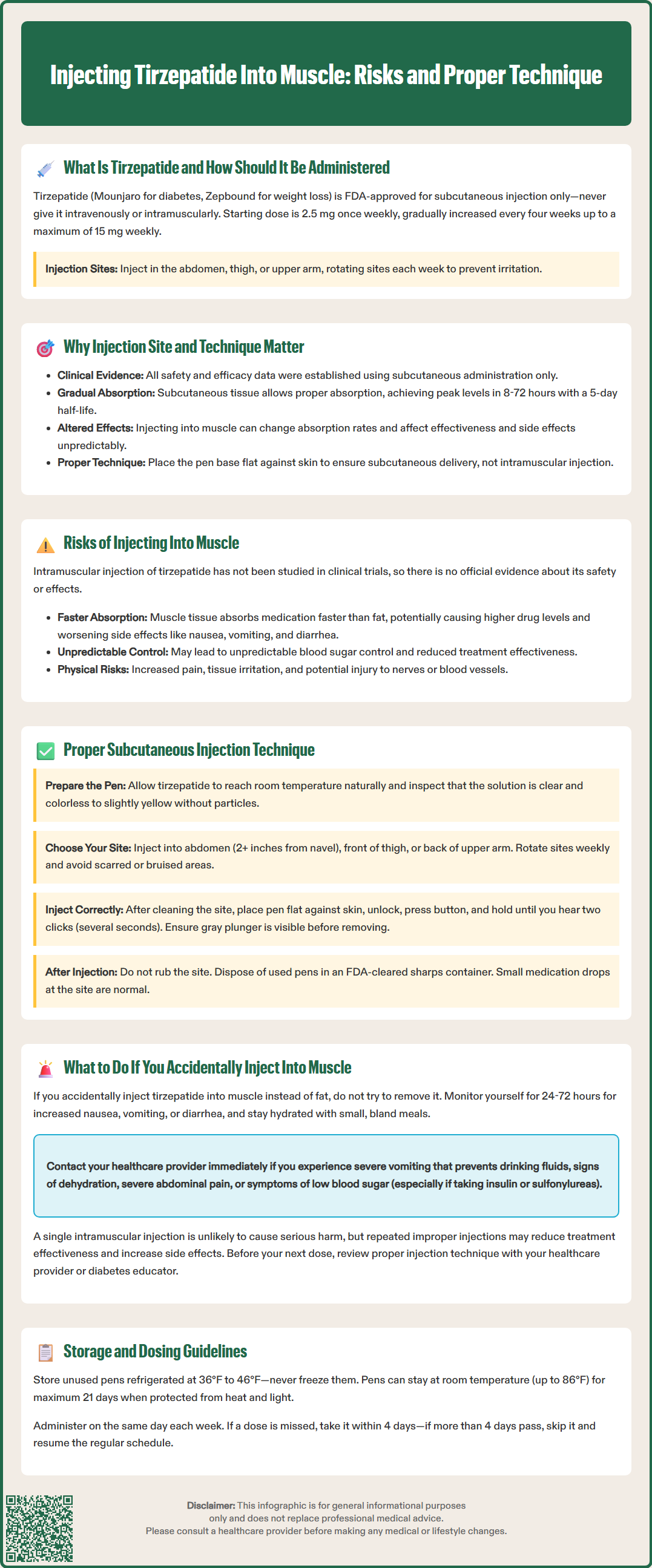
The subcutaneous route of administration is essential for tirzepatide because the medication's pharmacokinetic properties—including absorption rate, bioavailability, and duration of action—were established through subcutaneous delivery in all clinical trials. Subcutaneous tissue provides a relatively avascular depot from which the large peptide molecule (molecular weight approximately 4,813 Da) is gradually absorbed into systemic circulation, achieving peak plasma concentrations approximately 8 to 72 hours post-injection, according to the FDA prescribing information.
This controlled absorption profile is fundamental to tirzepatide's once-weekly dosing schedule and its favorable efficacy and tolerability profile. The medication's half-life of approximately five days allows for steady-state concentrations to be achieved after four weeks of weekly dosing, providing consistent glycemic control and weight reduction effects throughout the dosing interval.
Proper injection technique matters for several reasons:
Predictable absorption: Subcutaneous fat provides consistent drug absorption, whereas muscle tissue has different vascularity and may alter absorption kinetics
Safety profile: All safety data from clinical trials reflect subcutaneous administration; alternative routes have unknown safety implications
Efficacy: The dose-response relationship established in trials assumes subcutaneous delivery
Tolerability: Gastrointestinal adverse effects (nausea, vomiting, diarrhea) are dose-dependent and may be affected by altered absorption
Patients with lower body mass index or those injecting in areas with less subcutaneous fat may be at higher risk of inadvertent intramuscular injection if proper technique is not followed. Following the device-specific Instructions for Use, which directs users to place the pen base flat against the skin, is the primary method to ensure subcutaneous delivery. Healthcare providers should assess individual patient anatomy and provide tailored education on appropriate injection sites and proper pen use.
While there is limited published data specifically examining intramuscular administration of tirzepatide, extrapolation from pharmacokinetic principles and experience with other subcutaneous medications suggests several potential concerns. It is important to note that there is no official evidence base establishing definitive harm from accidental intramuscular injection, as this route has not been systematically studied in clinical trials.
Intramuscular tissue is more highly vascularized than subcutaneous fat, which theoretically could lead to more rapid absorption of tirzepatide. Faster absorption might result in higher peak plasma concentrations than intended, potentially increasing the risk or severity of dose-dependent adverse effects, particularly gastrointestinal symptoms such as nausea, vomiting, and diarrhea. These effects are already among the most common reasons for treatment discontinuation in clinical trials.
Additionally, altered pharmacokinetics could theoretically affect the medication's duration of action, though the clinical significance of this is uncertain given tirzepatide's long half-life. There is also a theoretical concern that intramuscular injection might cause local tissue irritation or injection site reactions, though tirzepatide generally has a relatively low incidence of injection site adverse events in clinical trials.
Other potential concerns include:
Unpredictable glycemic effects due to altered absorption patterns
Increased injection site pain or discomfort
Possible nerve or blood vessel injury with deeper injection
Deviation from the evidence-based administration method
Patients who consistently inject into muscle rather than subcutaneous tissue may not achieve the expected therapeutic outcomes, as the dose-response relationship has only been established for subcutaneous administration. Healthcare providers should emphasize that following FDA-approved administration guidelines is essential for both safety and efficacy.
Correct subcutaneous injection technique is essential for safe and effective tirzepatide administration. Healthcare providers should provide hands-on training during treatment initiation and periodically reassess technique at follow-up visits.
Step-by-step subcutaneous injection technique:
Preparation: Remove the tirzepatide pen from the refrigerator and allow it to reach room temperature naturally (do not warm by other methods). Inspect the solution through the pen window—it should be clear and colorless to slightly yellow. Do not use if the solution is cloudy, discolored, or contains particles.
Site selection: Choose an injection site on the abdomen (at least 2 inches away from the navel), front of the thigh, or back of the upper arm. Upper arm injections should be administered by a caregiver. Rotate sites weekly to reduce local irritation. Avoid areas with scars, bruises, or skin abnormalities.
Injection technique: Cleanse the injection site with an alcohol swab and allow to dry. Remove the pen cap. Place the clear base flat against your skin. Unlock the pen by turning the lock ring. Press and hold the injection button until you hear the clicks. The first click signals the beginning of the injection; continue holding until you hear the second click, which indicates the injection is complete. This typically takes several seconds. Remove the pen only after the gray plunger is visible in the indicator window.
Post-injection: Do not rub the injection site. Dispose of the used pen in an FDA-cleared sharps container. If a drop of medication appears at the injection site, this is normal and does not significantly affect the dose received.
Storage and handling:
Store unused pens in the refrigerator (36°F to 46°F or 2°C to 8°C)
Do not freeze; discard if the pen has been frozen
Pens can be stored at room temperature (up to 86°F or 30°C) for up to 21 days
Protect from direct heat and light
For the most current and detailed instructions, always refer to the Instructions for Use provided with your medication.
If you suspect you have accidentally injected tirzepatide into muscle tissue rather than subcutaneous fat, it is important to remain calm and take appropriate monitoring steps. Signs that might suggest intramuscular injection include injection in an area with minimal subcutaneous fat or not following the device's Instructions for Use.
Immediate steps:
Do not attempt to remove or "correct" the injection—the medication has already been administered. Monitor for adverse effects over the next 24-72 hours, particularly gastrointestinal symptoms such as nausea, vomiting, or diarrhea, which might be more pronounced if absorption was more rapid than intended. Stay well-hydrated and eat small, bland meals if nausea occurs.
When to contact your healthcare provider:
Severe or persistent nausea and vomiting that prevents adequate oral intake
Signs of dehydration (decreased urination, dizziness, dry mouth)
Severe abdominal pain, especially if persistent or radiating to the back
Symptoms of hypoglycemia if taking tirzepatide with insulin or sulfonylureas (shakiness, sweating, confusion, rapid heartbeat)
Unusual injection site reactions (severe pain, swelling, redness)
Intractable vomiting or inability to keep fluids down
Any other concerning symptoms
For future injections:
Review proper injection technique with your healthcare provider or a diabetes educator before your next dose. Request a supervised injection if you are uncertain about your technique. Consider using injection sites with more abundant subcutaneous tissue, such as the abdomen. Ensure you are following the specific Instructions for Use for your tirzepatide pen.
Important safety note: A single accidental intramuscular injection is unlikely to cause serious harm, but consistent improper technique may affect treatment efficacy and increase adverse effect risk. For guidance on your next scheduled dose, contact your healthcare provider for individualized advice, especially if you take insulin or sulfonylureas. Document the incident and discuss it at your next appointment to prevent recurrence.
No, tirzepatide is FDA-approved for subcutaneous injection only. Intramuscular administration has not been studied and may alter the medication's absorption, efficacy, and safety profile.
Monitor for increased gastrointestinal symptoms such as nausea or vomiting over 24-72 hours, stay hydrated, and contact your healthcare provider if you experience severe or persistent symptoms. Review proper subcutaneous injection technique before your next dose.
Place the pen base flat against your skin as directed in the Instructions for Use, choose injection sites with adequate subcutaneous fat (abdomen, thigh, or upper arm), and rotate sites weekly. Request supervised injection training from your healthcare provider if uncertain about technique.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.