LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Semaglutide, marketed as Ozempic, Wegovy, and Rybelsus, is an FDA-approved GLP-1 receptor agonist used for type 2 diabetes management and chronic weight management. As its use has expanded, questions have emerged about potential side effects, including concerns about semaglutide and blood clots. Understanding the relationship between this medication and thrombotic risk is essential for patients and healthcare providers. Current clinical evidence does not establish a causal link between semaglutide use and increased blood clot formation, though patients prescribed this medication often have underlying conditions that independently elevate thrombotic risk. This article examines the available research, risk factors, and important safety considerations.
Quick Answer: Current clinical evidence does not establish a causal relationship between semaglutide use and increased blood clot formation.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for two primary indications: type 2 diabetes management and chronic weight management in adults with obesity or overweight with at least one weight-related comorbidity. It's marketed under brand names including Ozempic (injectable for diabetes), Wegovy (injectable for weight management), and Rybelsus (oral tablet for diabetes).
The medication works by mimicking the action of naturally occurring GLP-1, a hormone released by the intestines after eating. Semaglutide binds to GLP-1 receptors in multiple tissues, triggering several physiological responses. In the pancreas, it stimulates glucose-dependent insulin secretion and suppresses inappropriate glucagon release, thereby improving glycemic control. In the brain, particularly in appetite-regulating centers, it reduces hunger signals and increases satiety. Additionally, semaglutide slows gastric emptying, which contributes to prolonged feelings of fullness after meals.
Injectable semaglutide is administered as a once-weekly subcutaneous injection, with a half-life of approximately one week. The medication is initiated at a low dose (typically 0.25 mg weekly) and gradually titrated upward over several weeks to minimize gastrointestinal side effects. For diabetes management, the maintenance dose ranges from 0.5 mg to 2 mg weekly, while weight management protocols may use doses up to 2.4 mg weekly.
Clinical trials have demonstrated significant benefits, including HbA1c reductions of 1.5-2% in patients with type 2 diabetes and weight loss averaging 10-15% of body weight in obesity treatment studies with Wegovy 2.4 mg.
Importantly, semaglutide carries a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Semaglutide should be discontinued when pregnancy is recognized and at least 2 months before a planned pregnancy due to its long half-life. Other important safety considerations include risk of diabetic retinopathy complications, gallbladder disease, and acute kidney injury.
Currently, there is no established causal relationship between semaglutide use and increased blood clot formation based on available clinical evidence. The FDA-approved prescribing information for semaglutide does not list thrombotic events or venous thromboembolism (VTE) as recognized adverse effects of the medication. Large-scale randomized controlled trials, including the SUSTAIN and STEP trial series, have not identified elevated rates of blood clots among semaglutide users compared to placebo groups.
The cardiovascular outcomes trial SUSTAIN-6, which enrolled over 3,000 patients with type 2 diabetes at high cardiovascular risk, actually demonstrated cardiovascular benefits with semaglutide, including reduced rates of major adverse cardiovascular events. More recently, the SELECT trial showed that Wegovy significantly reduced the risk of major adverse cardiovascular events in adults with established cardiovascular disease and overweight or obesity without diabetes, leading to an FDA-approved cardiovascular risk reduction indication. Importantly, these trials have not shown increased incidence of deep vein thrombosis (DVT), pulmonary embolism (PE), or arterial thrombotic events attributable to the medication itself.
However, it is important to recognize that patients prescribed semaglutide often have underlying conditions that independently increase thrombotic risk. Type 2 diabetes, obesity, and metabolic syndrome are all established risk factors for venous and arterial thromboembolism.
Some case reports and post-marketing surveillance data have documented thrombotic events in patients taking semaglutide, but these observations do not establish causation. The American Diabetes Association and American College of Physicians guidelines do not recommend specific thrombosis monitoring or prophylaxis for patients on GLP-1 receptor agonists. Ongoing pharmacovigilance continues to monitor for any emerging safety signals, but current evidence does not support a direct mechanistic link between semaglutide and blood clot formation.
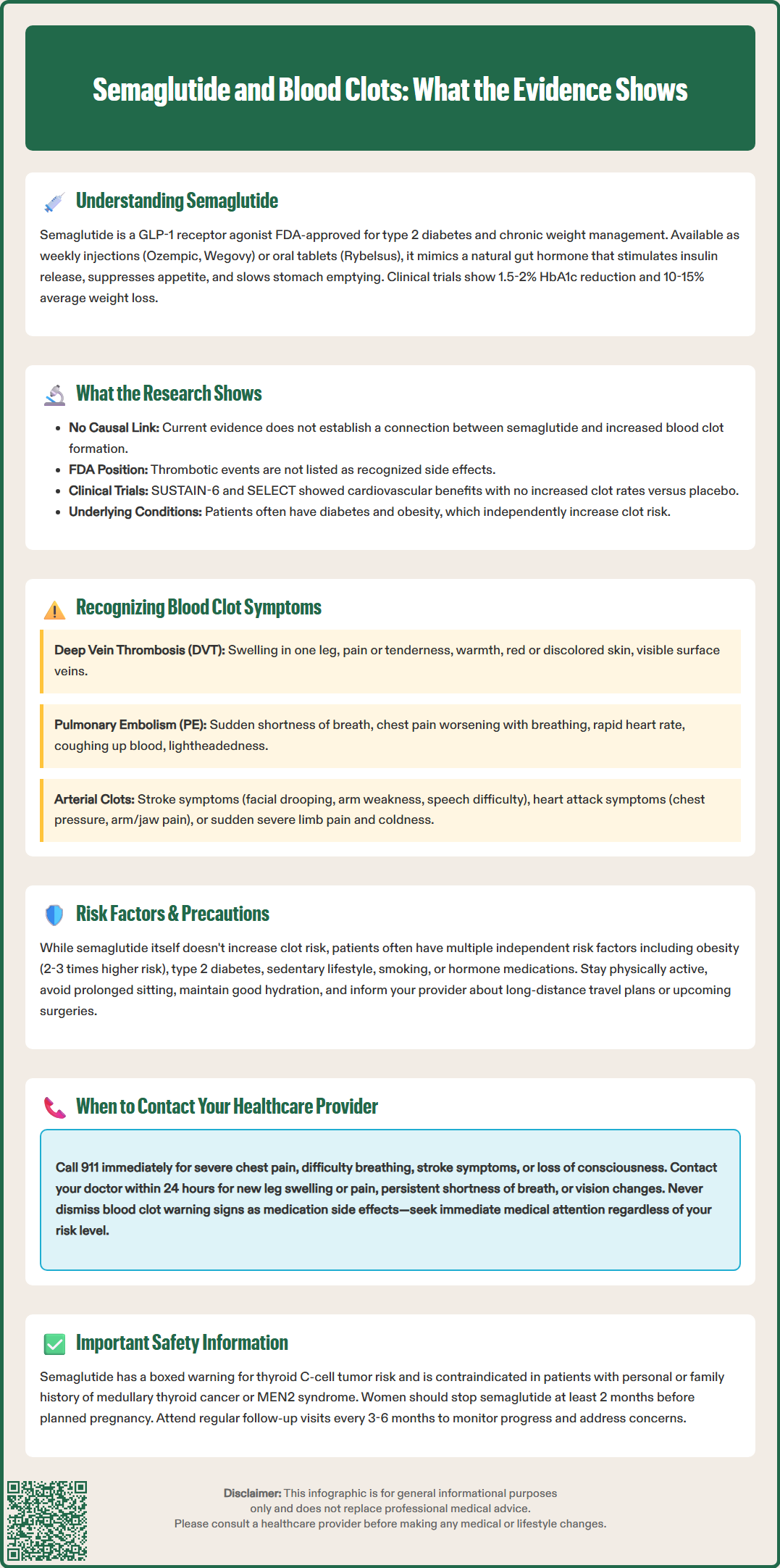
Regardless of medication use, all patients should be educated about the warning signs of blood clots, as early recognition and treatment are critical for preventing serious complications. Blood clots can occur in veins (venous thromboembolism) or arteries (arterial thrombosis), each presenting with distinct symptom patterns.
Deep vein thrombosis (DVT) typically affects the legs and may cause:
Swelling in one leg, often starting in the calf
Pain or tenderness, sometimes described as cramping or soreness
Warmth in the affected area
Red or discolored skin
Visible surface veins
Pulmonary embolism (PE), which occurs when a clot travels to the lungs, presents with more acute symptoms:
Sudden shortness of breath or difficulty breathing
Chest pain that worsens with deep breathing or coughing
Rapid heart rate or palpitations
Coughing up blood
Lightheadedness or fainting
Arterial thrombosis symptoms depend on the affected vessel but may include sudden onset of stroke symptoms (facial drooping, arm weakness, speech difficulty, sudden vision loss, severe headache), heart attack symptoms (chest pressure, arm or jaw pain, nausea), or acute limb ischemia (sudden severe pain, pallor, and coldness in an extremity).
Patients taking semaglutide should not attribute these symptoms to medication side effects or dismiss them as minor concerns. While gastrointestinal symptoms like nausea and abdominal discomfort are common with semaglutide, the symptoms described above are not typical medication effects and warrant immediate medical evaluation. The presence of multiple risk factors for thrombosis should heighten awareness, but symptoms should never be ignored regardless of perceived risk level.
While semaglutide itself has not been linked to increased clotting risk, patients prescribed this medication often have multiple independent risk factors for thromboembolism that require clinical attention. Understanding these risk factors helps both patients and healthcare providers make informed decisions about monitoring and prevention strategies.
Established thrombotic risk factors commonly present in semaglutide users include:
Obesity (BMI ≥30 kg/m²), which increases VTE risk 2-3 fold
Type 2 diabetes and insulin resistance
Prolonged immobility or sedentary lifestyle
History of previous blood clots
Active cancer or recent cancer treatment
Recent surgery, particularly orthopedic or abdominal procedures
Smoking
Certain medications, including estrogen-containing contraceptives or hormone replacement therapy
Inherited thrombophilias (clotting disorders)
Advanced age (risk increases after age 60)
Pregnancy and postpartum period (note that semaglutide should be discontinued when pregnancy is recognized)
Patients initiating semaglutide should undergo comprehensive baseline assessment including medical history review, with particular attention to prior thrombotic events and family history of clotting disorders. For patients with multiple risk factors or previous VTE, healthcare providers may consider additional precautions, though these relate to underlying conditions rather than semaglutide specifically.
Practical precautions for all patients include:
Maintaining adequate hydration as part of overall health
Staying physically active and avoiding prolonged immobility
Continuing prescribed anticoagulation if already indicated for other conditions
Discussing travel plans, as long flights or car trips may require movement strategies
Reporting any new medications or supplements to healthcare providers
For patients undergoing elective surgery while taking semaglutide, discussion with both the prescribing physician and surgeon is important regarding perioperative management. Current multi-society guidelines (including the American Society of Anesthesiologists) provide risk-based recommendations on whether to continue or temporarily hold GLP-1 receptor agonists before procedures, primarily addressing concerns about glycemic management and aspiration risk.
Patients taking semaglutide should maintain open communication with their healthcare team and understand which symptoms require urgent versus routine medical attention. Clear guidance on when to seek care promotes both safety and appropriate healthcare utilization.
Seek immediate emergency care (call 911 or go to the emergency department) for:
Sudden severe chest pain or pressure
Difficulty breathing or shortness of breath at rest
Coughing up blood
Sudden weakness, numbness, difficulty speaking, vision changes, or severe headache (stroke symptoms)
Severe leg pain with swelling and skin color changes
Fainting or loss of consciousness
Sudden severe abdominal pain (which could indicate pancreatitis, a known rare semaglutide risk)
Signs of severe allergic reaction (rash, itching, swelling of face/throat, difficulty breathing)
Contact your healthcare provider within 24 hours for:
New or worsening leg swelling, especially if unilateral
Persistent calf pain or tenderness
Unexplained shortness of breath with exertion
New onset of rapid heart rate
Persistent severe nausea or vomiting preventing adequate hydration
Sudden vision changes (potential retinopathy complication)
Right upper quadrant pain, fever, or yellowing of skin/eyes (potential gallbladder disease)
Markedly decreased urination (potential kidney issue)
Positive pregnancy test (semaglutide should be discontinued)
Schedule a routine appointment to discuss:
Planned surgeries or procedures
New medications or supplements
Significant changes in activity level or mobility
Pregnancy planning (semaglutide should be discontinued at least 2 months before planned conception)
Concerns about medication side effects
Difficulty with injection technique or medication adherence
Patients should generally not discontinue semaglutide abruptly without medical guidance, as this may affect glycemic control in those with diabetes. However, exceptions include pregnancy, suspected serious adverse reactions (pancreatitis, gallbladder disease, severe allergic reactions), or as directed before certain procedures. If concerns arise about any aspect of treatment, discussion with the prescribing provider allows for informed decision-making about continuing, adjusting, or discontinuing therapy.
Regular follow-up appointments are important—typically every 3 months if therapy is being adjusted or treatment goals aren't met, and up to every 6 months for stable patients. These visits provide opportunities to reassess treatment goals and address emerging concerns.
No, current clinical evidence does not establish a causal relationship between semaglutide and blood clot formation. Large-scale trials have not shown increased rates of thrombotic events compared to placebo, and the FDA prescribing information does not list blood clots as a recognized adverse effect.
Warning signs include sudden leg swelling with pain and warmth, sudden shortness of breath or chest pain, coughing up blood, or stroke symptoms like facial drooping and speech difficulty. These symptoms require immediate emergency medical evaluation regardless of medication use.
While semaglutide itself has not been linked to increased clotting risk, patients prescribed this medication often have underlying conditions like obesity and diabetes that independently increase thrombotic risk. Discuss your individual risk factors with your healthcare provider and maintain awareness of blood clot warning signs.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.