LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Pain at injection site semaglutide is a recognized local adverse reaction affecting approximately 1.2-1.4% of patients using this GLP-1 receptor agonist for type 2 diabetes or weight management. While typically mild and transient, injection site discomfort can impact treatment adherence and patient experience. Understanding the mechanisms behind this reaction—including tissue distension, preservative irritation, and injection technique factors—empowers patients and clinicians to minimize discomfort through evidence-based strategies. This article examines why semaglutide injections cause pain, how common this reaction is, proven techniques to reduce discomfort, and when medical evaluation becomes necessary.
Quick Answer: Pain at the semaglutide injection site occurs in approximately 1.2-1.4% of patients and typically results from tissue distension, preservative irritation, and injection technique factors.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist administered subcutaneously for type 2 diabetes management (Ozempic) and chronic weight management (Wegovy). Pain at the injection site represents a recognized local adverse reaction that occurs through several mechanisms.
The subcutaneous injection introduces a small volume of solution into the tissue beneath the skin, which can cause mechanical tissue distension and activate local nociceptors. Semaglutide formulations contain different excipients depending on the product. Ozempic (multi-dose pen) contains disodium phosphate dihydrate and phenol as a preservative, while Wegovy (single-dose pen) has a different formulation. Preservatives, while necessary for maintaining sterility in multi-dose pens, may contribute to localized tissue irritation and injection discomfort.
Additional factors influencing injection site pain include needle gauge, injection technique, injection speed, and individual patient characteristics such as subcutaneous tissue thickness and pain sensitivity. Cold medication injected directly from refrigerated storage may cause more discomfort than medication allowed to reach room temperature according to product storage instructions. Injection into areas with less subcutaneous fat or closer proximity to nerve endings may also increase pain perception.
The body's response to the injection itself can produce tenderness, erythema, or mild swelling that persists after administration. Understanding these mechanisms helps clinicians counsel patients on expected sensations versus concerning reactions requiring further evaluation.
Importantly, patients should never share pens or needles due to infection risk, and should not use the medication if the solution appears discolored or contains particles.
According to FDA prescribing information, injection site reactions occur in a measurable proportion of patients receiving semaglutide. In the SUSTAIN clinical trial program evaluating Ozempic for type 2 diabetes, injection site reactions were reported in 1.2-1.4% of patients receiving semaglutide compared to 0.7% receiving placebo. These reactions were generally mild to moderate in severity.
For Wegovy (higher-dose semaglutide for weight management), the STEP clinical trials reported injection site reactions in 1.4% of participants. The definition of injection site reactions in clinical trials typically includes pain, erythema, pruritus, and other local symptoms that patients report to investigators.
It is important to distinguish between transient injection discomfort—a brief stinging or pressure sensation during or immediately after injection—and persistent injection site pain lasting hours or days. Brief discomfort is common with subcutaneous injections. Patients should inform their healthcare providers about persistent or bothersome injection site reactions, as these may require evaluation or management.
Many patients who experience initial injection site discomfort report improvement with subsequent injections as technique improves and tissue adaptation occurs. Severe or persistent injection site reactions leading to treatment discontinuation are uncommon in clinical trials. Individual pain thresholds and anxiety about self-injection may influence subjective reporting of injection site discomfort.
If patients experience concerning or persistent injection site reactions, they should discuss these with their healthcare provider rather than assuming such reactions are too minor to report.
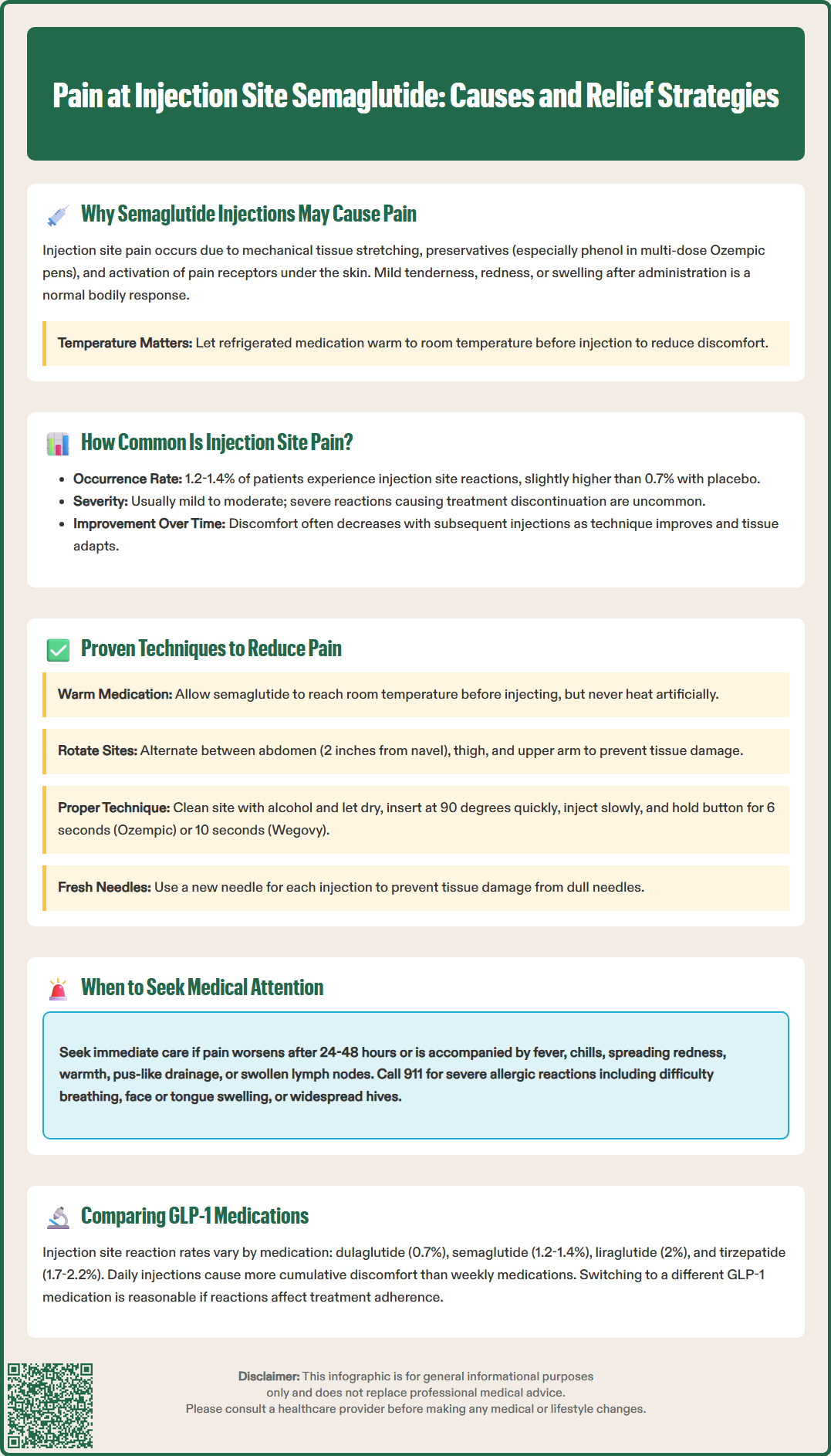
Evidence-based injection techniques can significantly reduce pain and improve patient experience with semaglutide administration. Temperature optimization represents a simple but effective intervention: allowing the medication to reach room temperature according to the product's Instructions for Use may reduce cold-induced discomfort. The medication should never be heated artificially or exposed to direct sunlight.
Proper injection site selection and rotation minimizes tissue trauma and prevents lipohypertrophy. Recommended sites include the abdomen (avoiding a 2-inch radius around the navel), anterior and lateral thigh, and upper outer arm. Note that upper arm injections may require assistance from another person. Rotating injection sites with each dose—rather than using the same location repeatedly—allows tissue recovery and reduces cumulative irritation. Patients should avoid injecting into areas with visible scarring, bruising, or skin abnormalities.
Injection technique refinements include:
Cleaning the injection site with alcohol and allowing it to dry completely before injection (wet alcohol can cause stinging)
Pinching the skin gently to create a subcutaneous tissue fold without excessive pressure
Inserting the needle at a 90-degree angle with a quick, smooth motion
Injecting slowly and steadily according to the device Instructions for Use
Maintaining pressure on the injection button for the recommended time (approximately 6 seconds for Ozempic; 10 seconds for Wegovy) before withdrawing the needle
Releasing the skin pinch before withdrawing the needle
Avoiding massage or rubbing of the injection site immediately after administration
Needle considerations may also impact comfort. Ozempic requires attaching a new pen needle for each injection, while Wegovy has an integrated needle in its single-dose pen. Using a new needle for each injection prevents tissue damage from dull or bent needles. Some patients report reduced discomfort when injecting into areas with more subcutaneous fat, such as the abdomen, compared to leaner areas like the thigh.
For patients with significant injection anxiety, distraction techniques, topical numbing agents (after consultation with a healthcare provider), or ice application before injection may provide additional comfort. However, ice should be used cautiously as excessive cooling can cause vasoconstriction.
Proper sharps disposal is essential for safety. Used needles and pens should be placed in an FDA-cleared sharps disposal container, following local regulations for disposal.
While mild injection site discomfort is expected and generally benign, certain presentations warrant prompt medical evaluation. Severe or worsening pain that intensifies over 24-48 hours rather than improving suggests possible complications beyond normal injection site reactions. Pain accompanied by systemic symptoms—including fever, chills, malaise, or regional lymphadenopathy—raises concern for injection site infection (cellulitis or abscess formation) requiring antibiotic therapy.
Local signs of infection include progressive erythema extending beyond the immediate injection site, warmth, fluctuance suggesting abscess formation, or purulent drainage. While sterile technique and single-use needles minimize infection risk, any breach in skin integrity creates potential for bacterial entry. Patients with poorly controlled diabetes may have increased infection susceptibility and should maintain heightened vigilance.
Allergic or hypersensitivity reactions present differently from mechanical injection site pain. Concerning features include extensive urticaria, significant swelling beyond the injection site, intense pruritus, or rapid onset of symptoms. Immediate hypersensitivity reactions—though rare with semaglutide—may include angioedema, bronchospasm, or anaphylaxis. If signs of severe allergic reaction occur (difficulty breathing, facial/tongue swelling, severe rash), call 911 immediately.
Injection site nodules or persistent induration lasting beyond one week may indicate lipohypertrophy, sterile abscess formation, or rarely, localized inflammatory reactions. These findings warrant clinical examination to determine appropriate management, which may include temporary cessation of injections at the affected site or diagnostic imaging if abscess is suspected.
Patients should also seek medical advice if injection site reactions lead to inability to continue treatment, if pain significantly impacts daily activities, or if there is uncertainty about whether symptoms represent normal reactions versus complications. Patients should avoid injecting into affected areas until evaluated by a healthcare provider.
Significant adverse events related to injection site reactions should be reported to the FDA MedWatch program (www.fda.gov/medwatch) in addition to informing the prescribing healthcare provider.
Injection site reactions vary across the GLP-1 receptor agonist class based on formulation characteristics, injection frequency, and dosing volumes. Semaglutide (Ozempic, Wegovy) administered once weekly demonstrates injection site reaction rates of 1.2-1.4% according to FDA prescribing information.
Dulaglutide (Trulicity), another once-weekly GLP-1 agonist, reports injection site reaction rates of approximately 0.7% in its FDA label. Both medications benefit from reduced injection frequency, allowing tissue recovery between doses. Dulaglutide uses a single-dose pen with an automated injection mechanism that differs from semaglutide pens.
Liraglutide (Victoza, Saxenda), administered daily, demonstrates injection site reaction rates of approximately 2% in its FDA prescribing information. More frequent injections increase cumulative exposure to injection-related discomfort. Proper site rotation becomes particularly important with daily injections to prevent localized tissue changes.
Exenatide formulations show variable injection site tolerability. Extended-release exenatide (Bydureon BCise), given weekly, uses a microsphere suspension that may cause more injection site nodules (reported in 10.5% of patients according to its FDA label) compared to solution-based formulations.
Tirzepatide (Mounjaro, Zepbound), a dual GIP/GLP-1 receptor agonist, reports injection site reaction rates of approximately 1.7-2.2% in its FDA prescribing information, similar to semaglutide.
Formulation factors influencing injection site reactions include preservative content, solution characteristics, and injection volume. Suspension formulations generally cause more injection site reactions than clear solutions due to particulate matter. Individual patient responses vary considerably, and some patients who experience significant injection site reactions with one GLP-1 medication may tolerate another formulation better. When injection site reactions significantly impact treatment adherence, discussing alternative GLP-1 options with healthcare providers represents a reasonable approach, as therapeutic efficacy across the class often allows successful substitution while maintaining glycemic control or weight management benefits.
It's important to note that FDA-approved GLP-1 medications have undergone rigorous testing for safety and efficacy, including evaluation of injection site tolerability. Compounded semaglutide products are not FDA-approved and may have different excipient profiles and reaction patterns.
Most patients experience brief discomfort during or immediately after injection that resolves within minutes to hours. Mild tenderness may persist for 1-2 days but should gradually improve. Pain lasting beyond 48 hours or worsening over time warrants medical evaluation.
Ice application before injection may provide comfort for some patients, though excessive cooling can cause vasoconstriction. Topical numbing agents should only be used after consultation with your healthcare provider to ensure they don't interfere with medication absorption or cause additional skin reactions.
Yes, rotating injection sites with each dose is recommended to allow tissue recovery and minimize cumulative irritation. If one anatomical area (abdomen, thigh, or upper arm) consistently causes more discomfort, focus on the better-tolerated sites while maintaining proper rotation within that area.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.