LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Should you take GLP-1 shots on an empty stomach? For most long-acting GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and tirzepatide (Mounjaro, Zepbound), the answer is no—food timing doesn't matter. These subcutaneous injections can be administered with or without food, as stomach contents don't affect their absorption or efficacy. However, short-acting agents like exenatide (Byetta) require specific meal-related timing. Understanding the correct administration guidelines for your particular GLP-1 medication ensures optimal treatment outcomes while managing type 2 diabetes or chronic weight. This guide clarifies FDA-approved timing recommendations and best practices for GLP-1 injection use.
Quick Answer: Most long-acting GLP-1 injections can be taken with or without food, as stomach contents do not affect their subcutaneous absorption or efficacy.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists are injectable medications approved by the FDA for managing type 2 diabetes and, in some formulations, chronic weight management. These medications include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), and exenatide (Byetta), among others. Tirzepatide (Mounjaro, Zepbound) works as a dual GIP/GLP-1 receptor agonist with a slightly different mechanism. These agents mimic the action of naturally occurring incretin hormones released by the intestine in response to food intake.
GLP-1 receptor agonists work through several complementary mechanisms. They enhance glucose-dependent insulin secretion from pancreatic beta cells, meaning insulin is released primarily when blood glucose levels are elevated, which reduces the risk of hypoglycemia compared to some other diabetes medications. These agents also suppress glucagon secretion from pancreatic alpha cells, further helping to lower blood glucose levels. Additionally, they slow gastric emptying, which prolongs the sensation of fullness after meals and contributes to reduced caloric intake.
The weight loss effects observed with these medications result from both delayed gastric emptying and direct effects on appetite centers in the hypothalamus, leading to reduced hunger and increased satiety. According to the American Diabetes Association (ADA) Standards of Care, GLP-1 receptor agonists with proven cardiovascular benefit are recommended for many patients with type 2 diabetes who have established cardiovascular disease, with individualized therapy based on patient factors. The pharmacokinetic profiles vary among different agents, with some administered daily and others weekly.
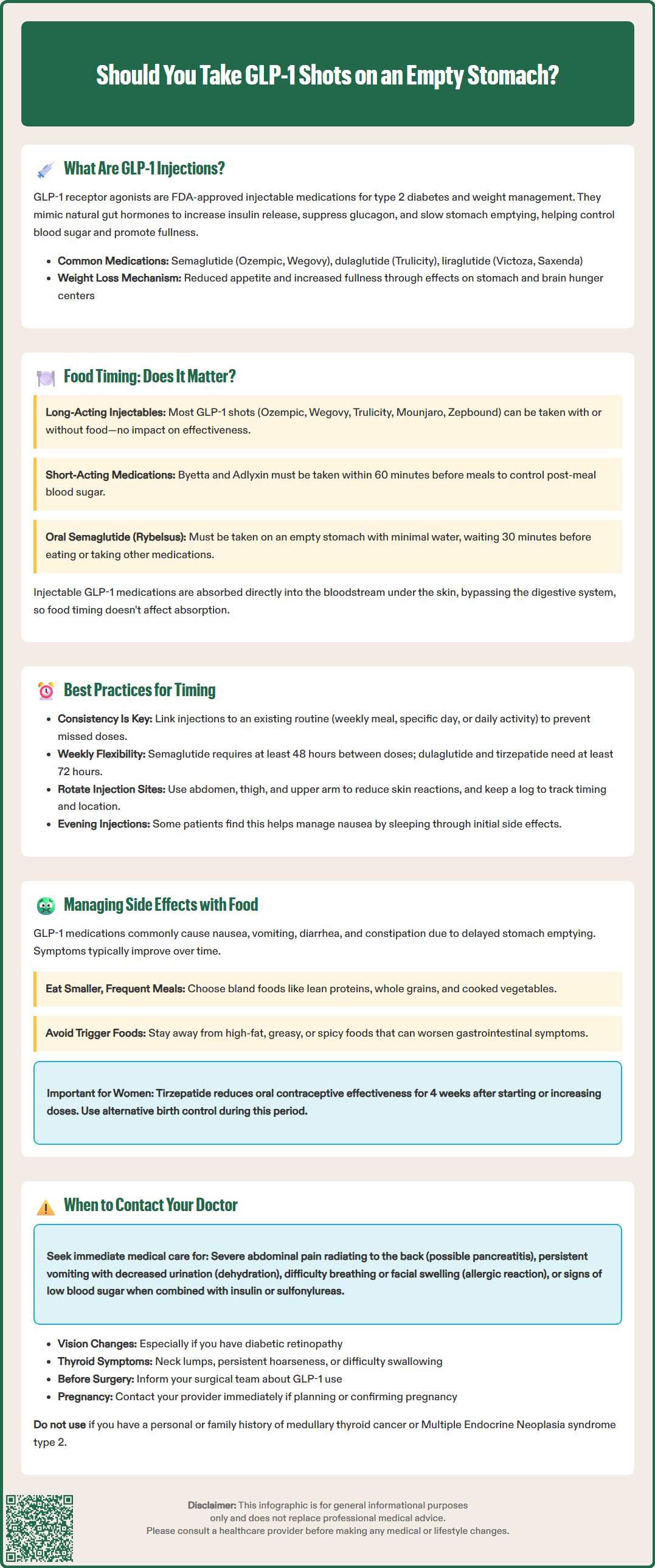
The answer depends on which specific GLP-1 medication you're using. Most long-acting injectable GLP-1 receptor agonists can be administered with or without food—there is no requirement to take them on an empty stomach. According to FDA-approved prescribing information for semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), and tirzepatide (Mounjaro, Zepbound), food intake does not significantly affect the absorption or efficacy of these subcutaneous injections.
However, there are important exceptions. Short-acting GLP-1 receptor agonists such as exenatide immediate-release (Byetta) and lixisenatide (Adlyxin) must be administered within 60 minutes before meals. These medications are specifically designed to target postprandial glucose control and require meal-related timing.
For the long-acting injectables, because they are administered subcutaneously (under the skin) rather than orally, they bypass the gastrointestinal absorption process that can be influenced by stomach contents. The medication is absorbed directly into the bloodstream from subcutaneous tissue, making the presence or absence of food in the stomach clinically irrelevant to drug pharmacokinetics.
Patients using long-acting GLP-1 injectables should focus on consistency and convenience rather than food timing when scheduling their injections. The American College of Physicians (ACP) and ADA guidelines emphasize medication adherence as a critical factor in achieving glycemic control and weight management goals.
It is worth noting that the oral formulation of semaglutide (Rybelsus) does require specific administration instructions, including taking it on an empty stomach with no more than 4 ounces of water and waiting 30 minutes before eating, drinking, or taking other oral medications. However, this guidance applies exclusively to the oral tablet and not to any injectable GLP-1 formulations.
While food timing is not a medical requirement for most GLP-1 injections, establishing a consistent routine optimizes treatment outcomes and minimizes the risk of missed doses. Choose a specific day and time for weekly injections or a consistent time each day for daily formulations. Many patients find it helpful to link their injection schedule to an existing routine, such as a weekly meal, a specific day of the week, or a daily activity.
For weekly GLP-1 injections, the FDA labeling permits some flexibility in timing, but this varies by product. If you need to change your regular injection day for semaglutide (Ozempic, Wegovy), you may do so as long as the new dose is administered at least 48 hours (2 days) after the previous injection. For dulaglutide (Trulicity) and tirzepatide (Mounjaro, Zepbound), at least 72 hours (3 days) must elapse between doses. Once you select a new day, maintain that schedule consistently going forward.
For short-acting agents like exenatide immediate-release (Byetta) and lixisenatide (Adlyxin), timing is specifically linked to meals—these must be administered within 60 minutes before eating.
Injection site rotation is an important technical consideration that should be incorporated into your routine. These medications are typically administered subcutaneously in the abdomen, thigh, or upper arm. Rotating injection sites reduces the risk of injection site reactions. Keep a simple log or use a smartphone reminder to track both timing and location of injections. Never share injection pens with others, even if you change the needle. If you also use insulin, administer these medications at different injection sites.
Some patients report that administering their GLP-1 injection in the evening, particularly after dinner, may help them manage early gastrointestinal side effects such as nausea, as they can sleep through the initial hours after injection. While there is no official clinical guidance supporting this practice, individual tolerance patterns vary, and patients should discuss timing strategies with their healthcare provider if side effects are problematic. The most important factor remains consistent adherence to the prescribed schedule, regardless of the specific time chosen.
The most frequently reported adverse effects of GLP-1 receptor agonists are gastrointestinal in nature, including nausea, vomiting, diarrhea, constipation, and abdominal discomfort. These effects result directly from the medication's mechanism of action—specifically, delayed gastric emptying and effects on gastrointestinal motility. According to FDA prescribing information, gastrointestinal side effects are typically most pronounced during dose initiation and escalation, and they often diminish over time as the body adapts to the medication.
While the timing of most injections relative to meals does not affect drug absorption, strategic meal planning can help manage gastrointestinal symptoms. Patients experiencing nausea may benefit from eating smaller, more frequent meals rather than large portions, as the medication already slows stomach emptying. Avoiding high-fat, greasy, or heavily spiced foods can reduce nausea severity. Staying well-hydrated and eating slowly, with adequate chewing, supports digestive comfort when gastric emptying is delayed.
Some practical dietary strategies include:
Smaller portion sizes: Eating until comfortably satisfied rather than full reduces the risk of nausea and discomfort
Bland, easily digestible foods: During dose escalation, focus on lean proteins, whole grains, and cooked vegetables
Adequate hydration: Sipping water throughout the day, particularly if experiencing nausea or constipation
Avoiding trigger foods: Identifying and temporarily limiting foods that worsen individual symptoms
Persistent vomiting or diarrhea can lead to dehydration and potentially acute kidney injury. Contact your healthcare provider if you're unable to keep fluids down or notice decreased urination.
Patients with diabetic retinopathy should be aware that rapid improvement in blood glucose with semaglutide may temporarily worsen retinopathy; report any vision changes to your provider.
These medications may also affect the absorption of oral medications. Notably, tirzepatide can reduce the effectiveness of oral contraceptives during initiation and dose increases; alternative contraception is recommended for 4 weeks after starting or increasing doses.
More serious but less common adverse effects include pancreatitis, gallbladder disease, and hypoglycemia (particularly when combined with insulin or sulfonylureas). The FDA labeling includes a boxed warning regarding thyroid C-cell tumors observed in rodent studies, though the relevance to humans remains uncertain. Patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 should not use these medications.
While GLP-1 receptor agonists are generally well-tolerated, certain symptoms warrant prompt medical evaluation. Contact your healthcare provider immediately if you experience severe, persistent abdominal pain, particularly if it radiates to the back, as this may indicate pancreatitis. This serious adverse effect requires urgent assessment and typically necessitates discontinuation of the medication. Similarly, symptoms of gallbladder disease—including right upper quadrant pain, fever, jaundice (yellowing of skin or eyes), or clay-colored stools—require prompt evaluation.
Signs of dehydration or potential kidney problems—such as persistent vomiting, inability to keep fluids down, decreased urination, or dark-colored urine—should prompt immediate medical attention. Patients with diabetic retinopathy should report any vision changes, as rapid improvement in blood glucose can temporarily worsen retinopathy, particularly with semaglutide.
Signs of an allergic reaction, though rare, constitute a medical emergency. Seek immediate care for difficulty breathing, severe rash, swelling of the face or throat, or rapid heartbeat after injection. Additionally, if you experience symptoms of thyroid tumors—such as a lump in the neck, persistent hoarseness, difficulty swallowing, or shortness of breath—contact your provider for evaluation, though it should be noted that the clinical significance of thyroid findings from animal studies remains uncertain in humans.
Hypoglycemia symptoms require attention, particularly if you are taking GLP-1 medications in combination with insulin or sulfonylureas. Warning signs include shakiness, sweating, confusion, rapid heartbeat, dizziness, or extreme hunger. While GLP-1 agents alone rarely cause hypoglycemia due to their glucose-dependent mechanism, combination therapy increases this risk. Your provider may need to adjust doses of other diabetes medications when initiating or escalating GLP-1 therapy.
Routine follow-up is essential for monitoring treatment response and safety. Schedule regular appointments to assess glycemic control (through A1C testing), weight changes, and tolerability. If you are planning surgery or procedures requiring anesthesia, inform your surgical team about your GLP-1 medication use, as they may provide specific instructions. If you are considering pregnancy or become pregnant while taking a GLP-1 medication, contact your provider promptly, as these agents are generally discontinued before conception due to limited safety data in pregnancy.
Yes, you can eat before or after taking semaglutide injections (Ozempic, Wegovy). Food does not affect the absorption or efficacy of subcutaneous GLP-1 injections, so you may administer them at any time regardless of meals.
Short-acting GLP-1 agents like exenatide immediate-release (Byetta) and lixisenatide (Adlyxin) must be administered within 60 minutes before meals. The oral formulation of semaglutide (Rybelsus) also requires empty stomach administration with specific water restrictions.
While injection timing relative to meals doesn't affect absorption, eating smaller, more frequent meals and avoiding high-fat or greasy foods can help manage nausea. Some patients find evening injections allow them to sleep through initial side effects.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.