LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide after gallbladder removal is safe and effective for managing type 2 diabetes and chronic weight management. This dual GIP/GLP-1 receptor agonist (Mounjaro, Zepbound) is not contraindicated in patients who have undergone cholecystectomy, as it does not depend on biliary function for its therapeutic action. While both tirzepatide and gallbladder removal can affect digestion, understanding how these factors interact helps optimize treatment outcomes. This guide examines the safety profile, dosing considerations, and practical management strategies for patients using tirzepatide after cholecystectomy, addressing common concerns about gastrointestinal side effects and medication efficacy in this population.
Quick Answer: Tirzepatide can be safely used after gallbladder removal, as cholecystectomy is not a contraindication and does not affect the medication's pharmacokinetics or therapeutic efficacy.
Tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management and chronic weight management in adults. For weight management, it's indicated for adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. This injectable medication works by enhancing insulin secretion, suppressing glucagon release, slowing gastric emptying, and reducing appetite through central nervous system pathways.
Cholecystectomy, the surgical removal of the gallbladder, is one of the most common abdominal procedures performed in the United States. The gallbladder stores and concentrates bile produced by the liver, releasing it in response to dietary fat to aid digestion. After cholecystectomy, bile flows continuously from the liver directly into the small intestine rather than being stored and released on demand.
Patients who have undergone cholecystectomy may require tirzepatide for diabetes management or weight loss, raising important questions about safety and efficacy in this population. The FDA prescribing information for tirzepatide does not specifically contraindicate its use after gallbladder removal, and cholecystectomy is not listed as a precaution. However, understanding the interaction between tirzepatide's mechanism of action and post-cholecystectomy digestive physiology is essential for optimizing patient outcomes.
Both tirzepatide therapy and gallbladder disease share associations with weight changes and gastrointestinal symptoms, making it important for clinicians to understand how these factors intersect in patient care. The absence of the gallbladder does not fundamentally alter tirzepatide's pharmacokinetics, as the medication is administered subcutaneously and undergoes proteolytic degradation rather than requiring biliary processing for absorption or metabolism.
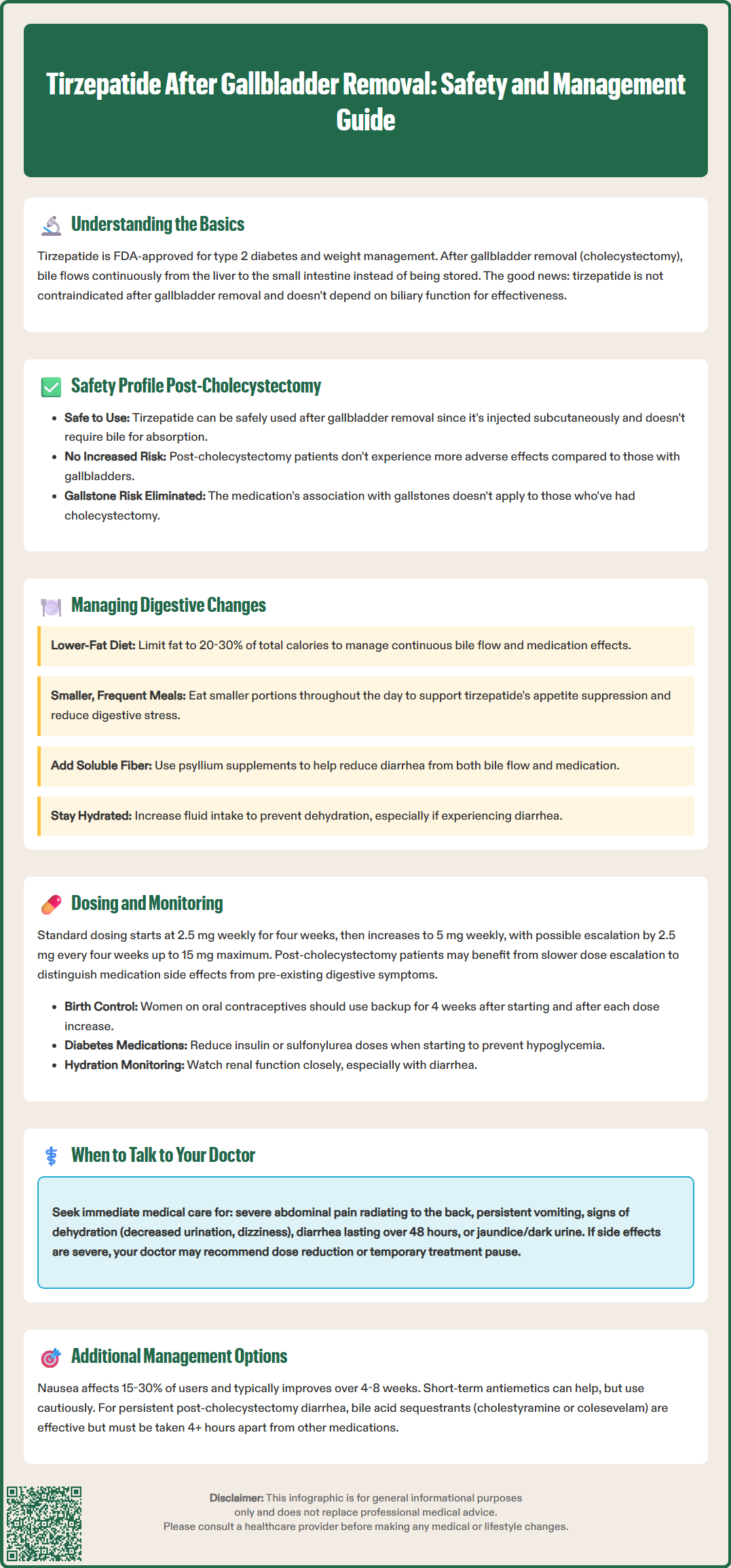
There is no specific contraindication to using tirzepatide in patients who have previously undergone cholecystectomy. The medication's safety profile appears consistent regardless of gallbladder status, as tirzepatide does not depend on biliary function for its therapeutic action or elimination. The drug is metabolized primarily through proteolytic cleavage and does not undergo hepatobiliary excretion as an intact molecule.
While clinical trials of tirzepatide included patients with various medical histories, specific subgroup analyses focused on post-cholecystectomy patients have not been published. The most common adverse effects of tirzepatide—nausea, diarrhea, vomiting, constipation, and abdominal pain—are gastrointestinal in nature and occur through the medication's effects on gastric motility and gut hormone signaling rather than biliary mechanisms.
Importantly, tirzepatide carries a boxed warning regarding thyroid C-cell tumors observed in rodent studies, though the relevance to humans remains uncertain. This warning applies equally to all patients regardless of gallbladder status. The medication is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2.
The FDA label for tirzepatide includes warnings about acute gallbladder disease, as GLP-1 receptor agonists have been associated with an increased risk of cholelithiasis or cholecystitis. This association is likely related to rapid weight loss and altered gallbladder motility. While the specific risk of gallstone formation is not applicable to patients who have already undergone cholecystectomy, other biliary tract complications remain theoretically possible. There is currently no evidence suggesting that post-cholecystectomy patients experience increased tirzepatide-related adverse effects compared to those with intact gallbladders.
Patients should be informed that having undergone cholecystectomy does not appear to increase their risk of tirzepatide-related adverse effects, though individual tolerance to gastrointestinal side effects may vary based on their post-surgical digestive adaptation.
After cholecystectomy, patients experience altered bile flow patterns that can affect fat digestion and bowel habits. Without a gallbladder to store and concentrate bile, bile acids flow continuously into the duodenum in a diluted form. This continuous bile flow can lead to bile acid diarrhea (also called bile acid malabsorption) in some post-cholecystectomy patients, with reported prevalence estimates varying widely in the literature. This condition is particularly noticeable after consuming high-fat meals.
Tirzepatide's mechanism of slowing gastric emptying and affecting gastrointestinal motility may theoretically interact with these post-cholecystectomy changes. The delayed gastric emptying induced by tirzepatide could potentially provide more gradual delivery of nutrients to the small intestine, though there are no clinical studies specifically examining whether this effect modifies bile acid-related diarrhea. Conversely, the medication's effects on intestinal motility might exacerbate loose stools in susceptible individuals.
Post-cholecystectomy syndrome, characterized by persistent abdominal pain, bloating, and altered bowel habits after gallbladder removal, affects a variable percentage of patients depending on diagnostic criteria used. Distinguishing between symptoms related to post-cholecystectomy digestive changes and those attributable to tirzepatide can be challenging, particularly during the initial titration period when gastrointestinal side effects are most common.
Patients without a gallbladder may benefit from dietary modifications that complement tirzepatide therapy. A lower-fat diet distributed across smaller, more frequent meals can minimize bile acid-related symptoms while supporting the appetite suppression and portion control that tirzepatide promotes. Adequate hydration becomes particularly important, as both post-cholecystectomy diarrhea and tirzepatide-related gastrointestinal effects can increase fluid losses.
Clinicians should obtain a thorough history of post-cholecystectomy digestive patterns before initiating tirzepatide, establishing a baseline against which medication-related changes can be assessed. Patients who have achieved stable digestive function after cholecystectomy are generally good candidates for tirzepatide therapy, while those with ongoing post-cholecystectomy syndrome may require additional evaluation and management strategies.
The standard tirzepatide dosing protocol does not require modification based on cholecystectomy status. For type 2 diabetes, the initial dose is 2.5 mg subcutaneously once weekly for four weeks, followed by escalation to 5 mg weekly. The dose may be increased in 2.5 mg increments every four weeks based on glycemic response and tolerability, up to a maximum of 15 mg weekly. For chronic weight management, the same titration schedule applies, with maintenance doses typically ranging from 5 mg to 15 mg weekly.
The gradual dose escalation strategy is particularly important in post-cholecystectomy patients to allow assessment of gastrointestinal tolerance at each dose level. Because these patients may already experience digestive symptoms related to altered bile flow, distinguishing medication-related side effects from pre-existing issues requires careful monitoring during titration. Maintaining patients at a given dose for an additional four weeks before escalation may be appropriate if gastrointestinal symptoms are difficult to characterize.
Patients should be advised that tirzepatide may delay gastric emptying, potentially affecting the absorption of oral medications. Women using oral contraceptives should use a non-oral method or add a backup method for 4 weeks after tirzepatide initiation and for 4 weeks after each dose escalation. Tirzepatide should be used with caution in patients with severe gastrointestinal disease, including severe gastroparesis.
When tirzepatide is used with insulin or insulin secretagogues (such as sulfonylureas), the risk of hypoglycemia increases. Clinicians should consider reducing the dose of these medications when initiating tirzepatide therapy to mitigate this risk.
Monitoring parameters should include standard assessments: hemoglobin A1c and fasting glucose for diabetes management, body weight, blood pressure, and lipid profiles. Additionally, clinicians should specifically inquire about stool frequency, consistency, and timing relative to meals to identify patterns suggesting bile acid malabsorption versus medication-related effects.
Patients should be educated to report severe or persistent abdominal pain, as tirzepatide has been associated with acute pancreatitis in clinical trials. The FDA label advises considering alternative therapies in patients with a history of pancreatitis. While there is no evidence that cholecystectomy specifically increases pancreatitis risk from tirzepatide, patients with a history of pancreatitis warrant particularly careful monitoring. Lipase elevation alone without clinical symptoms does not necessarily indicate pancreatitis and should be interpreted in clinical context.
Renal function monitoring is important because gastrointestinal side effects leading to dehydration could precipitate acute kidney injury, particularly in patients with pre-existing renal impairment. Post-cholecystectomy patients experiencing diarrhea may be at risk for volume depletion and should be counseled on maintaining adequate fluid intake.
Managing tirzepatide's gastrointestinal side effects in post-cholecystectomy patients requires a tailored approach that addresses both medication-related symptoms and underlying digestive changes from gallbladder removal. Nausea, the most common side effect occurring in 15-30% of patients depending on dose, typically peaks during the first few weeks after dose initiation or escalation and often improves with continued use.
Dietary strategies form the foundation of side effect management. Patients should be advised to consume smaller, more frequent meals rather than large portions, which aligns with both tirzepatide's appetite-suppressing effects and the digestive limitations of continuous bile flow. Limiting dietary fat to 20-30% of total calories can reduce bile acid-related diarrhea while supporting weight loss goals. Soluble fiber supplementation (such as psyllium) may help by binding bile acids and improving stool consistency.
If side effects are intolerable despite dietary modifications, dose reduction or temporary treatment interruption may be necessary, with subsequent slower re-titration once symptoms resolve. For persistent nausea that significantly impacts quality of life, antiemetic medications may be considered. If metoclopramide is used, clinicians should be aware of its FDA boxed warning regarding tardive dyskinesia with long-term use and limit duration of therapy. Ginger supplements or acupressure wristbands offer non-pharmacologic alternatives that some patients find helpful.
Bile acid sequestrants such as cholestyramine or colesevelam can be effective for post-cholecystectomy diarrhea under clinician guidance. These agents should be taken at least four hours before or after other medications to avoid binding interactions. Patients should be informed that bile acid sequestrants may cause constipation and can affect the absorption of fat-soluble vitamins and certain medications.
When to seek medical attention:
Severe, persistent abdominal pain radiating to the back (possible pancreatitis)
Persistent vomiting preventing adequate hydration
Signs of dehydration: decreased urination, dizziness, extreme thirst
Severe diarrhea lasting more than 48 hours
Jaundice or dark urine (suggesting biliary obstruction, which remains possible despite cholecystectomy)
Patients should be reassured that most gastrointestinal side effects improve significantly within 4-8 weeks of reaching a stable dose. Tirzepatide should be discontinued if pregnancy is detected, as weight loss medications are not recommended during pregnancy.
Yes, tirzepatide can be safely used after cholecystectomy. The FDA prescribing information does not contraindicate tirzepatide in patients who have undergone gallbladder removal, and the medication's effectiveness is not affected by gallbladder status.
No, tirzepatide dosing does not require modification based on cholecystectomy status. The standard protocol starts at 2.5 mg weekly with gradual escalation every four weeks based on response and tolerability, regardless of gallbladder status.
There is no evidence that post-cholecystectomy patients experience increased tirzepatide-related side effects compared to those with intact gallbladders. However, distinguishing between medication-related gastrointestinal symptoms and pre-existing post-surgical digestive changes requires careful monitoring during treatment initiation.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.