LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 receptor agonist approved by the FDA for type 2 diabetes and chronic weight management. While this once-weekly injectable medication effectively improves glycemic control and promotes weight loss, questions have emerged about its potential impact on vitamin B12 levels. Unlike metformin, which has a well-established association with B12 deficiency, tirzepatide has not demonstrated a direct mechanism affecting B12 absorption. However, indirect factors—including altered gastric emptying, reduced dietary intake, and concurrent metformin use—may influence B12 status in patients taking this medication. Understanding these relationships is essential for optimal patient monitoring and care.
Quick Answer: Tirzepatide has no established direct effect on vitamin B12 levels, but indirect factors such as reduced dietary intake, slowed gastric emptying, and concurrent metformin use may increase deficiency risk.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Marketed under the brand names Mounjaro (for diabetes) and Zepbound (for weight management), tirzepatide works by mimicking the actions of two naturally occurring incretin hormones.
GIP and GLP-1 are released from the intestine in response to food intake and play crucial roles in glucose homeostasis. By activating both GIP and GLP-1 receptors, tirzepatide enhances glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriately elevated glucagon secretion, and slows gastric emptying. These combined effects result in improved glycemic control and weight reduction.
Tirzepatide is administered as a once-weekly subcutaneous injection, starting at 2.5 mg for the first 4 weeks as an initiation dose only. The dose is then increased in 2.5 mg increments every 4 weeks as tolerated, with typical maintenance doses ranging from 5 mg to 15 mg. In clinical trials such as SURPASS-2, tirzepatide demonstrated greater efficacy in type 2 diabetes compared to semaglutide 1 mg, with patients achieving substantial reductions in hemoglobin A1c levels and body weight.
Common adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhea, and decreased appetite, which are generally mild to moderate in severity and tend to diminish over time. Important safety information includes a boxed warning for thyroid C-cell tumors (contraindicated in patients with personal/family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2) and warnings for pancreatitis, gallbladder disease, acute kidney injury, and hypoglycemia risk when used with insulin or sulfonylureas.
Currently, there is no established direct link between tirzepatide use and vitamin B12 deficiency based on available clinical trial data and FDA labeling information. Unlike metformin, which has a well-documented association with reduced vitamin B12 absorption, tirzepatide has not demonstrated a similar pharmacological mechanism that would directly interfere with B12 metabolism or absorption in the terminal ileum.
However, several theoretical indirect mechanisms warrant clinical consideration. Tirzepatide's effect on gastric emptying and gastrointestinal motility could theoretically influence the absorption of various nutrients, including vitamin B12. The medication significantly slows gastric emptying, which is central to its therapeutic mechanism but may potentially alter the normal digestive processes required for B12 liberation from food proteins and subsequent binding to intrinsic factor. Additionally, the gastrointestinal adverse effects commonly experienced with tirzepatide—including nausea, vomiting, and reduced appetite—may lead to decreased dietary intake and potential nutritional deficiencies over time.
Patients taking tirzepatide often experience substantial weight loss, which typically involves significant dietary modifications and reduced caloric intake. This behavioral change, rather than a direct drug effect, may contribute to inadequate consumption of B12-rich foods such as meat, fish, dairy products, and fortified cereals. Furthermore, many patients prescribed tirzepatide for type 2 diabetes are concurrently taking metformin, which independently increases the risk of vitamin B12 deficiency through impaired calcium-dependent B12-intrinsic factor uptake in the ileum. This combination therapy scenario makes it challenging to attribute B12 deficiency solely to tirzepatide when multiple risk factors coexist.
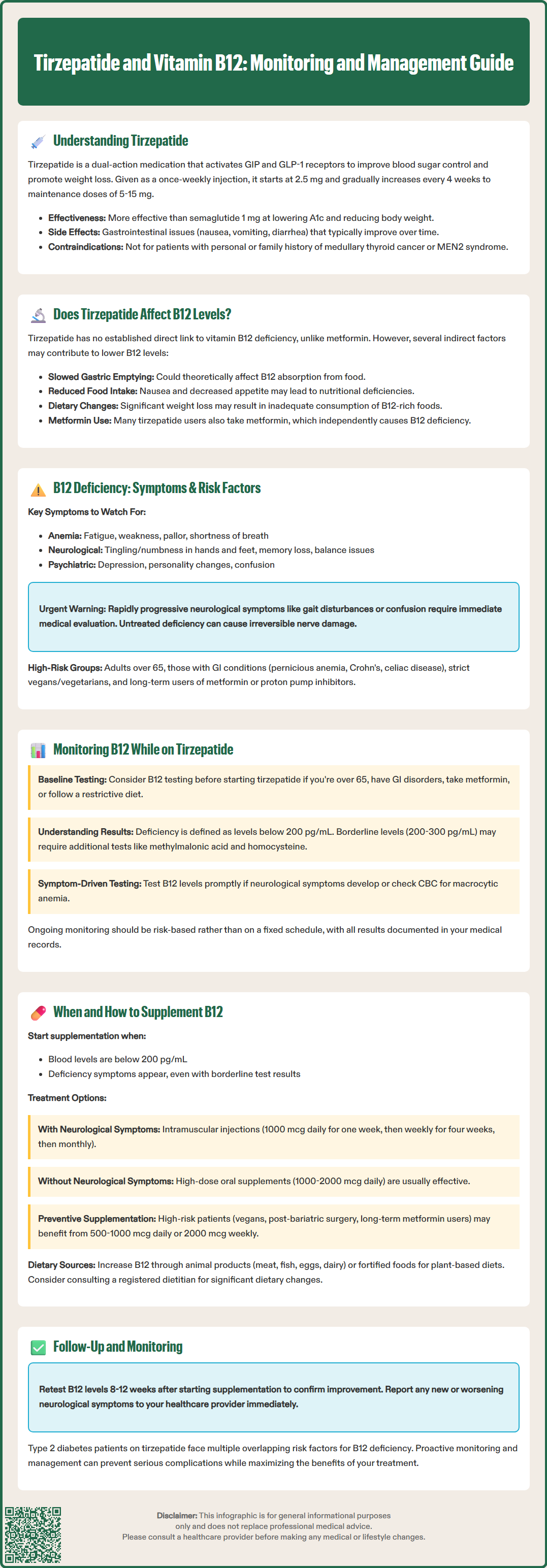
Vitamin B12 (cobalamin) is an essential water-soluble vitamin critical for DNA synthesis, red blood cell formation, and neurological function. Deficiency develops gradually, as the body stores approximately 2-5 mg of B12 in the liver, which can sustain normal function for several years even with inadequate intake or absorption. Clinical manifestations of B12 deficiency are diverse and can affect multiple organ systems.
Hematological symptoms include macrocytic anemia, characterized by fatigue, weakness, pallor, and shortness of breath. Folate deficiency can present with similar macrocytosis and should be assessed concurrently. Neurological manifestations are particularly concerning and may include peripheral neuropathy with paresthesias (tingling and numbness in hands and feet), ataxia, impaired proprioception and vibratory sense, cognitive impairment, memory loss, and in severe cases, subacute combined degeneration of the spinal cord. Rapidly progressive neurologic deficits, gait disturbance, or confusion warrant urgent evaluation. Neuropsychiatric symptoms such as depression, irritability, and personality changes may also occur. Glossitis (inflamed, smooth tongue) and angular cheilitis are characteristic mucocutaneous findings.
Several risk factors predispose individuals to vitamin B12 deficiency beyond medication effects. Age-related factors include reduced gastric acid production (achlorhydria) in older adults, which impairs B12 liberation from food. Gastrointestinal conditions such as pernicious anemia (autoimmune destruction of gastric parietal cells), Crohn's disease, celiac disease, and prior gastric or ileal surgery significantly impair absorption. Dietary factors include strict vegan or vegetarian diets lacking animal products. Medication use, particularly long-term metformin therapy, proton pump inhibitors, and H2-receptor antagonists, increases deficiency risk. Patients with type 2 diabetes taking tirzepatide often have multiple overlapping risk factors, including advanced age, metformin use, and potential dietary restrictions, making them a particularly vulnerable population requiring vigilant monitoring.
While routine vitamin B12 monitoring is not specifically mandated in tirzepatide prescribing information, clinical judgment should guide individualized screening strategies based on patient risk factors and clinical presentation. The American Diabetes Association (ADA) recommends considering periodic measurement of vitamin B12 levels in patients with type 2 diabetes taking metformin, particularly those with anemia or peripheral neuropathy, though no specific monitoring interval is specified.
Baseline assessment should be considered before initiating tirzepatide in high-risk patients, including those over 65 years of age, individuals with pre-existing gastrointestinal disorders, patients on concurrent metformin or acid-suppressing medications, and those following restrictive diets. Laboratory evaluation typically includes serum vitamin B12 levels, with values below 200 pg/mL generally indicating deficiency and levels between 200-300 pg/mL considered borderline, though laboratory reference ranges may vary. When B12 levels are equivocal, additional testing with methylmalonic acid (MMA) and homocysteine levels can provide greater diagnostic accuracy, as both are elevated in true B12 deficiency.
Ongoing monitoring should be based on individual risk assessment rather than a fixed schedule. Testing is appropriate when symptoms suggestive of deficiency develop or when risk factors accumulate. Complete blood count (CBC) should be reviewed for macrocytic anemia, characterized by elevated mean corpuscular volume (MCV). Patients experiencing neurological symptoms such as paresthesias, balance problems, or cognitive changes warrant prompt B12 assessment with same-day clinical evaluation for severe or rapidly progressive symptoms. Healthcare providers should maintain a low threshold for testing given the potential for irreversible neurological damage if deficiency remains undetected and untreated. Documentation of B12 status and monitoring plans in the medical record facilitates continuity of care and appropriate follow-up.
Vitamin B12 supplementation should be initiated when laboratory testing confirms deficiency (serum B12 <200 pg/mL) or when clinical symptoms strongly suggest deficiency even with borderline laboratory values. The route and dosage of supplementation depend on the severity of deficiency, presence of neurological symptoms, and underlying cause of the deficiency.
For confirmed deficiency with neurological symptoms, intramuscular cyanocobalamin injections are preferred, typically administered as 1000 mcg daily for one week, then weekly for four weeks, followed by monthly maintenance therapy. This parenteral approach bypasses potential absorption issues and rapidly replenishes body stores. For deficiency without neurological involvement or for borderline levels, oral supplementation with high-dose cyanocobalamin (1000-2000 mcg daily) is often effective, as approximately 1% of an oral dose is absorbed through passive diffusion even in the absence of intrinsic factor. Sublingual and nasal formulations are alternative options, though evidence supporting superior efficacy over oral tablets is limited.
Prophylactic supplementation may be considered for select high-risk patients, particularly those with strict vegan diets, post-bariatric surgery, or on long-term metformin therapy. A daily oral supplement of 500-1000 mcg or a weekly dose of 2000 mcg can help maintain adequate levels, though evidence for routine prophylaxis specifically for tirzepatide users is limited. Many multivitamin preparations contain B12, though doses are typically lower (6-25 mcg) and may be insufficient for patients with absorption issues.
Patients should be counseled on dietary sources of vitamin B12, including animal products such as meat, poultry, fish, eggs, and dairy. For those following plant-based diets, fortified cereals, nutritional yeast, and plant-based milk alternatives can provide supplemental B12. Referral to a registered dietitian is valuable for patients experiencing significant dietary changes or restrictions during tirzepatide therapy. Follow-up laboratory testing should occur 8-12 weeks after initiating supplementation to confirm adequate response, with ongoing monitoring as clinically indicated. Patients should be advised to report new or worsening neurological symptoms promptly, as these may indicate progressive deficiency requiring more aggressive intervention.
Tirzepatide has no established direct mechanism causing vitamin B12 deficiency, unlike metformin. However, indirect factors such as reduced dietary intake from decreased appetite, altered gastric emptying, and concurrent use of metformin may increase the risk of B12 deficiency in some patients.
Routine B12 monitoring is not mandated for tirzepatide, but baseline and periodic testing should be considered for high-risk patients, including those over 65, on concurrent metformin, with gastrointestinal disorders, or experiencing symptoms such as fatigue, neuropathy, or cognitive changes.
Symptoms include fatigue, weakness, tingling or numbness in hands and feet, balance problems, memory loss, cognitive impairment, smooth or inflamed tongue, and macrocytic anemia. Neurological symptoms warrant prompt medical evaluation as they may become irreversible if untreated.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.