LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide effects on brain function represent an emerging area of scientific interest beyond this medication's established metabolic benefits. As a dual GIP and GLP-1 receptor agonist approved for type 2 diabetes and weight management, tirzepatide acts on receptors throughout the central nervous system, influencing appetite regulation and potentially offering neuroprotective properties. While preclinical research suggests promising effects on brain health, including reduced neuroinflammation and enhanced neuronal survival, human evidence remains limited. Understanding how tirzepatide interacts with brain pathways is essential for clinicians managing patients on this therapy and for recognizing both therapeutic potential and safety considerations in neurological health.
Quick Answer: Tirzepatide acts on GIP and GLP-1 receptors in the brain to regulate appetite and may offer neuroprotective effects, though human evidence for cognitive benefits remains limited and investigational.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus (brand name Mounjaro) and chronic weight management (brand name Zepbound). This medication combines the actions of two incretin hormones that play crucial roles in glucose homeostasis and energy regulation.
The medication works primarily through its effects on GIP and GLP-1 receptors located throughout the body, including the pancreas, gastrointestinal tract, and the central nervous system. When tirzepatide binds to GLP-1 receptors on pancreatic beta cells, it stimulates glucose-dependent insulin secretion, meaning insulin is released only when blood glucose levels are elevated. Simultaneously, it suppresses glucagon secretion from pancreatic alpha cells, reducing hepatic glucose production. The GIP component enhances insulin secretion and may improve insulin sensitivity in peripheral tissues.
Beyond glycemic control, tirzepatide affects appetite regulation through central nervous system pathways. GLP-1 receptors are expressed in key brain regions including the hypothalamus, brainstem, and reward centers. Activation of these receptors may reduce appetite, increase satiety, and slow gastric emptying, though the gastric emptying effects tend to diminish with chronic use. The medication may also influence food reward pathways, potentially affecting food preferences. These effects contribute to the medication's weight loss efficacy, with clinical trials showing weight reductions that vary by dose and indication, generally ranging from 5-15% in type 2 diabetes and 15-20% in obesity at the highest doses.
Tirzepatide is administered as a once-weekly subcutaneous injection. Treatment typically begins with a 2.5 mg dose for 4 weeks to improve gastrointestinal tolerability, followed by gradual dose increases every 4 weeks as tolerated, up to a maximum of 15 mg weekly. Tirzepatide is not indicated for type 1 diabetes and should not be used in combination with other GLP-1 receptor agonists or weight management medications.
Preclinical research suggests that GLP-1 receptor agonists may possess neuroprotective properties that extend beyond metabolic regulation. Animal studies have demonstrated that GLP-1 receptor activation can reduce neuroinflammation, decrease oxidative stress, and promote neuronal survival in models of neurodegenerative disease. These findings have generated interest in the potential therapeutic applications of incretin-based therapies for conditions such as Alzheimer's disease, Parkinson's disease, and stroke recovery.
In experimental models of Alzheimer's disease, GLP-1 receptor agonists have shown promise in reducing amyloid-beta plaque formation and tau protein phosphorylation, two hallmark pathological features of the condition. Additionally, these medications appear to enhance synaptic plasticity and may improve cerebral blood flow in preclinical models, mechanisms that could theoretically support cognitive function. Some animal studies have reported improvements in spatial learning and memory tasks following GLP-1 receptor agonist treatment, though it remains uncertain whether these effects translate to human populations.
The proposed neuroprotective mechanisms include enhancement of brain-derived neurotrophic factor (BDNF) expression, reduction of microglial activation, and improvement of mitochondrial function in neurons. GLP-1 receptors are expressed throughout the brain, particularly in regions vulnerable to neurodegenerative processes such as the hippocampus and cortex. However, it is important to note that most neuroprotective data comes from animal models and in vitro studies, with limited evidence specific to tirzepatide.
Several clinical trials are investigating whether GLP-1 receptor agonists can slow cognitive decline in patients with mild cognitive impairment or early Alzheimer's disease, including studies with semaglutide (EVOKE and EVOKE+ trials). Human evidence for cognitive benefits with GLP-1 receptor agonists remains mixed and inconclusive, and definitive evidence for tirzepatide specifically is not yet available. Clinicians should recognize that while the preclinical data is encouraging, prescribing tirzepatide for neuroprotection is investigational and not supported by FDA-approved indications.
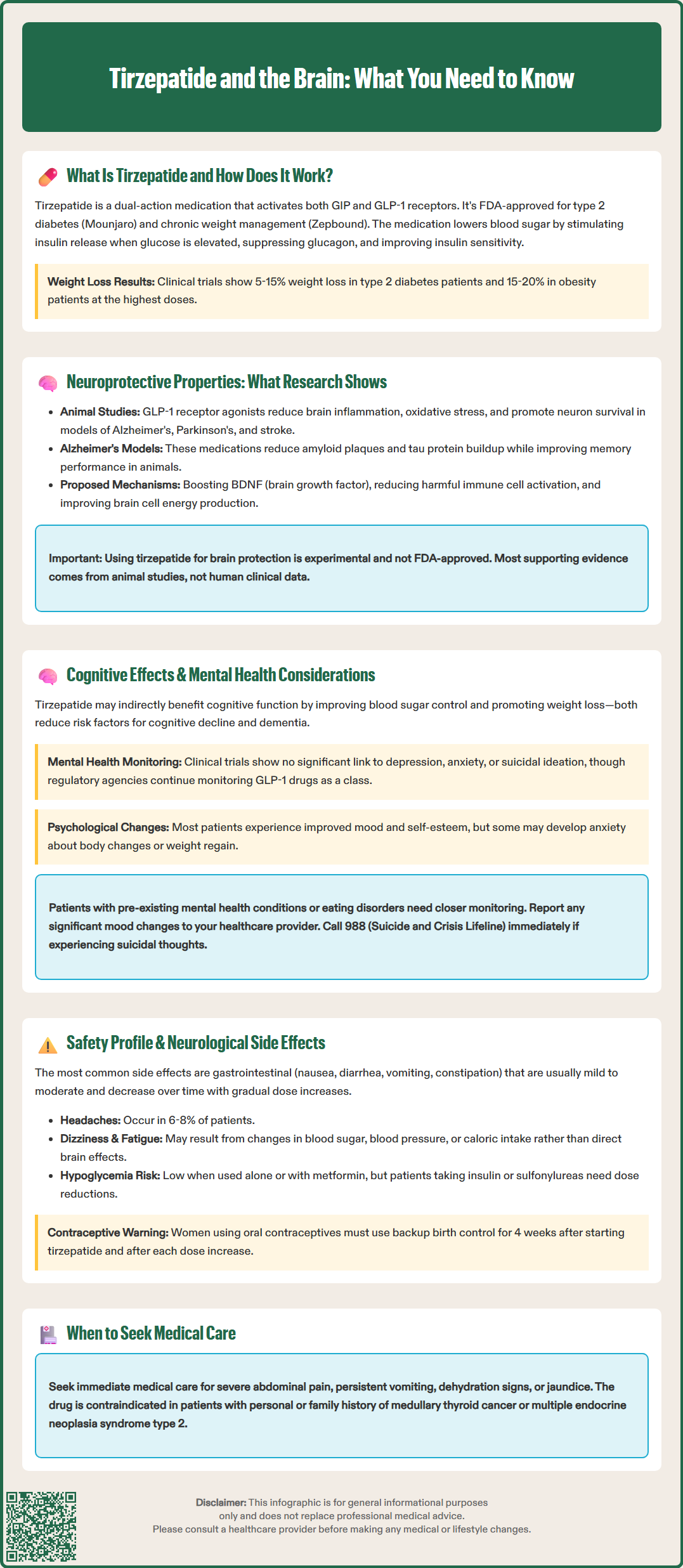
The relationship between tirzepatide and cognitive function is complex and multifaceted. Improved glycemic control and weight loss achieved through tirzepatide therapy may indirectly benefit cognitive health, as both poorly controlled diabetes and obesity are established risk factors for cognitive decline and dementia. Patients with type 2 diabetes who achieve better glucose control often report improvements in concentration, mental clarity, and overall cognitive performance, though these effects typically reflect resolution of hyperglycemia-related symptoms rather than direct drug effects on the brain.
Regarding mental health, clinical trial data for tirzepatide have not identified significant concerns related to depression or anxiety as direct adverse effects. However, substantial weight loss from any cause can be associated with psychological changes, both positive and negative. Many patients experience improved mood, self-esteem, and quality of life as they lose weight and achieve better metabolic control. Conversely, some individuals may experience anxiety related to rapid body composition changes or concerns about weight regain if treatment is discontinued.
There is no established link between tirzepatide and increased risk of suicidal ideation or behavior, though this has been an area of scrutiny for GLP-1 receptor agonists as a class. The FDA and European Medicines Agency have reviewed available data and have not identified a causal relationship. Nevertheless, clinicians should maintain awareness of patients' mental health status, particularly in those with pre-existing psychiatric conditions or history of eating disorders.
Patients initiating tirzepatide should be counseled about the importance of reporting any significant mood changes, cognitive difficulties, or psychological distress. Those with a history of depression, anxiety disorders, or eating disorders may benefit from closer monitoring and potentially concurrent mental health support. If patients experience suicidal thoughts, they should be advised to call or text 988 (Suicide and Crisis Lifeline) and seek emergency care for imminent risk. Healthcare providers should consider a multidisciplinary approach that includes nutritional counseling, behavioral support, and mental health resources when appropriate.
Tirzepatide's safety profile is generally favorable, with most adverse effects related to gastrointestinal function rather than neurological systems. The most common side effects include nausea, diarrhea, vomiting, constipation, and abdominal discomfort, which are typically mild to moderate in severity and tend to diminish over time. These effects result from the medication's actions on GLP-1 receptors in the gastrointestinal tract and can be minimized through gradual dose escalation.
Neurological side effects specifically attributed to tirzepatide are uncommon but warrant clinical attention. Headache has been reported in approximately 6-8% of patients in clinical trials, though causality is often difficult to establish given the high background prevalence of headaches in the general population. Dizziness and fatigue have also been reported, which may relate to changes in blood glucose levels, blood pressure, or caloric intake rather than direct central nervous system effects.
Hypoglycemia is a potential concern when tirzepatide is used in combination with insulin or sulfonylureas, and severe hypoglycemia can cause neurological symptoms including confusion, seizures, and loss of consciousness. However, tirzepatide's glucose-dependent mechanism of action means that hypoglycemia risk is low when used as monotherapy or with metformin. Patients using concomitant insulin or sulfonylureas typically require dose reductions of these medications to minimize hypoglycemia risk.
Important FDA-labeled warnings and precautions include risk of acute pancreatitis, acute gallbladder disease, acute kidney injury, hypersensitivity reactions including anaphylaxis, and severe gastrointestinal disease. Patients should seek immediate medical attention for severe abdominal pain (especially if radiating to the back), persistent vomiting, signs of dehydration, or jaundice. Tirzepatide carries a boxed warning regarding thyroid C-cell tumors observed in rodent studies, and is contraindicated in patients with personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2.
Patients should be aware that tirzepatide may affect the absorption of oral medications, including oral contraceptives. Women using oral contraceptives should use a backup method of contraception for 4 weeks after initiating tirzepatide and after each dose increase. Tirzepatide is not recommended during pregnancy, and women of reproductive potential should discuss pregnancy planning with their healthcare provider. The medication has not been established as safe and effective in pediatric populations for these indications.
Yes, tirzepatide activates GLP-1 receptors in the brain's hypothalamus, brainstem, and reward centers, which reduces appetite and increases satiety. Preclinical research suggests potential neuroprotective effects, but human evidence for cognitive benefits remains limited and investigational.
While animal studies show promise for neuroprotection and improved memory, definitive human evidence for tirzepatide's cognitive benefits is not yet available. Improved glycemic control and weight loss may indirectly support brain health, but prescribing tirzepatide specifically for neuroprotection is not FDA-approved.
Headache occurs in 6-8% of patients, while dizziness and fatigue are less common. Hypoglycemia-related neurological symptoms like confusion can occur when tirzepatide is combined with insulin or sulfonylureas, requiring dose adjustments of these medications.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.