LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide, a dual GIP/GLP-1 receptor agonist approved for type 2 diabetes and weight management, has sparked interest as a potential treatment for binge eating disorder (BED). While this medication demonstrates powerful effects on appetite regulation and weight reduction, its use for BED remains entirely off-label and unsupported by clinical trial evidence. This article examines the current state of knowledge regarding tirzepatide for binge eating disorder, including its mechanism of action, theoretical benefits, significant risks, and the critical importance of evidence-based psychological treatments. Understanding these factors is essential for patients and clinicians considering this experimental approach.
Quick Answer: Tirzepatide is not FDA-approved for binge eating disorder and lacks clinical trial evidence supporting its use for this condition.
Binge eating disorder (BED) is the most common eating disorder in the United States, affecting approximately 1.2% of the adult population. It is characterized by recurrent episodes of consuming large quantities of food in a discrete period, accompanied by a sense of loss of control, marked distress, and absence of regular compensatory behaviors such as purging. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) defines BED as occurring at least once weekly for three months, with associated features including eating more rapidly than normal, eating until uncomfortably full, eating when not physically hungry, and feelings of disgust or guilt afterward. Severity ranges from mild (1-3 episodes weekly) to extreme (14+ episodes weekly).
Current evidence-based treatments for BED include both psychological and pharmacological interventions. Cognitive behavioral therapy (CBT) remains the first-line psychological treatment, demonstrating significant efficacy in reducing binge episodes and improving psychological outcomes. Other therapeutic approaches include interpersonal psychotherapy and dialectical behavior therapy. From a pharmacological perspective, lisdexamfetamine dimesylate (Vyvanse) is currently the only FDA-approved medication specifically for moderate to severe BED in adults. This central nervous system stimulant has demonstrated effectiveness in reducing binge days and obsessive-compulsive features related to eating.
Additional medications used off-label for BED include selective serotonin reuptake inhibitors (SSRIs) and topiramate, though evidence for these agents varies. Many individuals with BED also present with comorbid obesity, type 2 diabetes, depression, or anxiety disorders, complicating treatment approaches. The relationship between BED and metabolic health has prompted interest in medications that address both disordered eating patterns and weight management, leading clinicians to explore novel therapeutic options including newer anti-obesity medications.
Clinicians should monitor for red flags requiring higher levels of care, including suicidal ideation, severe depression, medical instability, significant electrolyte disturbances, or severe dehydration. These symptoms may necessitate more intensive treatment settings such as partial hospitalization or inpatient care.
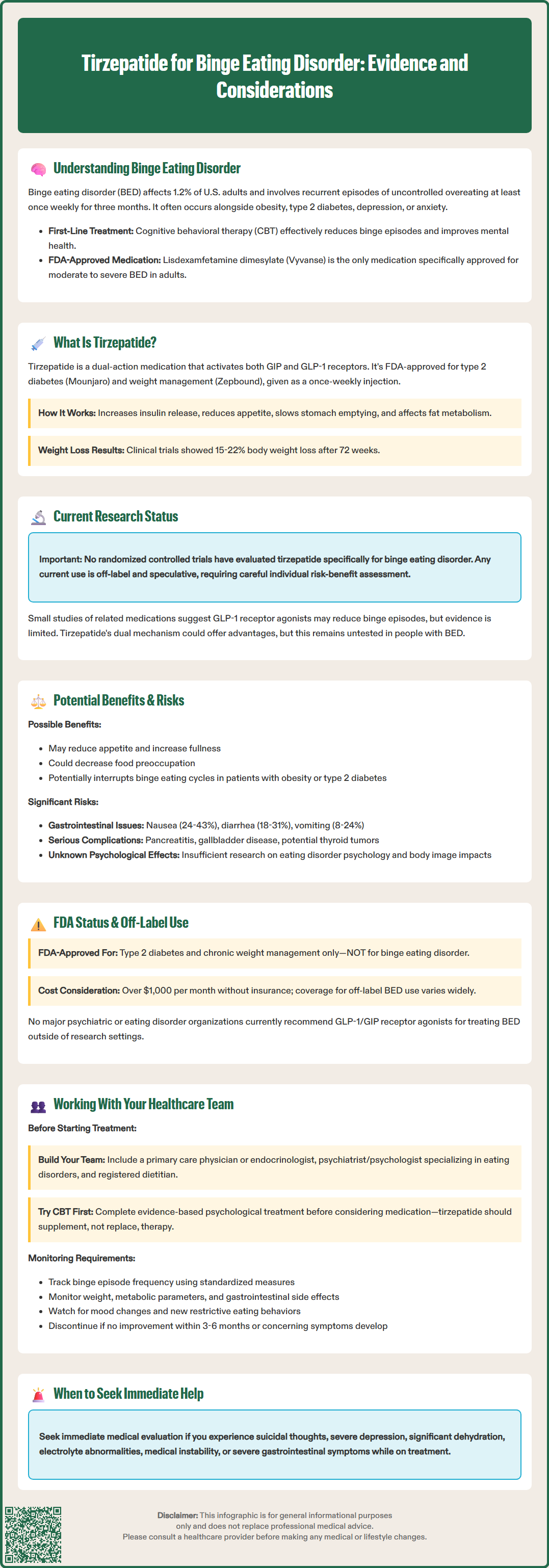
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist, representing the first dual incretin receptor agonist approved for clinical use. Marketed under the brand names Mounjaro for type 2 diabetes and Zepbound for chronic weight management, tirzepatide was approved by the FDA in May 2022 and November 2023, respectively. The medication is administered as a once-weekly subcutaneous injection, with doses ranging from 2.5 mg to 15 mg depending on the indication and individual tolerance.
The pharmacological mechanism of tirzepatide involves simultaneous activation of both GIP and GLP-1 receptors, which are naturally occurring incretin hormones involved in glucose homeostasis and appetite regulation. GLP-1 receptor activation enhances glucose-dependent insulin secretion, suppresses inappropriately elevated glucagon secretion, and slows gastric emptying. Additionally, GLP-1 acts on appetite centers in the hypothalamus to reduce food intake and increase satiety. The GIP component further augments insulin secretion and may have effects on fat metabolism and energy expenditure. This dual mechanism appears to produce greater effects on glycemic control and weight reduction compared to GLP-1 receptor agonists alone.
In clinical trials for type 2 diabetes (SURPASS program) and obesity (SURMOUNT-1), tirzepatide has demonstrated substantial efficacy. In the SURMOUNT-1 trial, participants with obesity or overweight achieved average weight reductions of 15-22% of body weight after 72 weeks, depending on the dose. The medication's effects on appetite and satiety have generated interest in its potential application for conditions characterized by dysregulated eating behaviors, including binge eating disorder.
Important safety information includes a boxed warning regarding thyroid C-cell tumors observed in rodent studies (contraindicated in patients with personal/family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2), risk of pancreatitis, gallbladder disease, and hypoglycemia when used with insulin or insulin secretagogues. Tirzepatide may decrease the effectiveness of oral contraceptives and is not recommended during pregnancy due to weight loss effects.
Currently, there are no published randomized controlled trials specifically evaluating tirzepatide for the treatment of binge eating disorder. The existing evidence base consists primarily of mechanistic insights from obesity and diabetes trials, case reports, and extrapolation from studies of other GLP-1 receptor agonists in eating disorders. This represents an important knowledge gap, as BED has distinct psychopathological features that may respond differently to pharmacological interventions compared to obesity without disordered eating patterns.
Research on related GLP-1 receptor agonists, such as semaglutide and liraglutide, provides some preliminary insights. Small studies and case series have suggested that GLP-1 receptor agonists may reduce binge eating episodes in some individuals, potentially through effects on satiety signaling and reduction of food cravings. However, these studies typically involve small, uncontrolled samples with significant methodological limitations, making it premature to draw firm conclusions about efficacy for BED.
The dual agonist properties of tirzepatide theoretically could provide additional benefits beyond GLP-1 monotherapy, but this hypothesis remains untested in the BED population. The effects of these medications on food-related reward pathways and impulse control in BED are largely theoretical and require further investigation through well-designed clinical trials.
Several clinical trials examining incretin-based therapies in eating disorder populations may be in development, though specific registered trials for tirzepatide in BED are limited. These studies face methodological challenges, including the need to distinguish between reduction in binge episodes due to pharmacological effects on eating behavior versus secondary effects of nausea or gastrointestinal side effects. Until rigorous clinical trial data become available, any use of tirzepatide for BED remains speculative and off-label, requiring careful consideration of the risk-benefit profile in individual patients.
The theoretical benefits of tirzepatide for individuals with binge eating disorder center on its effects on appetite regulation and satiety. For patients with BED who also have obesity or type 2 diabetes, tirzepatide could theoretically address multiple therapeutic targets simultaneously. The medication's ability to reduce overall food intake and increase feelings of fullness might help interrupt the cycle of binge eating episodes. Additionally, some patients report reduced food preoccupation while taking GLP-1-based medications, which could potentially benefit the obsessive thoughts about food characteristic of BED.
However, significant risks and concerns must be carefully considered. The most common adverse effects of tirzepatide at weight management doses include gastrointestinal symptoms such as nausea (24-43% of patients), diarrhea (18-31%), vomiting (8-24%), constipation (16-24%), and abdominal pain (10-20%), according to the FDA label. These side effects are typically most pronounced during dose escalation and may diminish over time, but they can be distressing and potentially trigger or worsen disordered eating patterns in vulnerable individuals. There is theoretical concern that the nausea and reduced appetite could reinforce restrictive eating behaviors or lead to a different pattern of disordered eating.
More serious potential risks include pancreatitis, gallbladder disease, and hypoglycemia when used with other glucose-lowering medications. The FDA label includes a boxed warning regarding thyroid C-cell tumors observed in rodent studies, with contraindication in patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2. Tirzepatide may decrease the effectiveness of oral contraceptives, requiring additional contraceptive measures. The medication is not recommended during pregnancy due to weight loss effects.
Critically, there is insufficient data on the psychological impact of these medications in individuals with eating disorders, including effects on body image, eating disorder cognitions, and risk of transitioning to other forms of disordered eating. Rapid weight loss itself can be psychologically destabilizing for some individuals with eating disorders. Any consideration of tirzepatide in BED must involve comprehensive psychiatric assessment and close monitoring by providers experienced in eating disorder treatment.
Tirzepatide currently has two FDA-approved indications, neither of which includes binge eating disorder. Under the brand name Mounjaro, it is approved as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. As Zepbound, it is approved for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbid condition, used alongside a reduced-calorie diet and increased physical activity. These approvals were based on robust clinical trial programs demonstrating efficacy and acceptable safety profiles in these specific populations.
The use of tirzepatide for binge eating disorder would constitute off-label prescribing. Off-label use of medications is legal and common in medical practice, occurring when physicians prescribe FDA-approved medications for conditions, populations, or dosing regimens not specifically included in the approved labeling. Physicians may prescribe medications off-label when they judge, based on available evidence and clinical experience, that the potential benefits outweigh the risks for a particular patient. However, off-label prescribing carries additional responsibilities, including thorough informed consent discussions about the lack of specific evidence for the condition being treated.
For tirzepatide and BED specifically, the evidence base supporting off-label use is currently minimal to nonexistent. This distinguishes it from some other off-label applications where substantial clinical trial data or extensive clinical experience supports the practice. Patients considering tirzepatide for BED should understand that they would essentially be participating in an uncontrolled clinical experiment, with unknown efficacy and potentially unforeseen risks in this population. Insurance coverage for off-label uses varies widely and often requires extensive documentation and prior authorization. Patients should verify coverage before initiating treatment, as the medication is expensive, with monthly list prices exceeding $1,000 without insurance coverage. No major professional guidelines, including those from the American Psychiatric Association and Academy for Eating Disorders, currently recommend GLP-1/GIP receptor agonists for the treatment of BED outside of research settings.
If you are considering tirzepatide for binge eating disorder, a comprehensive and collaborative approach with your healthcare team is essential. Ideally, your care should involve coordination between multiple specialists, including a primary care physician or endocrinologist familiar with tirzepatide, a psychiatrist or psychologist with expertise in eating disorders, and potentially a registered dietitian specializing in eating disorders. This multidisciplinary approach ensures that all aspects of BED—psychological, behavioral, nutritional, and medical—are addressed appropriately.
Before considering any pharmacological intervention for BED, ensure you have accessed evidence-based psychological treatments, particularly cognitive behavioral therapy, which has the strongest evidence base for BED. Medication should generally be considered as an adjunct to, not a replacement for, psychological treatment. If you and your providers decide to explore tirzepatide, the decision should be based on individual factors including the severity of binge eating, presence of comorbid obesity or type 2 diabetes, previous treatment responses, and your personal preferences and values. A thorough discussion should cover the lack of specific evidence for BED, potential benefits and risks, alternative treatment options, and the plan for monitoring both efficacy and safety.
Key monitoring parameters should include frequency and severity of binge episodes (using standardized measures such as the Binge Eating Scale or Eating Disorder Examination-Questionnaire), weight and metabolic parameters, gastrointestinal side effects, mood and anxiety symptoms, and importantly, any emergence of new disordered eating patterns such as restrictive eating or compensatory behaviors. Establish clear criteria for treatment success and predetermined timeframes for reassessment. If binge eating does not improve within 3-6 months, or if concerning side effects or new eating disorder symptoms emerge, discontinuation should be seriously considered.
Be alert to warning signs requiring higher levels of care, including suicidal thoughts, severe depression, significant dehydration, electrolyte abnormalities, or medical instability. These symptoms may necessitate immediate evaluation or referral to intensive outpatient, partial hospitalization, or inpatient treatment. Throughout treatment, maintain open communication with all members of your healthcare team, reporting both improvements and concerns promptly to ensure safe and effective care. Consider participation in clinical trials of tirzepatide for BED if available, as this provides structured monitoring and contributes to the evidence base for this potential application.
No, tirzepatide is not FDA-approved for binge eating disorder. It is only approved for type 2 diabetes (as Mounjaro) and chronic weight management (as Zepbound), and any use for BED would be off-label without supporting clinical trial evidence.
Lisdexamfetamine dimesylate (Vyvanse) is currently the only FDA-approved medication specifically for moderate to severe binge eating disorder in adults. Cognitive behavioral therapy remains the first-line treatment with the strongest evidence base.
Risks include gastrointestinal side effects (nausea, vomiting, diarrhea) that may worsen disordered eating, potential for pancreatitis and gallbladder disease, and unknown psychological impacts in eating disorder populations. There is insufficient data on safety and efficacy specifically for BED, and the medication could potentially trigger restrictive eating patterns.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.