LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide (Mounjaro for type 2 diabetes, Zepbound for weight management) is a dual GIP/GLP-1 receptor agonist that regulates blood sugar through glucose-dependent mechanisms. While tirzepatide low blood sugar risk is minimal when used alone, understanding hypoglycemia potential becomes critical when combined with insulin or sulfonylureas. This comprehensive guide examines tirzepatide's effects on blood glucose, identifies risk factors for hypoglycemia, and provides evidence-based strategies for prevention and management. Patients and clinicians must recognize that hypoglycemia risk depends primarily on concomitant medications rather than tirzepatide monotherapy.
Quick Answer: Tirzepatide carries low intrinsic risk of causing hypoglycemia when used alone due to its glucose-dependent mechanism, but risk increases significantly when combined with insulin or sulfonylureas.
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus (under the brand name Mounjaro) and chronic weight management (under the brand name Zepbound). This dual-acting medication represents a significant advancement in metabolic disease management.
The mechanism of action of tirzepatide involves stimulating insulin secretion from pancreatic beta cells in a glucose-dependent manner. This means insulin release occurs primarily when blood glucose levels are elevated, such as after meals. Simultaneously, tirzepatide suppresses glucagon secretion from pancreatic alpha cells in a glucose-dependent fashion. Glucagon normally raises blood glucose by promoting hepatic glucose production. The medication also slows gastric emptying (an effect that may attenuate with continued use), reducing the rate at which glucose enters the bloodstream after eating, and acts on central appetite centers to promote satiety and reduce caloric intake.
The glucose-dependent nature of tirzepatide's insulin secretion is a critical safety feature. Unlike sulfonylureas or exogenous insulin, which stimulate insulin release regardless of blood glucose levels, tirzepatide's activity diminishes as glucose concentrations approach normal ranges. This pharmacological characteristic theoretically reduces the risk of hypoglycemia (low blood sugar) when tirzepatide is used as monotherapy. Understanding this mechanism is essential for clinicians and patients to appropriately assess hypoglycemia risk and implement preventive strategies, particularly when tirzepatide is combined with other glucose-lowering medications.
It's important to note that tirzepatide is not indicated for the treatment of type 1 diabetes or diabetic ketoacidosis.
When used alone (as monotherapy), tirzepatide carries a low intrinsic risk of causing clinically significant hypoglycemia. Clinical trial data from the SURPASS program, which evaluated tirzepatide across various doses and patient populations, demonstrated that hypoglycemia rates with tirzepatide monotherapy were generally low. In the SURPASS-1 trial, clinically significant hypoglycemia (blood glucose <54 mg/dL) occurred infrequently in participants receiving tirzepatide monotherapy, with no severe hypoglycemic events (requiring assistance from another person) reported.
The glucose-dependent mechanism of tirzepatide explains this favorable safety profile. As blood glucose levels decline toward the normal range (approximately 70–100 mg/dL), the medication's stimulation of insulin secretion naturally decreases, and glucagon suppression is reduced. This built-in regulatory mechanism distinguishes tirzepatide from older diabetes medications such as sulfonylureas (glipizide, glyburide) and insulin, which can drive blood glucose below normal levels.
However, the risk profile changes substantially when tirzepatide is combined with other glucose-lowering agents, particularly insulin or insulin secretagogues. In the SURPASS-3 trial, which compared tirzepatide to insulin degludec in patients already taking metformin with or without an SGLT2 inhibitor, hypoglycemia rates remained relatively low with tirzepatide. Conversely, when tirzepatide was added to existing insulin glargine therapy in SURPASS-5, the incidence of clinically significant hypoglycemia was higher compared to placebo plus insulin, particularly at higher tirzepatide doses.
It is important to note that while tirzepatide itself has minimal hypoglycemic potential when used alone, the overall risk depends heavily on the patient's complete medication regimen and individual metabolic factors.
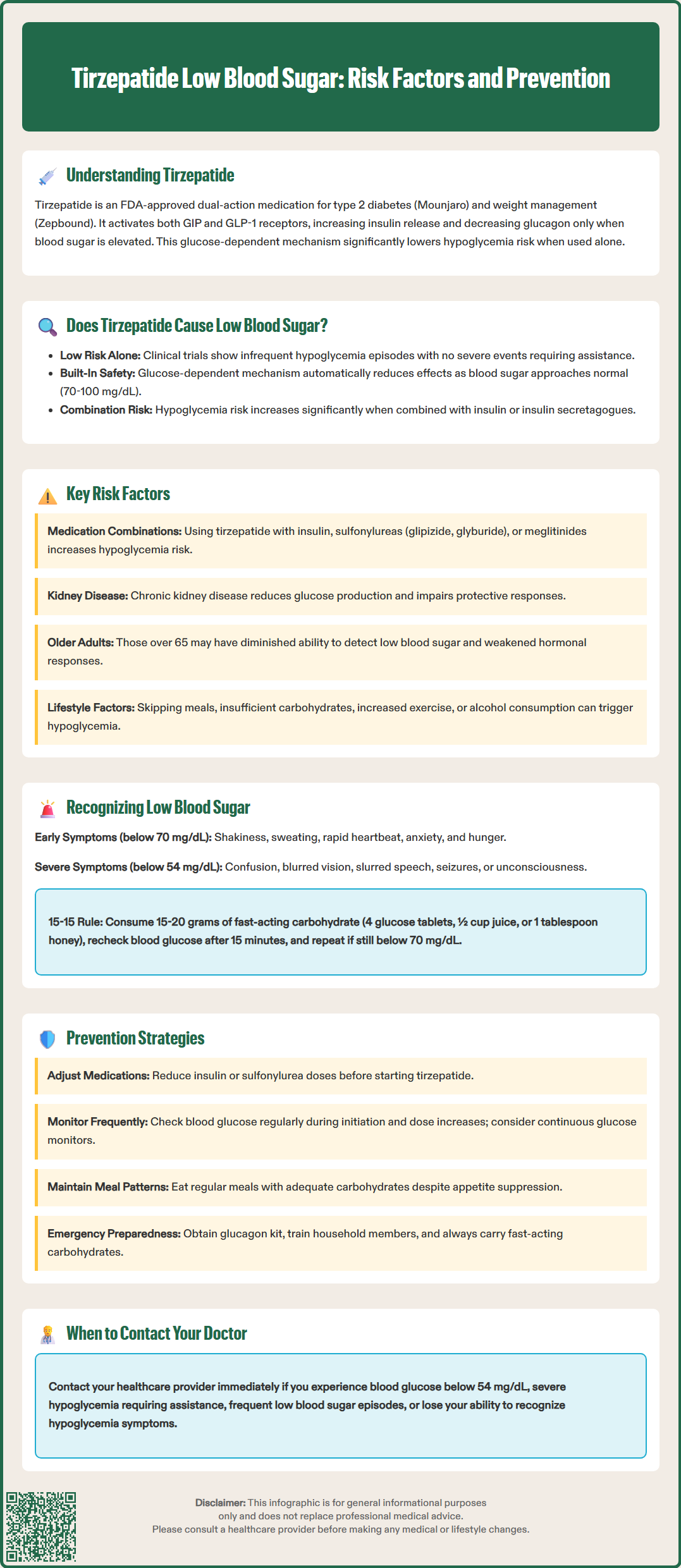
Several clinical factors significantly increase the risk of hypoglycemia in patients taking tirzepatide. The most important risk factor is concomitant use of insulin or insulin secretagogues (sulfonylureas such as glipizide, glyburide, or glimepiride, and meglitinides such as repaglinide). These medications independently increase hypoglycemia risk, and their combination with tirzepatide creates additive glucose-lowering effects. The FDA labeling recommends considering dose reduction of insulin or sulfonylureas when initiating tirzepatide to mitigate this risk.
Renal impairment represents another significant risk factor. While tirzepatide does not require dose adjustment based on kidney function, patients with chronic kidney disease have reduced gluconeogenesis capacity and impaired counter-regulatory responses to hypoglycemia. Additionally, these patients often take multiple medications that can affect glucose metabolism. Close monitoring is warranted in patients with advanced kidney disease.
Other important risk factors include advanced age (particularly over 65 years), where counter-regulatory hormone responses may be blunted and hypoglycemia awareness reduced; irregular meal patterns or inadequate carbohydrate intake, especially given tirzepatide's appetite-suppressing effects; increased physical activity without corresponding nutritional adjustment; alcohol consumption, which inhibits hepatic gluconeogenesis; and acute illness or infection that alters metabolic demands.
Patients with a history of severe hypoglycemia, hypoglycemia unawareness, or long-standing diabetes with autonomic neuropathy require particularly careful assessment. Healthcare providers should conduct comprehensive medication reviews and individualize treatment plans, considering the cumulative hypoglycemia risk from all sources rather than attributing risk to tirzepatide alone.
Hypoglycemia typically manifests through a predictable constellation of symptoms that result from both autonomic nervous system activation and neuroglycopenic effects. Early warning signs include trembling or shakiness, sweating, rapid heartbeat (palpitations), anxiety or nervousness, hunger, and irritability. These adrenergic symptoms generally occur when blood glucose falls below 70 mg/dL and serve as important warning signals prompting corrective action.
As blood glucose continues to decline below 54 mg/dL (the threshold for clinically significant hypoglycemia), neuroglycopenic symptoms emerge due to insufficient glucose delivery to the brain. These include difficulty concentrating, confusion, blurred vision, slurred speech, weakness, dizziness, and coordination problems. Severe hypoglycemia (requiring assistance from another person) can progress to altered consciousness, seizures, or loss of consciousness if untreated. Notably, some patients with long-standing diabetes develop impaired awareness of hypoglycemia, experiencing reduced or absent warning symptoms, which increases the risk of severe episodes.
Immediate management of hypoglycemia follows the "15-15 Rule" protocol. Patients experiencing symptoms with confirmed blood glucose below 70 mg/dL should consume 15–20 grams of fast-acting carbohydrate, such as 4 glucose tablets, 4 ounces (½ cup) of fruit juice or regular (non-diet) soda, or 1 tablespoon of honey or sugar. After 15 minutes, blood glucose should be rechecked. If it remains below 70 mg/dL, the treatment should be repeated. Once blood glucose normalizes, patients should consume a small snack containing protein and complex carbohydrates if the next meal is more than 1 hour away.
For severe hypoglycemia where the patient cannot safely swallow, glucagon administration is essential. Glucagon emergency kits (available as nasal spray, autoinjector, or traditional injection) should be prescribed for high-risk patients, and family members or caregivers should be trained in their use. Emergency medical services (911) should be contacted for any severe hypoglycemic episode. Patients should be advised never to drive or operate machinery when experiencing hypoglycemia symptoms, to carry fast-acting carbohydrates at all times, and to wear medical identification.
Prevention strategies for hypoglycemia in patients taking tirzepatide center on proactive medication management, patient education, and individualized monitoring. When initiating tirzepatide in patients already taking insulin or sulfonylureas, the FDA label recommends considering dose reduction of these medications. The specific adjustment should be individualized based on current glycemic control, hypoglycemia history, and treatment goals. This preemptive approach significantly reduces hypoglycemia risk during the titration phase.
Blood glucose monitoring is essential, particularly for patients on insulin or sulfonylureas, during tirzepatide initiation and dose escalation. Patients at higher risk should check blood glucose before meals, at bedtime, and whenever hypoglycemia symptoms occur. Those using continuous glucose monitoring (CGM) systems benefit from real-time glucose trends and predictive low glucose alerts, enabling earlier intervention. Healthcare providers should review glucose data regularly and adjust treatment regimens accordingly.
Patient education forms the cornerstone of hypoglycemia prevention. Patients should understand that tirzepatide's appetite-suppressing effects may reduce food intake, potentially increasing hypoglycemia risk if other glucose-lowering medications are not adjusted. They should be counseled to maintain regular meal patterns, avoid prolonged fasting, and consume adequate carbohydrates, particularly when physically active. Alcohol consumption should be limited and always accompanied by food, as alcohol inhibits the liver's ability to release glucose.
Healthcare providers should conduct comprehensive medication reviews at each visit, assessing for drug interactions and cumulative hypoglycemia risk. Patients should be provided with written hypoglycemia action plans, including symptom recognition, treatment protocols, and emergency contact information. High-risk patients should be prescribed glucagon emergency kits and receive training in their use, with similar training provided to household members.
Regular assessment of hypoglycemia awareness is important, as patients with impaired awareness may require more conservative glycemic targets and closer monitoring. Recurrent episodes of clinically significant hypoglycemia (blood glucose <54 mg/dL), any severe hypoglycemia, or development of hypoglycemia unawareness should prompt immediate contact with healthcare providers and possible referral to an endocrinologist. Patients should always carry fast-acting carbohydrates and wear medical identification. Collaboration between patients, caregivers, and healthcare teams ensures optimal safety while maximizing the therapeutic benefits of tirzepatide.
Tirzepatide monotherapy carries low intrinsic risk of causing clinically significant hypoglycemia due to its glucose-dependent mechanism of action. Clinical trials demonstrated infrequent hypoglycemia with tirzepatide alone, but risk increases substantially when combined with insulin or sulfonylureas.
Follow the 15-15 Rule: consume 15-20 grams of fast-acting carbohydrate (such as 4 glucose tablets or 4 ounces of juice), wait 15 minutes, then recheck blood glucose. If still below 70 mg/dL, repeat treatment. For severe hypoglycemia where you cannot swallow safely, use glucagon and call 911.
The FDA label recommends considering dose reduction of insulin or sulfonylureas when initiating tirzepatide to reduce hypoglycemia risk. The specific adjustment should be individualized based on your current glycemic control, hypoglycemia history, and treatment goals in consultation with your healthcare provider.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.