LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

A tirzepatide meal plan for weight loss focuses on nutrient-dense foods that support the medication's appetite-suppressing effects while ensuring adequate nutrition. Tirzepatide (Zepbound, Mounjaro) is a dual GIP/GLP-1 receptor agonist that significantly reduces hunger and slows gastric emptying, making strategic meal planning essential. Many patients experience profound appetite suppression, which can inadvertently lead to insufficient protein and micronutrient intake. A well-structured eating approach prioritizes lean proteins, non-starchy vegetables, and smaller frequent meals while minimizing foods that trigger gastrointestinal side effects. This article provides evidence-based guidance on building an effective meal plan that maximizes weight loss outcomes while maintaining nutritional adequacy and tolerability during tirzepatide therapy.
Quick Answer: A tirzepatide meal plan for weight loss should prioritize high-protein foods, smaller frequent meals, and nutrient-dense options while avoiding high-fat and ultra-processed foods that may worsen gastrointestinal side effects.
The medication works through multiple complementary mechanisms. As a GLP-1 receptor agonist, tirzepatide slows gastric emptying, which prolongs the sensation of fullness after meals and reduces appetite. It also acts on appetite-regulating centers in the hypothalamus, decreasing hunger signals and food cravings. The GIP component enhances insulin secretion in a glucose-dependent manner and may contribute additional metabolic benefits.
Clinical trials have demonstrated substantial weight loss with tirzepatide. In the SURMOUNT-1 trial, participants without diabetes lost an average of 15-20% of their body weight over 72 weeks, depending on the dose (5 mg, 10 mg, or 15 mg weekly). These results significantly exceed those seen with lifestyle modification alone.
The medication is administered as a once-weekly subcutaneous injection, with dosing typically starting at 2.5 mg and gradually increasing every four weeks to minimize gastrointestinal side effects. Maximum efficacy is generally achieved at doses of 10-15 mg weekly.
Important safety information: Tirzepatide has a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). The medication may reduce the effectiveness of oral contraceptives, particularly after initiation and dose increases; alternative or additional contraceptive methods are recommended for 4 weeks after these changes.
Creating a structured meal plan while taking tirzepatide requires balancing reduced appetite with adequate nutritional intake. Many patients experience significant appetite suppression, which can inadvertently lead to insufficient protein, vitamin, and mineral consumption if not carefully managed. A well-designed meal plan should prioritize nutrient density over caloric volume.
Key principles for meal planning include:
Protein prioritization: Aim for approximately 1.0-1.5 grams of protein per kilogram of ideal body weight daily, distributed across meals. For most adults, this translates to roughly 70-100 grams daily, though needs vary by individual. Adequate protein intake preserves lean muscle mass during weight loss and promotes satiety. Include lean meats, fish, eggs, Greek yogurt, legumes, and protein supplements if needed. Patients with chronic kidney disease should discuss protein targets with their healthcare provider.
Smaller, frequent meals: Rather than three large meals, consider 4-5 smaller eating occasions throughout the day. This approach accommodates reduced stomach capacity and helps maintain steady energy levels without overwhelming the digestive system.
Meal timing consistency: Establish regular eating times to ensure adequate nutrition despite diminished hunger cues. Many patients report forgetting to eat due to appetite suppression, which can compromise metabolic health and energy levels.
Hydration focus: Aim for 64-80 ounces of water daily for most adults (unless fluid-restricted), consumed between meals rather than with food to avoid premature fullness. Adequate hydration supports digestive function and helps manage constipation, a common side effect.
A practical approach involves planning meals in advance and tracking intake using a food diary or mobile application. This monitoring helps ensure nutritional adequacy and identifies patterns that may contribute to side effects. Working with a registered dietitian familiar with GLP-1 medications can provide personalized guidance tailored to individual needs, preferences, and weight loss goals. The American Diabetes Association recommends medical nutrition therapy as an integral component of weight management programs.
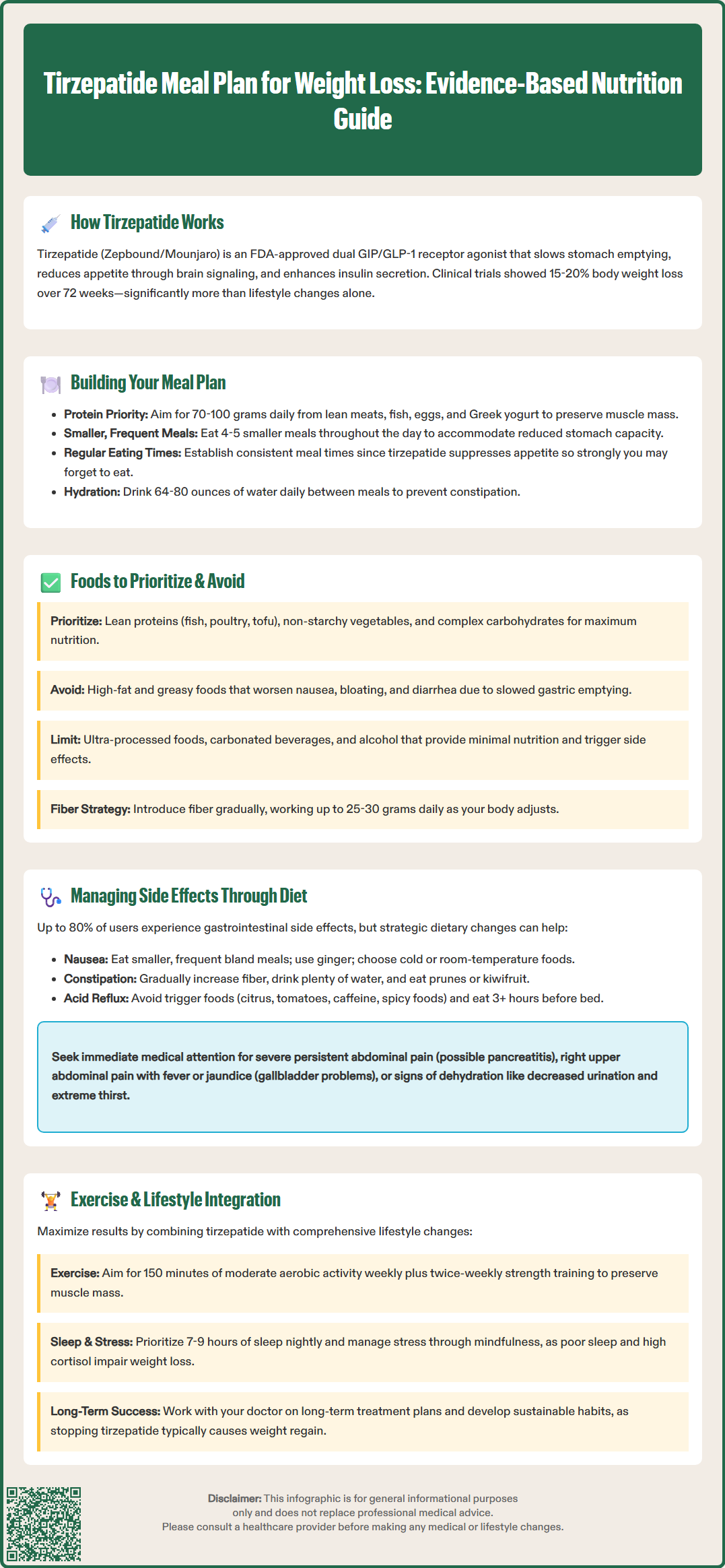
Selecting appropriate foods while taking tirzepatide can significantly impact both weight loss success and tolerability of the medication. The goal is to maximize nutritional value within a reduced caloric intake while minimizing gastrointestinal discomfort.
Foods to prioritize:
Lean proteins: Skinless poultry, fish (especially fatty fish rich in omega-3s), eggs, low-fat dairy, tofu, and legumes provide essential amino acids without excessive fat that may trigger nausea.
Non-starchy vegetables: Leafy greens, broccoli, cauliflower, peppers, and zucchini offer fiber, vitamins, and minerals with minimal calories. These should comprise a significant portion of each meal.
Complex carbohydrates: Whole grains like quinoa, brown rice, and oats provide sustained energy and fiber. Portion control remains important, but these foods support digestive health better than refined alternatives.
Healthy fats in moderation: Avocado, nuts, seeds, and olive oil provide essential fatty acids and fat-soluble vitamins. Use sparingly, as high-fat foods may exacerbate nausea.
Foods to limit or avoid:
High-fat, greasy foods: Fried foods, fatty cuts of meat, and heavy cream sauces can worsen nausea, bloating, and diarrhea due to delayed gastric emptying.
Ultra-processed foods: Items high in added sugars, sodium, and artificial ingredients provide minimal nutritional value and may trigger blood sugar fluctuations.
Carbonated beverages: These can increase bloating and gastric discomfort, particularly given the medication's effect on gastric emptying.
High-fiber foods initially: While fiber is beneficial, introducing too much too quickly can worsen gastrointestinal symptoms during dose escalation. Gradually increase fiber intake to the recommended 25-30 grams daily as tolerance improves.
Alcohol: Limit consumption as alcohol provides empty calories, may increase nausea, and can affect blood sugar regulation. For patients with diabetes taking insulin or sulfonylureas, alcohol increases hypoglycemia risk. Alcohol may also increase pancreatitis risk in susceptible individuals.
Individual tolerance varies considerably, so maintaining a food symptom diary helps identify personal triggers and optimize the meal plan accordingly. If dairy products cause discomfort, lactose-free alternatives may be better tolerated.
Gastrointestinal side effects are the most commonly reported adverse events with tirzepatide, affecting up to 80% of users to some degree. These include nausea, vomiting, diarrhea, constipation, abdominal pain, and decreased appetite. Strategic dietary modifications can significantly reduce the severity and frequency of these symptoms.
For nausea management:
Eat smaller portions more frequently rather than large meals. Bland, easily digestible foods such as crackers, toast, rice, and bananas (the BRAT diet components) may be better tolerated during periods of increased nausea, though this should be a short-term approach followed by resumption of balanced nutrition. Ginger tea or ginger supplements have evidence supporting anti-nausea effects. Avoid lying down immediately after eating, and consider eating your largest meal when nausea tends to be less severe. Cold or room-temperature foods often cause less nausea than hot, aromatic dishes.
For constipation:
Gradually increase dietary fiber through fruits, vegetables, and whole grains, aiming for 25-30 grams daily. Ensure adequate hydration, as fiber requires water to function effectively. Prunes, kiwifruit, and flaxseed have natural laxative properties. If dietary measures prove insufficient, discuss fiber supplements or stool softeners with your healthcare provider.
For diarrhea:
Temporarily reduce fat and fiber intake, focusing on easily digestible proteins and simple carbohydrates. Some patients may experience dairy sensitivity; if symptoms occur, try lactose-free alternatives. Probiotics may help restore gut microbiome balance, though evidence specific to tirzepatide remains limited.
For acid reflux:
Avoid trigger foods including citrus, tomatoes, chocolate, caffeine, and spicy dishes. Eat at least three hours before lying down, and consider elevating the head of your bed. Smaller, more frequent meals reduce gastric distension.
Important safety information: Stop taking tirzepatide and seek immediate medical attention if you experience severe persistent abdominal pain (with or without vomiting), as this may indicate pancreatitis. Also seek prompt medical care for symptoms of gallbladder problems (pain in the right upper abdomen, fever, yellowing of skin/eyes, or clay-colored stools), or signs of dehydration (decreased urination, dizziness, extreme thirst). Persistent vomiting or diarrhea can lead to acute kidney injury, especially in patients with pre-existing kidney disease or those taking medications that affect kidney function.
While tirzepatide produces significant weight loss through appetite suppression and metabolic effects, combining the medication with exercise and comprehensive lifestyle modifications optimizes outcomes and promotes long-term weight maintenance. The American College of Physicians and American Diabetes Association both emphasize that pharmacotherapy should complement, not replace, behavioral interventions.
Exercise recommendations:
Aim for at least 150 minutes of moderate-intensity aerobic activity weekly, such as brisk walking, cycling, or swimming, as recommended by the U.S. Department of Health and Human Services Physical Activity Guidelines. This can be divided into 30-minute sessions five days per week. Resistance training at least twice weekly is crucial for preserving lean muscle mass during weight loss. Tirzepatide-induced weight loss includes both fat and muscle; strength training helps maintain metabolic rate and functional capacity. Start gradually, especially if previously sedentary, and progressively increase intensity and duration as fitness improves.
Many patients report reduced energy levels, particularly during dose escalation. Schedule exercise when symptoms are least bothersome and ensure adequate pre-exercise nutrition to maintain consistency. If nausea is problematic, avoid vigorous exercise immediately after meals.
Behavioral and lifestyle strategies:
Sleep optimization: Aim for 7-9 hours nightly. Poor sleep disrupts appetite-regulating hormones and may affect weight management outcomes.
Stress management: Chronic stress promotes cortisol elevation, which can impair weight loss. Consider mindfulness practices, yoga, or counseling.
Behavioral therapy: Cognitive-behavioral approaches address emotional eating, develop coping strategies, and establish sustainable habits that persist beyond medication use.
Social support: Engage family members, join support groups, or work with a health coach to maintain accountability and motivation.
Regular monitoring: Track weight, measurements, and non-scale victories (improved energy, better sleep, reduced medication needs for comorbidities). Regular follow-up with healthcare providers ensures appropriate dose titration and addresses emerging concerns.
Long-term considerations:
Tirzepatide is indicated for chronic weight management; clinical studies show that discontinuation typically results in weight regain. Developing sustainable eating patterns and exercise habits during treatment creates a foundation for weight maintenance. Discuss long-term treatment plans with your physician, including potential duration of therapy, maintenance dosing strategies, and transition plans if discontinuation becomes necessary. The goal extends beyond weight loss to achieving improved metabolic health, reduced cardiovascular risk, and enhanced quality of life.
Aim for approximately 1.0-1.5 grams of protein per kilogram of ideal body weight daily, typically 70-100 grams for most adults. Adequate protein intake preserves lean muscle mass during weight loss and should be distributed across multiple meals throughout the day.
Limit high-fat and greasy foods, ultra-processed items, carbonated beverages, and alcohol, as these can worsen gastrointestinal side effects like nausea, bloating, and diarrhea. Focus instead on lean proteins, non-starchy vegetables, and complex carbohydrates in appropriate portions.
Eat smaller, more frequent meals with bland, easily digestible foods like crackers, toast, and rice during periods of increased nausea. Cold or room-temperature foods are often better tolerated than hot meals, and ginger tea may provide additional relief.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.