LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Some patients taking tirzepatide (Mounjaro, Zepbound) report experiencing taste changes, including metallic or altered taste sensations. While not formally listed as a common side effect in FDA prescribing information, these taste disturbances may occur in certain individuals. Understanding why tirzepatide might affect taste perception and knowing effective management strategies can help patients maintain treatment adherence and quality of life. This article explores the potential mechanisms behind taste changes with tirzepatide, practical solutions for managing this symptom, and guidance on when to contact your healthcare provider.
Quick Answer: Tirzepatide may cause taste changes including metallic or altered taste sensations in some patients, though this is not formally documented as a common side effect in FDA labeling.
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus (Mounjaro) and chronic weight management (Zepbound). For weight management, it is indicated for adults with a BMI ≥30 kg/m², or ≥27 kg/m² with at least one weight-related comorbidity, as an adjunct to diet and exercise. This once-weekly subcutaneous injection works by enhancing insulin secretion, suppressing glucagon release, slowing gastric emptying, and reducing appetite.
Importantly, tirzepatide carries a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2).
The most commonly reported adverse effects of tirzepatide are gastrointestinal in nature. In clinical trials, nausea occurred in 24-37% of patients, diarrhea in 15-22%, vomiting in 8-24%, and constipation in 11-21%, with rates varying by dose. These gastrointestinal side effects are typically mild to moderate in severity and tend to diminish over time as the body adjusts to the medication. The incidence is highest during dose escalation periods.
While the FDA-approved prescribing information does not specifically list taste disturbances as a common adverse effect, some patients have reported experiencing changes in taste perception, including metallic taste or altered taste sensations. It is important to note that there is no official established link between tirzepatide and taste changes in the product labeling, and the exact prevalence of this symptom remains unclear. However, patient reports suggest that taste alterations may occur in some individuals taking this medication, warranting further discussion and appropriate management strategies.
The mechanism by which tirzepatide might cause taste disturbances is not definitively established, as this side effect is not formally documented in clinical trial data. However, several plausible hypotheses exist based on the drug's pharmacological properties and known effects on the gastrointestinal system.
Tirzepatide's action on GLP-1 and GIP receptors significantly slows gastric emptying, which may potentially contribute to gastroesophageal reflux in susceptible individuals. This reflux could theoretically result in a bitter or metallic taste in the mouth, particularly when lying down or after meals, though this connection requires further study.
Additionally, the gastrointestinal side effects commonly associated with tirzepatide—particularly nausea and vomiting—can independently affect taste sensation. Nausea itself is often accompanied by dysgeusia (altered taste perception), and the metabolic changes associated with reduced food intake may influence taste bud function. Dehydration secondary to vomiting or diarrhea can also contribute to dry mouth and altered taste.
Another potential contributor to taste changes may be ketosis resulting from reduced carbohydrate intake and weight loss while taking tirzepatide. This metabolic state can sometimes cause a metallic or fruity taste in the mouth and may be managed with adequate hydration and balanced nutrition.
It is worth considering that taste changes may be indirectly related to tirzepatide rather than a direct pharmacological effect. For instance, patients experiencing significant nausea may develop food aversions or notice tastes more acutely. Individual patient factors, including concurrent medications, nutritional status, and underlying health conditions, may also play a role in taste disturbances.
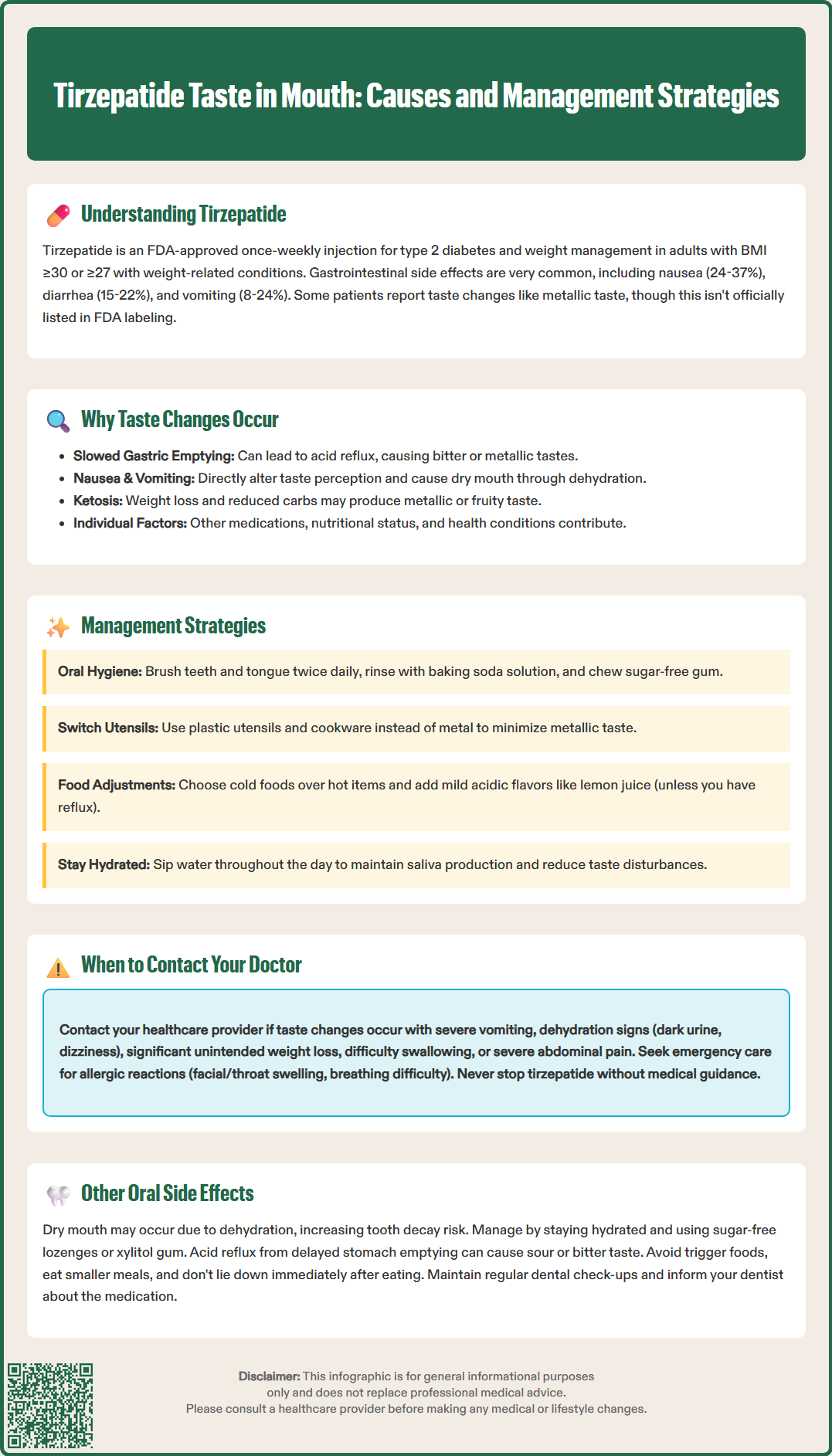
If you experience taste changes while taking tirzepatide, several practical strategies may help minimize this bothersome symptom. These approaches focus on oral hygiene, dietary modifications, and symptom management techniques that have proven helpful for patients experiencing medication-related taste disturbances.
Oral hygiene measures are fundamental to managing taste alterations. Brush your teeth at least twice daily with fluoride toothpaste, and consider brushing your tongue gently to remove any coating that may contribute to taste changes. Rinsing your mouth with a baking soda solution (one-quarter teaspoon in one cup of warm water) several times daily can help neutralize metallic tastes. Some patients find that using an alcohol-free mouthwash or chewing sugar-free gum (particularly those containing xylitol) or mints can provide temporary relief and stimulate saliva production.
Dietary modifications can also be beneficial. If you experience a metallic taste, try using plastic utensils instead of metal ones, and avoid cooking with metal pots and pans when possible. Consuming cold foods and beverages may be more palatable than hot items. Adding mild acidic flavors such as lemon juice to meals can help mask unpleasant tastes, though be cautious with acidic foods if you experience reflux symptoms. Marinating meats in fruit juices or wine before cooking may improve their palatability. Stay well-hydrated by sipping water throughout the day, as adequate hydration helps maintain normal saliva production and can reduce taste disturbances.
Additional strategies include eating smaller, more frequent meals to minimize nausea-related taste changes, and maintaining good nutrition despite altered taste perception. If taste changes are affecting your food intake significantly or persist beyond a few weeks, consider consulting with your healthcare provider and a registered dietitian who can help you develop an eating plan that ensures adequate nutrition while accommodating your taste preferences. Some patients report that taste disturbances improve as their body adjusts to tirzepatide, particularly after the initial weeks of treatment or following dose increases.
While taste changes associated with tirzepatide are generally not considered medically serious, certain circumstances warrant prompt communication with your healthcare provider. Understanding when to seek medical advice ensures appropriate monitoring and management of your treatment.
You should contact your healthcare provider if taste changes are accompanied by other concerning symptoms. Seek medical attention if you experience:
Severe or persistent nausea and vomiting that prevents adequate fluid or food intake
Signs of dehydration, including decreased urination, dark urine, dizziness, or extreme thirst
Significant unintended weight loss beyond expected therapeutic effects
Difficulty swallowing or persistent throat pain
Symptoms suggestive of pancreatitis, such as severe abdominal pain radiating to the back (stop taking tirzepatide and seek urgent care)
Right upper abdominal pain, fever, or yellowing of skin/eyes (possible gallbladder disease)
Call 911 or seek emergency care immediately for:
Signs of allergic reaction, including facial/throat swelling, difficulty breathing, or severe rash
Severe abdominal pain with vomiting that prevents keeping down any fluids
Additionally, if you have diabetes, report any new or worsening vision changes and maintain regular retinal screening appointments. If taste disturbances are significantly impacting your quality of life, nutritional intake, or medication adherence, discuss this with your healthcare provider. They may consider adjusting your dose escalation schedule, providing additional supportive medications for nausea, or evaluating whether other factors might be contributing to your symptoms.
It is important to continue taking tirzepatide as prescribed unless specifically instructed otherwise by your healthcare provider. Do not discontinue the medication without medical guidance, as abrupt cessation may affect your diabetes control or weight management goals. Your provider can work with you to develop an individualized management plan that addresses bothersome side effects while maintaining therapeutic benefits.
Beyond taste disturbances, tirzepatide may be associated with other oral and oropharyngeal symptoms that patients should be aware of, though these are not extensively documented in the prescribing information as common adverse effects.
Dry mouth (xerostomia) may occur in some patients taking tirzepatide, potentially related to dehydration from gastrointestinal side effects or changes in fluid balance. Reduced saliva production can contribute to altered taste perception, difficulty swallowing, and increased risk of dental caries. Maintaining adequate hydration, using sugar-free lozenges or xylitol-containing gum to stimulate saliva production, and practicing meticulous oral hygiene can help manage this symptom. If dry mouth persists, consult your dentist, who may recommend saliva substitutes or additional fluoride measures. For severe cases, your healthcare provider may consider prescription options after proper evaluation.
Nausea-related oral symptoms are common given tirzepatide's gastrointestinal effects. Patients may experience increased salivation (sialorrhea) as a prodrome to nausea or vomiting, or conversely, may notice reduced appetite affecting their oral intake patterns. The sensation of food sitting heavily in the stomach due to delayed gastric emptying can create an unpleasant oral awareness or aversion to eating.
Gastroesophageal reflux symptoms may manifest with oral components, including a sour or bitter taste, particularly upon waking or after meals. This may occur in part because tirzepatide's effect on gastric emptying could potentially influence reflux patterns in susceptible individuals. Managing reflux through dietary modifications (avoiding trigger foods, eating smaller meals, not lying down immediately after eating) may help. If you experience persistent reflux symptoms, consult your healthcare provider before starting regular use of over-the-counter antacids or acid-suppressing medications, as these require appropriate medical oversight.
Patients should maintain regular dental check-ups while taking tirzepatide, as changes in eating patterns, potential dry mouth, and altered oral hygiene habits related to nausea may affect dental health. Inform your dentist about your tirzepatide use so they can provide appropriate preventive care and monitoring.
Metallic or altered taste is not formally listed as a common side effect in FDA prescribing information for tirzepatide, though some patients report experiencing taste changes. The exact prevalence remains unclear as it was not specifically documented in clinical trials.
Many patients report that taste disturbances improve as their body adjusts to tirzepatide, particularly after the initial weeks of treatment or following dose increases. If taste changes persist beyond a few weeks or significantly affect nutrition, consult your healthcare provider.
Effective strategies include rinsing with baking soda solution, using plastic utensils instead of metal, chewing sugar-free gum, staying well-hydrated, consuming cold foods, and maintaining excellent oral hygiene. Adding mild acidic flavors like lemon juice to meals may also help mask unpleasant tastes.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.