LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide is a groundbreaking medication that addresses two major health challenges: type 2 diabetes and obesity. Approved by the FDA and marketed as Mounjaro for diabetes and Zepbound for weight management, tirzepatide works through a unique dual-action mechanism that sets it apart from traditional treatments. By simultaneously activating two incretin hormone receptors—GIP and GLP-1—this once-weekly injectable medication helps regulate blood sugar, reduce appetite, and promote significant metabolic improvements. Understanding what tirzepatide does and how it works is essential for patients and clinicians considering this therapeutic option for chronic metabolic conditions.
Quick Answer: Tirzepatide is a dual GIP/GLP-1 receptor agonist that lowers blood sugar, promotes weight loss, and improves metabolic health in adults with type 2 diabetes and obesity.
Tirzepatide is a novel injectable medication approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management in adults. Marketed under the brand names Mounjaro (for diabetes) and Zepbound (for weight management and obstructive sleep apnea), tirzepatide represents a significant advancement in metabolic disease therapy due to its dual mechanism of action.
Unlike traditional diabetes medications that target a single pathway, tirzepatide functions as a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist. This means it activates two distinct incretin hormone receptors simultaneously. GIP and GLP-1 are naturally occurring hormones released by the intestine in response to food intake, and they play crucial roles in glucose regulation and appetite control.
The pharmacological action of tirzepatide includes several key mechanisms. First, it enhances insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning insulin release occurs primarily when blood glucose levels are elevated. While this reduces hypoglycemia risk when used alone, the risk increases when combined with insulin or sulfonylureas. Second, it suppresses glucagon secretion from pancreatic alpha cells, thereby decreasing hepatic glucose production. Third, tirzepatide slows gastric emptying, which moderates the rate at which glucose enters the bloodstream after meals. This delayed gastric emptying can affect the absorption of oral medications, particularly oral contraceptives. Finally, it acts on central appetite regulation centers in the brain, promoting satiety and reducing caloric intake.
Tirzepatide is administered once weekly via subcutaneous injection, typically in the abdomen, thigh, or upper arm. The medication has a half-life of approximately five days, allowing for sustained therapeutic effects throughout the week. Common side effects include nausea, vomiting, diarrhea, and constipation, which are typically most pronounced during dose escalation periods.
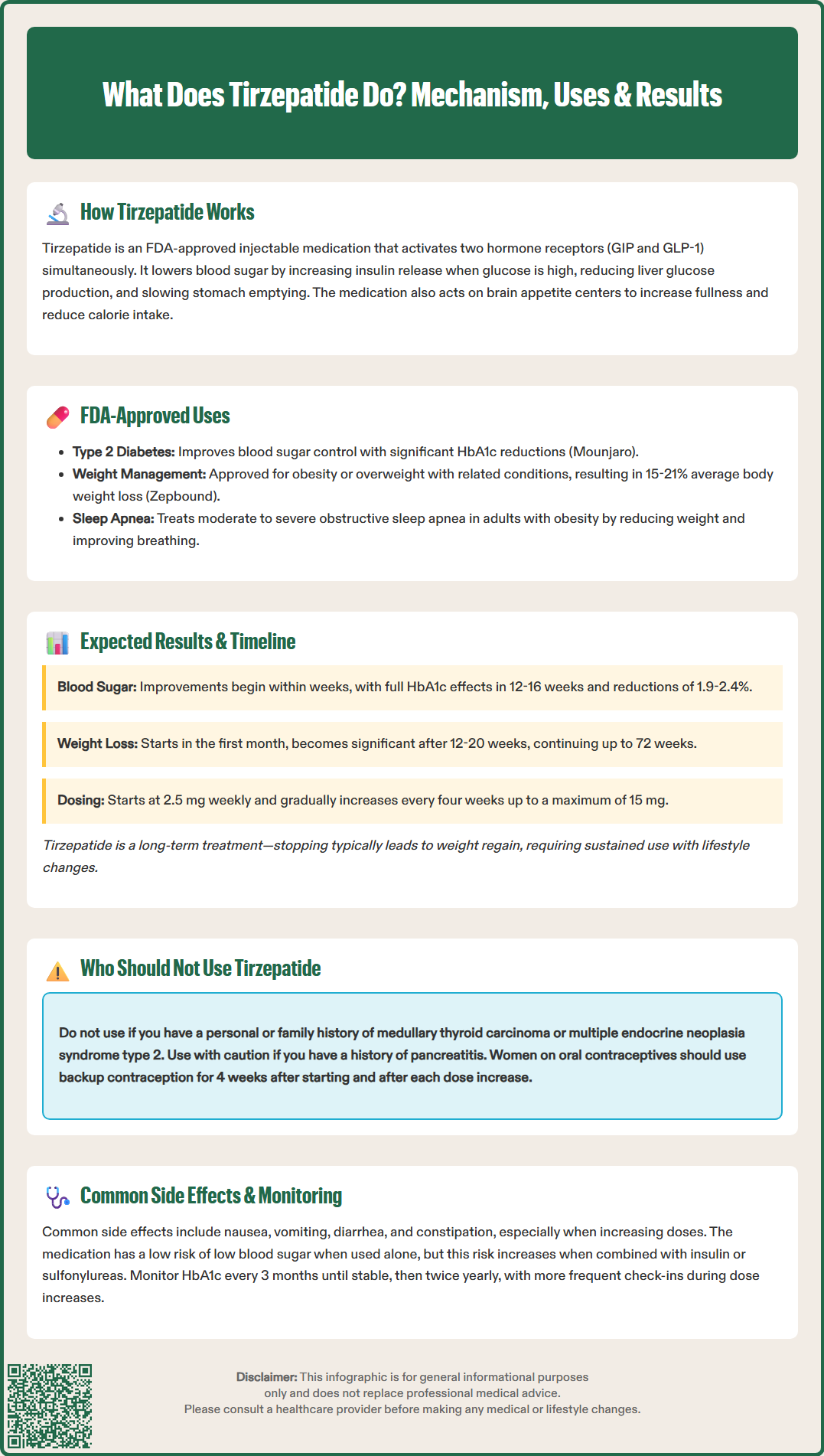
Tirzepatide has three FDA-approved indications, each addressing significant public health concerns in the United States. The first approved indication is as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. Clinical trials in the SURPASS program have demonstrated that tirzepatide produces substantial reductions in hemoglobin A1c (HbA1c), a key marker of long-term blood glucose control, with many patients achieving target HbA1c levels below 7%.
The second FDA-approved indication is for chronic weight management in adults with obesity (body mass index ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbid condition such as hypertension, dyslipidemia, or obstructive sleep apnea. When used for weight management, tirzepatide is prescribed as Zepbound and should be combined with a reduced-calorie diet and increased physical activity. In the SURMOUNT-1 trial, patients lost an average of 15-21% of their initial body weight over 72 weeks, with results varying by dose and individual factors.
The third FDA-approved indication, granted in 2024, is for the treatment of moderate to severe obstructive sleep apnea (OSA) in adults with obesity. Zepbound improves the apnea-hypopnea index primarily through weight reduction in these patients.
Beyond these approved indications, tirzepatide may offer additional metabolic benefits. Studies have shown improvements in cardiovascular risk factors including blood pressure, lipid profiles, and markers of inflammation. Research also suggests benefits in reducing liver fat content in patients with non-alcoholic fatty liver disease/metabolic dysfunction-associated steatohepatitis (MASH), though these are not currently approved indications and represent areas of ongoing research.
It is important to note that tirzepatide is not approved for type 1 diabetes or diabetic ketoacidosis. Additionally, while weight loss occurs in most patients treated for diabetes, the medication should only be prescribed for weight management or OSA under the specific Zepbound indication when appropriate criteria are met.
Patients beginning tirzepatide therapy should understand that results develop progressively over several months, with the medication requiring gradual dose escalation to optimize efficacy while minimizing gastrointestinal side effects. The typical starting dose is 2.5 mg once weekly for four weeks, serving primarily as a tolerability dose rather than a therapeutic dose. After this initial period, the dose is increased to 5 mg weekly, with further increases to 7.5 mg, 10 mg, 12.5 mg, and a maximum of 15 mg occurring at four-week intervals based on individual response and tolerability.
For glycemic control in type 2 diabetes, patients typically observe measurable improvements in fasting blood glucose within the first few weeks of treatment. However, the full effect on HbA1c becomes apparent after approximately 12-16 weeks of therapy. The SURPASS clinical trials have shown mean HbA1c reductions ranging from 1.9% to 2.4% depending on the dose, with higher doses generally producing greater glycemic improvements. Many patients achieve HbA1c levels below 7%, and a substantial proportion reach levels below 5.7%, which falls within the non-diabetic range.
Weight loss follows a more gradual trajectory. Patients generally begin noticing weight reduction within the first month, but significant changes become more apparent after 12-20 weeks. Weight loss continues progressively throughout the first year of treatment, with peak effects typically observed around 72 weeks. In the SURMOUNT-1 trial, patients treated with the highest doses lost an average of 15-21% of their baseline body weight. Individual results vary considerably based on adherence to dietary modifications, physical activity levels, baseline metabolic status, and genetic factors.
Patients should be counseled that tirzepatide is not a short-term intervention but rather a long-term treatment for chronic metabolic conditions. The SURMOUNT-4 trial demonstrated that discontinuation of the medication typically results in gradual weight regain, emphasizing the importance of sustained therapy alongside lifestyle modifications. For diabetes management, the American Diabetes Association recommends monitoring HbA1c approximately every 3 months until stable and at goal, then at least twice yearly if stable. More frequent follow-up is advised during dose escalation periods, particularly for weight management.
Tirzepatide carries several absolute and relative contraindications that clinicians must carefully evaluate before prescribing. The primary absolute contraindication is a personal or family history of medullary thyroid carcinoma (MTC) or multiple endocrine neoplasia syndrome type 2 (MEN 2). This contraindication stems from animal studies showing that GLP-1 receptor agonists cause thyroid C-cell tumors in rodents. While there is no definitive evidence that tirzepatide causes MTC in humans, the FDA requires a boxed warning, and the medication should not be used in patients with these risk factors. Patients should be counseled to report symptoms such as a neck mass, dysphagia, dyspnea, or persistent hoarseness.
Tirzepatide is also contraindicated in patients with a known hypersensitivity to the medication or any of its components. Serious hypersensitivity reactions, including anaphylaxis and angioedema, have been reported with GLP-1 receptor agonists, and patients experiencing such reactions should discontinue tirzepatide immediately and seek emergency medical care.
Several clinical conditions warrant caution. Patients with a history of pancreatitis should be carefully evaluated, as GLP-1 receptor agonists have been associated with acute pancreatitis in some cases. Tirzepatide should be discontinued if pancreatitis is suspected, and patients should be educated to recognize symptoms including severe, persistent abdominal pain that may radiate to the back. Tirzepatide is not recommended for patients with severe gastroparesis due to its effects on gastric emptying.
Regarding renal function, no dose adjustment is required for patients with renal impairment, including those with end-stage renal disease. However, patients should be monitored for potential dehydration from gastrointestinal side effects, which could affect kidney function.
Tirzepatide should be used with caution in patients taking oral contraceptives due to delayed gastric emptying. Non-oral contraception or backup contraception is recommended for 4 weeks after initiation and after each dose increase. Women should discontinue tirzepatide at least 1 month before a planned pregnancy and immediately if pregnancy occurs. For breastfeeding women, the benefits and risks should be carefully weighed.
Patients with a history of diabetic retinopathy should be monitored closely, as rapid improvements in glycemic control have been associated with temporary worsening of retinopathy. When used with insulin or sulfonylureas, tirzepatide increases the risk of hypoglycemia; dose reductions of these medications should be considered. Tirzepatide may also increase the risk of gallbladder disease, including cholelithiasis and cholecystitis. Concomitant use with other GLP-1 receptor agonists is not recommended.
Patients typically notice improvements in fasting blood glucose within the first few weeks, while full effects on HbA1c become apparent after 12-16 weeks. Weight loss begins within the first month but becomes more significant after 12-20 weeks, with peak effects around 72 weeks.
No, tirzepatide is not approved for type 1 diabetes or diabetic ketoacidosis. It is FDA-approved only for type 2 diabetes, chronic weight management in adults with obesity or overweight with comorbidities, and moderate-to-severe obstructive sleep apnea in adults with obesity.
Discontinuing tirzepatide typically results in gradual weight regain and potential worsening of glycemic control in patients with diabetes. Tirzepatide is intended as a long-term treatment for chronic metabolic conditions and should be combined with sustained lifestyle modifications for optimal results.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.