LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Nausea is the most common side effect of semaglutide, affecting up to 44% of patients taking Wegovy and approximately 15-20% of those on Ozempic. This GLP-1 receptor agonist slows gastric emptying and may directly stimulate nausea centers in the brainstem. While often temporary and most pronounced during dose escalation, semaglutide-related nausea can significantly impact quality of life. Fortunately, evidence-based dietary modifications, medication options, and dosing strategies can effectively manage this side effect. Understanding what helps with nausea from semaglutide empowers patients and clinicians to optimize treatment tolerability while maintaining therapeutic benefits for diabetes management and weight loss.
Quick Answer: Dietary modifications, gradual dose titration, and antiemetic medications effectively manage semaglutide-related nausea in most patients.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (under the brand name Ozempic) and chronic weight management (Wegovy). Nausea is the most commonly reported adverse effect, occurring in approximately 15-20% of patients taking Ozempic and up to 44% of patients taking Wegovy at the 2.4 mg dose during clinical trials. Understanding the proposed mechanisms behind this side effect can help patients and clinicians develop effective management strategies.
The primary reason semaglutide appears to cause nausea relates to its pharmacological action on the gastrointestinal system. GLP-1 receptors are present throughout the digestive tract, and when activated by semaglutide, they slow gastric emptying—the rate at which food moves from the stomach into the small intestine. This delayed emptying creates a sensation of fullness that contributes to weight loss but can also trigger nausea, particularly after meals. Additionally, semaglutide may act on receptors in the brainstem's area postrema, a region involved in the vomiting reflex, which may directly stimulate nausea sensations.
The intensity of nausea typically correlates with dose escalation and tends to be most pronounced during the first few weeks of treatment or following dose increases. Many patients experience improvement as their bodies adapt to the medication, though this adaptation may take longer than 8 weeks, particularly during Wegovy's 16-week titration period. Individual tolerance varies considerably, and some patients may experience persistent nausea that requires intervention. Factors such as eating habits, meal composition, and the rate of dose titration can significantly influence the severity of gastrointestinal side effects. Notably, semaglutide is not recommended for patients with severe gastrointestinal disease, such as severe gastroparesis, per FDA labeling.
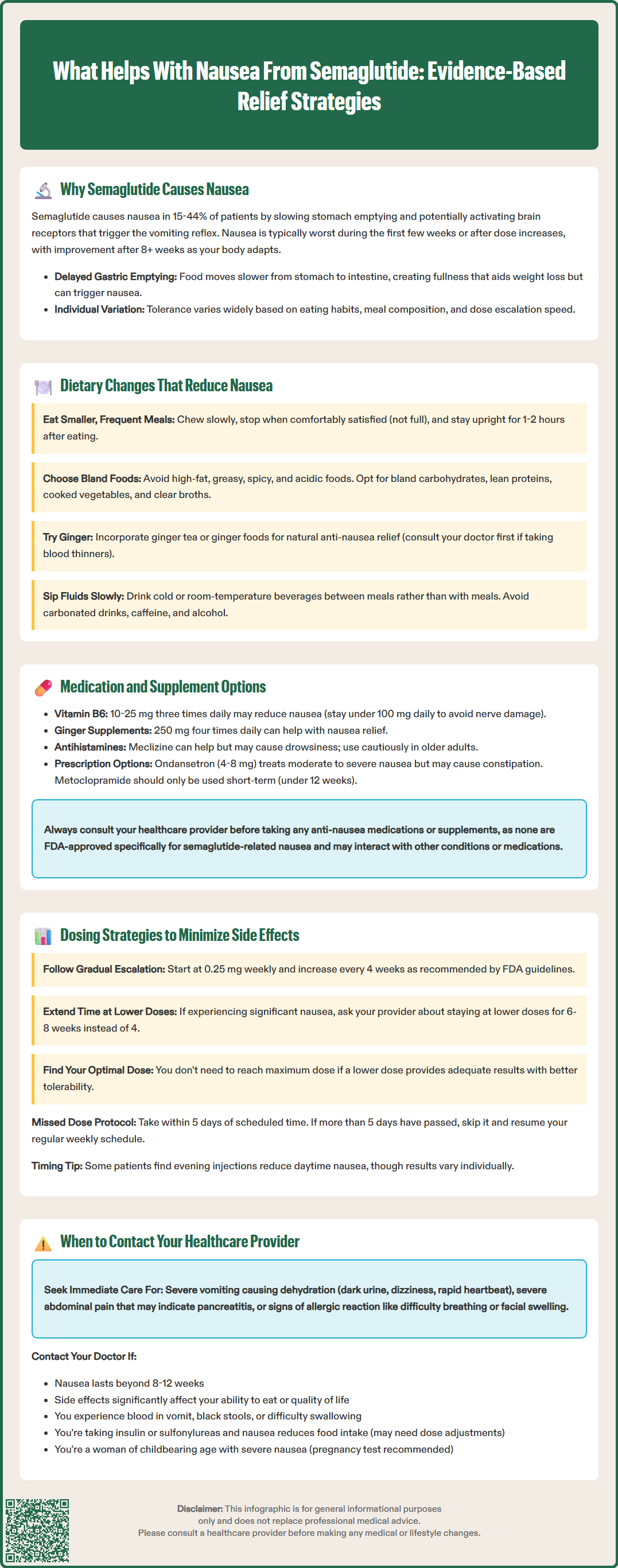
Modifying eating patterns and food choices represents the first-line approach to managing semaglutide-related nausea. These dietary strategies work by accommodating the medication's effect on gastric emptying and reducing triggers that exacerbate gastrointestinal discomfort.
Meal size and frequency adjustments are particularly effective. Patients should consume smaller, more frequent meals throughout the day rather than three large meals. Eating slowly and chewing food thoroughly allows better recognition of satiety signals and prevents overfilling the stomach. Stopping when comfortably satisfied—rather than completely full—helps avoid the uncomfortable bloating that can worsen nausea. Remaining upright for 1-2 hours after eating may also help reduce symptoms.
Food composition matters significantly. High-fat and greasy foods delay gastric emptying further and should be limited, especially during the initial treatment period. Similarly, spicy, acidic, or heavily seasoned foods may irritate the stomach lining and intensify nausea. Instead, patients should focus on:
Bland, easily digestible carbohydrates (crackers, toast, rice, oatmeal)
Lean proteins in moderate portions (chicken, fish, eggs)
Cooked vegetables rather than raw (lower fiber is often better tolerated)
Clear broths and soups
Ginger tea or ginger-containing foods, which have natural anti-nausea properties (though patients taking blood thinners should consult their healthcare provider before using ginger supplements due to potential interactions)
Hydration strategies also play a crucial role. Patients should sip fluids slowly throughout the day rather than drinking large volumes at once. Cold or room-temperature beverages are often better tolerated than hot drinks. Avoiding carbonated beverages, caffeine, and alcohol can reduce gastric irritation. Some patients find that drinking fluids between meals rather than with meals helps minimize the sensation of fullness and associated nausea. If vomiting occurs, oral rehydration solutions containing electrolytes may be preferable to plain water.
When dietary modifications prove insufficient, pharmacological interventions may be necessary to manage persistent nausea. Healthcare providers can recommend several options, though patients should always consult their prescriber before adding any medications or supplements to their regimen, as most are not FDA-approved specifically for semaglutide-related nausea.
Over-the-counter options provide relief for many patients. Vitamin B6 (pyridoxine) at doses of 10–25 mg three times daily has demonstrated anti-nausea effects and is generally well-tolerated, though patients should not exceed 100 mg daily due to risk of peripheral neuropathy with long-term high doses. Ginger supplements (250 mg four times daily) offer a natural alternative with some evidence for various types of nausea, but patients should discuss with their provider if they take anticoagulants or have gallbladder disease. Antihistamines such as meclizine (12.5–25 mg) or dimenhydrinate may help, though drowsiness and anticholinergic effects are common side effects that limit daytime use, particularly in older adults.
Prescription antiemetics may be warranted for moderate to severe nausea. Ondansetron (4–8 mg as needed) is a serotonin 5-HT3 receptor antagonist that can be effective for GLP-1 agonist-related symptoms, though it may cause constipation, headache, and can prolong the QT interval in susceptible individuals. Metoclopramide (5-10 mg) may be considered for short-term use (less than 12 weeks) under close supervision, as it carries a boxed warning for tardive dyskinesia risk with prolonged use. Prochlorperazine (5–10 mg) represents another option, though it carries risks of extrapyramidal side effects.
Acid-reducing medications such as proton pump inhibitors (PPIs) like omeprazole or H2 blockers like famotidine may benefit patients who experience nausea accompanied by acid reflux or heartburn. However, these medications address only the acid component and do not directly treat nausea itself. Patients should use the lowest effective dose for the shortest duration necessary, as long-term PPI use carries potential risks including nutrient malabsorption and increased infection susceptibility.
The FDA-approved prescribing information for semaglutide emphasizes gradual dose escalation to improve gastrointestinal tolerability. Adhering to recommended titration schedules significantly reduces the incidence and severity of nausea compared to rapid dose increases.
Standard titration protocols for Ozempic (diabetes indication) begin with 0.25 mg once weekly for four weeks, followed by an increase to 0.5 mg weekly. If additional glycemic control is needed, the dose may be increased to 1 mg weekly after at least four weeks, and potentially to 2 mg weekly after another four weeks at 1 mg. For Wegovy (weight management), the schedule starts at 0.25 mg weekly and increases monthly through 0.5 mg, 1 mg, 1.7 mg, and finally to the maintenance dose of 2.4 mg weekly. These gradual increases allow the gastrointestinal system to adapt progressively.
Individualized titration may be necessary for patients experiencing significant nausea. Healthcare providers can extend the time spent at lower doses beyond the standard four-week intervals, allowing 6–8 weeks at each level if needed. For Wegovy specifically, patients who cannot tolerate the 2.4 mg dose may use 1.7 mg as a maintenance dose. There is no clinical urgency to reach the maximum dose if adequate therapeutic benefit is achieved at lower doses with better tolerability.
Injection timing and missed doses should be managed according to FDA guidelines. If a dose is missed, it should be administered within 5 days of the scheduled dose. If more than 5 days have passed, skip the missed dose and administer the next dose on the regularly scheduled day. Some patients report that evening injections may reduce daytime nausea, though this is anecdotal and varies by individual. The injection site (abdomen, thigh, or upper arm) does not significantly affect nausea, though rotating sites prevents injection-site reactions. Patients should maintain consistency in their weekly injection schedule.
While nausea is an expected side effect of semaglutide, certain symptoms warrant prompt medical evaluation to rule out serious complications or determine whether treatment modification is necessary.
Immediate medical attention is required if patients experience severe, persistent vomiting that prevents adequate fluid intake, as this can lead to dehydration, electrolyte imbalances, and potentially acute kidney injury. Warning signs of dehydration include decreased urination, dark urine, dizziness upon standing, rapid heartbeat, and extreme thirst. Severe abdominal pain, particularly if localized to the upper abdomen and radiating to the back, may indicate pancreatitis—a rare but serious adverse effect of GLP-1 agonists that requires emergency evaluation. Right upper quadrant pain, especially if accompanied by fever or yellowing of the skin/eyes, could indicate gallbladder disease, which occurs more frequently with GLP-1 agonists. Severe abdominal distension, inability to pass gas or stool, or worsening constipation may signal intestinal obstruction or ileus. Any signs of allergic reaction, including difficulty breathing, facial swelling, or widespread rash, necessitate immediate emergency care.
Scheduled consultation is appropriate when nausea persists beyond 8–12 weeks without improvement, significantly impacts quality of life or nutritional intake, or is accompanied by unintended weight loss exceeding clinical targets. Patients who cannot tolerate the current dose despite dietary modifications and antiemetic use should discuss dose adjustment or extended titration schedules with their provider. New or worsening symptoms such as persistent heartburn, difficulty swallowing, or blood in vomit (bright red or coffee-ground appearance) or black, tarry stools require evaluation to exclude complications like gastrointestinal bleeding.
Treatment modifications may include temporarily reducing the dose, extending the interval between dose increases, or in some cases, discontinuing semaglutide if side effects remain intolerable despite comprehensive management strategies. Patients taking insulin or sulfonylureas should be particularly vigilant about hypoglycemia risk if nausea reduces food intake, and may need adjustment of these medications. For women of childbearing potential experiencing severe nausea, pregnancy testing may be warranted, as semaglutide is not recommended during pregnancy. Healthcare providers can assess the overall benefit-risk profile and determine the most appropriate course of action based on individual patient circumstances, therapeutic goals, and tolerance patterns.
Nausea is typically most pronounced during the first few weeks of treatment or following dose increases, with many patients experiencing improvement within 8 weeks as their bodies adapt. However, adaptation may take longer during Wegovy's 16-week titration period, and individual tolerance varies considerably.
Yes, options include vitamin B6 at 10-25 mg three times daily, ginger supplements at 250 mg four times daily, or antihistamines like meclizine. However, you should always consult your healthcare provider before adding any medications or supplements to ensure safety and appropriateness for your specific situation.
Seek immediate medical attention for severe, persistent vomiting preventing fluid intake, severe abdominal pain, signs of dehydration, or symptoms suggesting pancreatitis or gallbladder disease. Schedule a consultation if nausea persists beyond 8-12 weeks, significantly impacts quality of life, or prevents adequate nutritional intake despite management strategies.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.