LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) are incretin hormones secreted by the small intestine that regulate blood glucose and metabolism. These naturally occurring peptides enhance insulin secretion in a glucose-dependent manner, reducing hypoglycemia risk. Understanding GIP and GLP-1 has revolutionized diabetes and obesity treatment, leading to FDA-approved medications that mimic their actions. GLP-1 receptor agonists and the dual GIP/GLP-1 receptor agonist tirzepatide represent major therapeutic advances, offering improved glycemic control, cardiovascular benefits, and significant weight reduction for appropriate patients.
Quick Answer: GIP and GLP-1 are incretin hormones produced in the small intestine that enhance glucose-dependent insulin secretion and regulate metabolism.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) are incretin hormones secreted by specialized cells in the small intestine in response to nutrient intake. These endogenous peptides play critical roles in glucose homeostasis and metabolic regulation. GIP is primarily produced by K cells in the proximal small intestine, while GLP-1 is secreted by L cells predominantly in the distal ileum and colon.
Both hormones enhance insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning they stimulate insulin release only when blood glucose levels are elevated. This physiologic mechanism reduces the risk of hypoglycemia compared to insulin secretagogues that act independently of glucose concentration. GLP-1 also suppresses glucagon secretion from pancreatic alpha cells, slows gastric emptying, and promotes satiety through central nervous system pathways. GIP has additional effects on adipose tissue metabolism and may influence bone formation.
The incretin effect—the phenomenon whereby oral glucose intake produces a greater insulin response than intravenous glucose administration—is largely mediated by GIP and GLP-1. In individuals with type 2 diabetes mellitus, the incretin effect is diminished, with impaired beta-cell responsiveness to GIP being a dominant defect, while GLP-1 secretion may be modestly reduced in some patients. Both hormones are rapidly degraded by the enzyme dipeptidyl peptidase-4 (DPP-4), resulting in half-lives of approximately 5-7 minutes for GIP and 1-2 minutes for native GLP-1.
Understanding these hormones has led to the development of therapeutic agents that either mimic their actions (receptor agonists) or prevent their degradation (DPP-4 inhibitors), representing major advances in diabetes pharmacotherapy and, more recently, obesity management.
Medications targeting the GIP and GLP-1 pathways are FDA-approved primarily for type 2 diabetes mellitus and chronic weight management in adults with obesity or overweight with at least one weight-related comorbidity. The American Diabetes Association (ADA) Standards of Care recommend GLP-1 receptor agonists with proven cardiovascular benefit for patients with type 2 diabetes who have established atherosclerotic cardiovascular disease. For heart failure or chronic kidney disease progression, SGLT2 inhibitors are prioritized, with GLP-1 receptor agonists as alternatives when SGLT2 inhibitors are not appropriate.
For diabetes management, these medications improve glycemic control by enhancing glucose-dependent insulin secretion, suppressing inappropriate glucagon release, and slowing gastric emptying. Typical A1C reductions range from 0.8% to 2.0%, depending on the specific agent and baseline values. The glucose-dependent mechanism substantially reduces hypoglycemia risk compared to sulfonylureas or insulin, making these agents particularly suitable for older adults or those at high hypoglycemia risk.
In obesity treatment, GLP-1 receptor agonists approved for weight management produce clinically meaningful weight loss through multiple mechanisms: reduced appetite and caloric intake via central satiety pathways, delayed gastric emptying, and possible effects on energy expenditure. Clinical trials have demonstrated mean weight reductions of approximately 5-8% with liraglutide and 10-15% with semaglutide 2.4 mg. The dual GIP/GLP-1 receptor agonist tirzepatide has shown superior weight loss efficacy (15-22%) compared to selective GLP-1 agonists in head-to-head trials.
Cardiovascular risk reduction is established for specific GLP-1 receptor agonists in type 2 diabetes, and semaglutide 2.4 mg (Wegovy) has an FDA-approved indication for major adverse cardiovascular event risk reduction. Emerging evidence suggests potential benefits in nonalcoholic steatohepatitis (NASH) and obstructive sleep apnea, though these remain investigational indications. Patient selection should consider contraindications including personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2 for specific agents (liraglutide, semaglutide, dulaglutide, tirzepatide), as these carry a boxed warning based on rodent thyroid C-cell tumor findings.
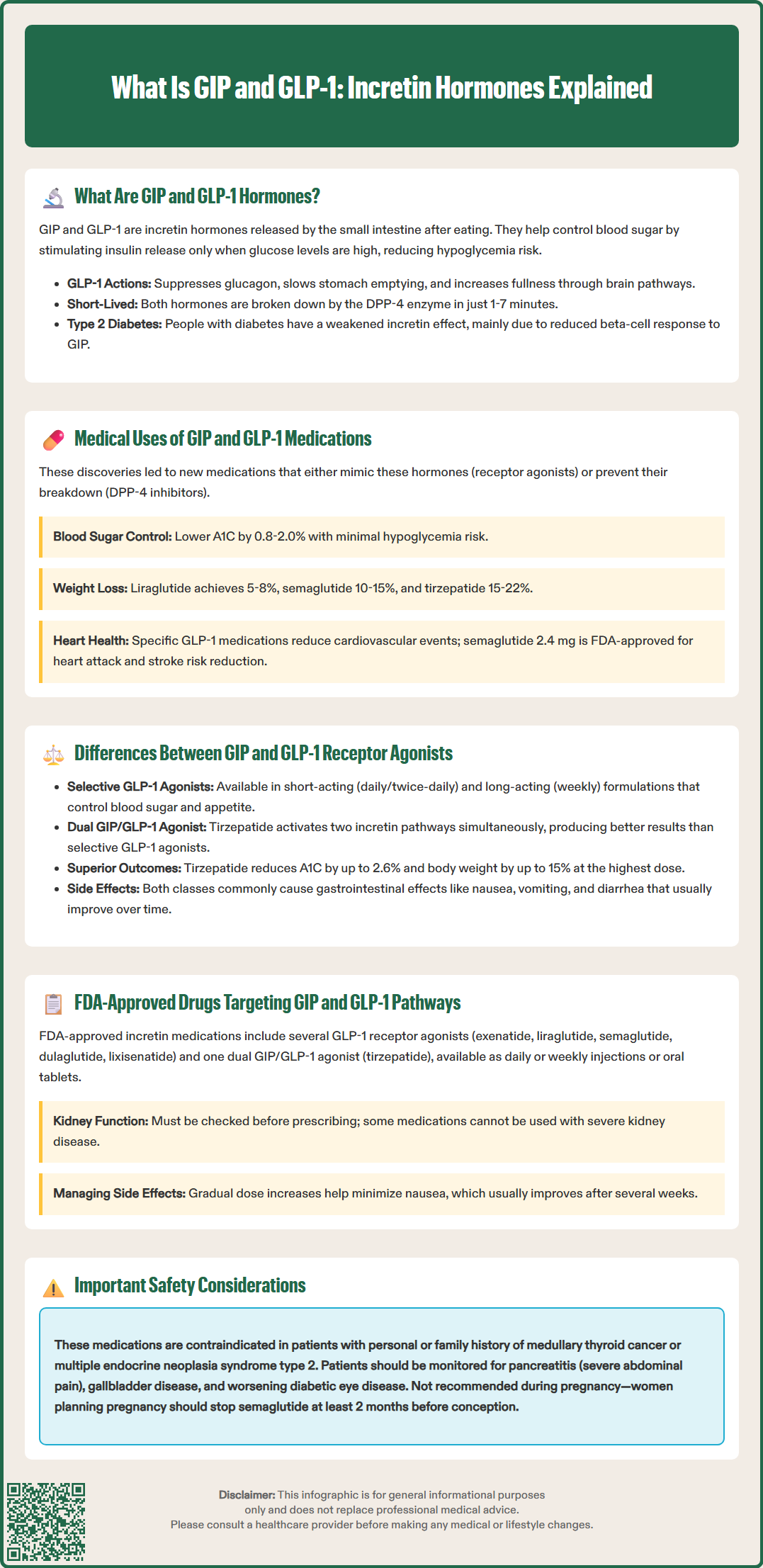
Selective GLP-1 receptor agonists have been the cornerstone of incretin-based therapy since exenatide's approval in 2005. These medications bind exclusively to GLP-1 receptors, mimicking the hormone's effects on insulin secretion, glucagon suppression, gastric emptying, and appetite regulation. Available formulations include short-acting agents requiring daily or twice-daily administration (exenatide, lixisenatide) and long-acting preparations given weekly (semaglutide, dulaglutide, exenatide extended-release). The extended half-life of long-acting formulations results from structural modifications that resist DPP-4 degradation and enhance albumin binding.
The dual GIP/GLP-1 receptor agonist tirzepatide represents a novel therapeutic approach, simultaneously activating both incretin pathways. While GLP-1 receptor activation provides well-established metabolic benefits, the contribution of GIP receptor agonism remains an area of active investigation. Preclinical studies suggest GIP may enhance insulin secretion, improve beta-cell function, and influence adipose tissue metabolism differently than GLP-1. Some preclinical evidence indicates GIP receptor activation may affect adipose tissue metabolism and ectopic lipid deposition, though these mechanisms require further confirmation in humans.
Clinical trial data demonstrate that tirzepatide produces superior A1C reduction and weight loss compared to selective GLP-1 agonists, though the precise mechanisms underlying this enhanced efficacy are not fully elucidated. The SURPASS clinical trial program showed tirzepatide reduced A1C by up to 2.6% and body weight by up to 15% at the highest dose, exceeding comparator GLP-1 agonists.
Adverse effect profiles are generally similar between drug classes, with gastrointestinal symptoms (nausea, vomiting, diarrhea) being most common. These effects are typically dose-dependent and diminish with continued therapy. Gradual dose titration is essential to minimize gastrointestinal intolerance. Both drug classes carry warnings regarding pancreatitis risk, though causality remains uncertain, and certain agents carry thyroid C-cell tumor risk warnings based on animal data.
The FDA has approved multiple medications targeting incretin pathways, categorized into GLP-1 receptor agonists and the dual GIP/GLP-1 receptor agonist. Current GLP-1 receptor agonists include:
Exenatide (Byetta): Twice-daily injection for type 2 diabetes
Exenatide extended-release (Bydureon BCise): Weekly injection for type 2 diabetes
Liraglutide (Victoza): Daily injection for type 2 diabetes; (Saxenda): daily injection for chronic weight management
Dulaglutide (Trulicity): Weekly injection for type 2 diabetes
Semaglutide (Ozempic): Weekly injection for type 2 diabetes; (Wegovy): weekly injection for chronic weight management; (Rybelsus): oral daily tablet for type 2 diabetes
Lixisenatide (Adlyxin): Daily injection for type 2 diabetes
The sole FDA-approved dual GIP/GLP-1 receptor agonist is tirzepatide (Mounjaro for type 2 diabetes; Zepbound for chronic weight management). This medication is administered as a weekly subcutaneous injection with doses ranging from 2.5 mg to 15 mg, titrated based on efficacy and tolerability.
Prescribing considerations include renal function assessment, as specific recommendations vary by agent. Exenatide and lixisenatide are not recommended in severe renal impairment or end-stage renal disease, while liraglutide, semaglutide, and dulaglutide typically require no dose adjustment. These medications are not indicated for type 1 diabetes and should not be coadministered with DPP-4 inhibitors.
Patients should be counseled on proper injection technique, storage requirements, and the importance of gradual dose escalation. Common adverse effects—particularly nausea—typically improve after several weeks but may necessitate dose reduction or discontinuation in some individuals. These medications should be used with caution in patients with severe gastrointestinal disease, including gastroparesis.
Clinicians should monitor for signs of pancreatitis (severe abdominal pain), gallbladder disease, and diabetic retinopathy worsening in susceptible patients. For weight management indications (Wegovy, Saxenda, Zepbound), use during pregnancy is contraindicated. For diabetes indications, these medications are generally not recommended during pregnancy and should be discontinued when pregnancy is recognized. Women of childbearing potential should be advised that semaglutide should be discontinued at least 2 months before planned conception. Tirzepatide may reduce the exposure of oral contraceptives; non-oral or backup contraception is advised for 4 weeks after initiation and each dose escalation.
GIP is produced by K cells in the proximal small intestine and primarily enhances insulin secretion with additional effects on adipose tissue and bone metabolism. GLP-1 is secreted by L cells in the distal ileum and colon and not only stimulates insulin but also suppresses glucagon, slows gastric emptying, and promotes satiety.
Medications targeting GIP and GLP-1 pathways improve glycemic control by enhancing glucose-dependent insulin secretion, suppressing inappropriate glucagon release, and slowing gastric emptying. Their glucose-dependent mechanism substantially reduces hypoglycemia risk compared to sulfonylureas or insulin.
Tirzepatide is the first FDA-approved dual GIP/GLP-1 receptor agonist that simultaneously activates both incretin pathways. Clinical trials demonstrate superior A1C reduction and weight loss compared to selective GLP-1 receptor agonists, though the precise mechanisms underlying this enhanced efficacy are still being investigated.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.