LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Many patients taking metformin for type 2 diabetes wonder whether this widely prescribed medication could be causing their hair loss. Metformin, a first-line biguanide antihyperglycemic agent approved by the FDA, is generally well-tolerated with primarily gastrointestinal side effects. However, concerns about hair thinning prompt important questions about this medication's safety profile. Understanding the relationship between metformin and hair loss requires examining current medical evidence, considering indirect mechanisms like vitamin B12 deficiency, and recognizing alternative causes. This article explores what research reveals about metformin's potential effects on hair health and provides guidance for patients experiencing hair loss while taking this essential diabetes medication.
Quick Answer: Metformin does not directly cause hair loss according to current medical evidence, though it may indirectly contribute through vitamin B12 deficiency with long-term use.
Metformin is a first-line oral medication for type 2 diabetes mellitus, prescribed to millions of patients in the United States. As a biguanide antihyperglycemic agent, metformin works primarily by decreasing hepatic glucose production, reducing intestinal glucose absorption, and improving insulin sensitivity in peripheral tissues. The FDA-approved medication has been in clinical use for decades and is generally well-tolerated, making it a cornerstone of diabetes management according to American Diabetes Association (ADA) guidelines.
The most frequently reported adverse effects of metformin are gastrointestinal in nature. Patients commonly experience nausea, diarrhea, abdominal discomfort, and metallic taste, particularly during initial treatment or dose escalation. These symptoms typically resolve within several weeks as the body adjusts to the medication. Starting with a low dose and taking metformin with meals can significantly reduce gastrointestinal side effects. Extended-release formulations may also improve tolerability.
Less common but clinically significant adverse effects include vitamin B12 deficiency, which may develop with long-term use due to impaired absorption in the terminal ileum. This deficiency can manifest as peripheral neuropathy, anemia, or cognitive changes. The ADA recommends periodic B12 assessment, especially in patients with anemia or neuropathy. Lactic acidosis, though rare (occurring in fewer than 10 cases per 100,000 patient-years), represents the most serious potential complication, particularly in patients with renal impairment (eGFR <30 mL/min/1.73 m²), hepatic dysfunction, alcohol misuse, advanced age (≥65), or conditions causing tissue hypoxia.
Other documented side effects include reduced appetite, weight loss (often considered beneficial in type 2 diabetes), and occasional reports of headache or dizziness. Metformin is contraindicated when eGFR is below 30 mL/min/1.73 m², and caution is advised when initiating at eGFR 30-44 mL/min/1.73 m². Temporary discontinuation is recommended with iodinated contrast procedures in patients with certain risk factors. Understanding these established adverse effects provides important context when evaluating less commonly reported symptoms, such as hair loss, in patients taking metformin.
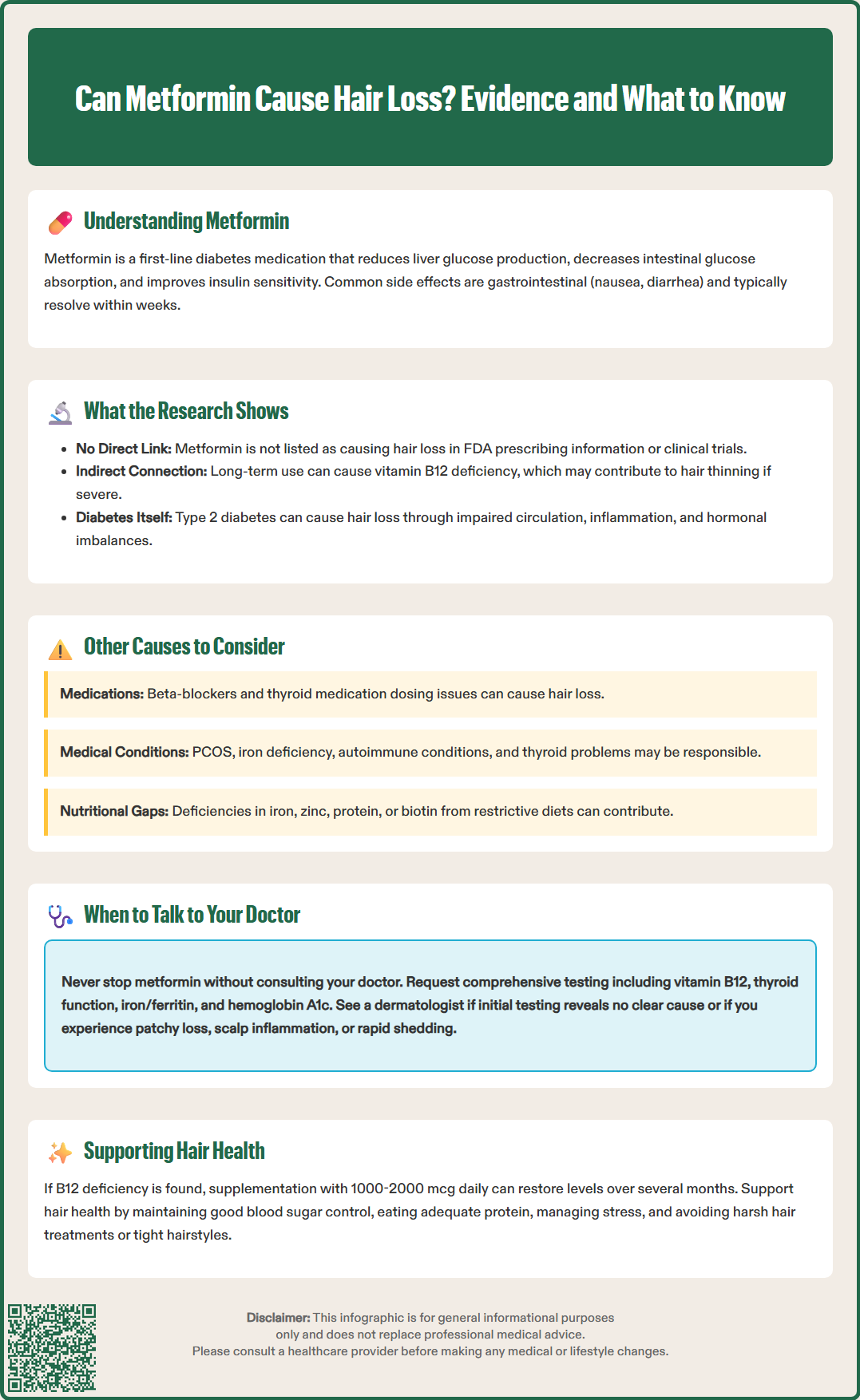
There is no established causal link between metformin and hair loss based on current medical evidence. Hair loss (alopecia) is not listed as a recognized adverse effect in the FDA-approved prescribing information for metformin, nor is it documented in major clinical trials or systematic reviews of metformin safety profiles. When patients report hair loss while taking metformin, the association is typically coincidental rather than causative.
The medical literature contains only isolated case reports suggesting a possible temporal relationship between metformin use and hair thinning, but these reports lack the scientific rigor to establish causation. No controlled clinical trials have demonstrated that metformin directly causes hair loss. While some research suggests metformin may indirectly affect hair follicles through its effects on insulin resistance, particularly in conditions like polycystic ovary syndrome (PCOS), there is insufficient evidence to support direct beneficial effects on scalp hair regrowth.
However, an indirect mechanism deserves consideration: metformin-induced vitamin B12 deficiency. Prolonged metformin therapy can impair vitamin B12 absorption, and severe B12 deficiency may contribute to hair changes, including thinning or loss. This represents a secondary effect rather than a direct drug-induced alopecia. Data from the Diabetes Prevention Program Outcomes Study indicate that patients on long-term metformin have significantly lower B12 levels compared to those not taking the medication. When B12 levels are borderline but symptoms are present, additional testing such as methylmalonic acid may help confirm deficiency.
It's important to recognize that type 2 diabetes itself can affect hair health. Poorly controlled diabetes may lead to hair thinning through multiple mechanisms, including impaired circulation, chronic inflammation, and hormonal imbalances. Additionally, the stress of managing a chronic condition, dietary changes, and weight fluctuations associated with diabetes treatment may all influence hair growth cycles. When evaluating hair loss in a patient taking metformin, clinicians should consider these alternative explanations before attributing the symptom to the medication. Suspected adverse drug reactions can be reported to the FDA MedWatch program.
Numerous medications commonly prescribed to patients with diabetes or related conditions can cause hair loss through various mechanisms. Antihypertensive medications, particularly beta-blockers (such as metoprolol and atenolol), have documented associations with telogen effluvium, a condition where hair follicles prematurely enter the resting phase. ACE inhibitors and statins have been linked to hair loss in rare case reports, though a causal relationship is not firmly established for most patients taking these medications.
Thyroid medications require careful consideration, as both hypothyroidism and hyperthyroidism can cause significant hair loss. Patients with type 2 diabetes have higher rates of thyroid dysfunction, and improper thyroid hormone replacement dosing may contribute to alopecia. Anticoagulants, including warfarin and heparin, are recognized causes of drug-induced hair loss, particularly relevant for diabetic patients with cardiovascular disease.
Several medical conditions commonly coexist with diabetes and independently cause hair loss. Polycystic ovary syndrome (PCOS), frequently treated with metformin, causes androgenic alopecia through elevated androgen levels. Iron deficiency anemia may contribute to diffuse hair thinning and should be evaluated based on risk factors and symptoms. Autoimmune conditions, including alopecia areata and thyroid disorders, occur at higher rates in patients with diabetes, particularly type 1 diabetes.
Nutritional deficiencies beyond vitamin B12 warrant investigation. Iron, zinc, protein, and occasionally biotin deficiencies can contribute to hair loss. Patients following restrictive diets for diabetes management may inadvertently develop these deficiencies. It's important to note that high-dose biotin supplements can interfere with many laboratory tests, including thyroid and cardiac markers, and should be avoided before blood testing. Chronic stress, whether from diabetes management or other life circumstances, can trigger telogen effluvium. Hormonal changes, particularly in perimenopausal women with diabetes, frequently cause hair thinning through altered estrogen and androgen ratios. A comprehensive evaluation should consider these multiple potential contributors before concluding that any single medication is responsible for hair loss.
If you notice hair loss while taking metformin, do not discontinue the medication without consulting your healthcare provider . Metformin plays a crucial role in diabetes management, and stopping it abruptly may lead to dangerous elevations in blood glucose levels. Instead, schedule an appointment with your physician to discuss your concerns and undergo appropriate evaluation.
Your healthcare provider should conduct a thorough assessment to identify the underlying cause. This evaluation typically includes a detailed medication review, examining all prescription and over-the-counter drugs that might contribute to hair loss. Laboratory testing is essential and should include vitamin B12 levels (particularly important for long-term metformin users), complete blood count to assess for anemia, thyroid function tests (TSH and free T4), iron studies including ferritin, and potentially zinc levels. For women with signs of hyperandrogenism or suspected PCOS, androgen testing (total/free testosterone, DHEAS) may be appropriate. Hemoglobin A1c testing helps determine whether poorly controlled diabetes might be contributing to the problem.
If vitamin B12 deficiency is identified, supplementation with oral B12 (1000-2000 mcg daily) or, in cases of severe deficiency or malabsorption, intramuscular B12 injections can effectively restore levels. The ADA recommends periodic B12 assessment in metformin users, especially those with anemia or neuropathy. Correcting B12 deficiency may improve hair health over several months, though hair regrowth is typically gradual. If taking biotin supplements, discontinue them at least 72 hours before laboratory testing to avoid interference with test results.
Referral to a dermatologist is appropriate if initial evaluation doesn't reveal an obvious cause or if hair loss is severe, patchy, or accompanied by scalp changes. Urgent referral is warranted for signs of scarring alopecia, rapid diffuse hair loss, painful or inflamed scalp, or hair loss with systemic symptoms. Dermatologists can perform specialized assessments, including scalp examination, hair pull tests, and occasionally scalp biopsy to diagnose specific types of alopecia. They can also provide targeted treatments such as topical minoxidil or other therapies appropriate for the diagnosed condition.
In the meantime, focus on optimizing overall health: maintain good glycemic control, ensure adequate nutrition with sufficient protein intake, manage stress through appropriate techniques, and avoid harsh hair treatments or tight hairstyles that may worsen hair loss. Most importantly, maintain open communication with your healthcare team to ensure both your diabetes management and overall well-being remain priorities.
No, hair loss is not a recognized or common side effect of metformin. The most frequent adverse effects are gastrointestinal, including nausea and diarrhea, which typically resolve within weeks of starting treatment.
Do not discontinue metformin without consulting your healthcare provider, as stopping it abruptly may cause dangerous blood glucose elevations. Schedule an appointment to discuss your concerns and undergo appropriate evaluation to identify the underlying cause.
Essential laboratory testing includes vitamin B12 levels, complete blood count, thyroid function tests, iron studies including ferritin, and hemoglobin A1c. For women with signs of hormonal imbalance, androgen testing may also be appropriate.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.