LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
GLP-1 balance describes the optimal production and function of glucagon-like peptide-1, a hormone that regulates blood sugar and appetite. While not a formal medical diagnosis, this concept has gained attention with the rise of GLP-1 medications for diabetes and weight management. Understanding how GLP-1 works in your body can help you make informed decisions about metabolic health. This article explains what GLP-1 balance means, signs of potential dysfunction, natural support strategies, and how this hormone system influences glucose control and satiety.
Quick Answer: GLP-1 balance refers to optimal production and activity of glucagon-like peptide-1, a hormone that regulates blood sugar and appetite, though it is not a recognized diagnostic entity in clinical practice.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
GLP-1 balance refers to the optimal production, secretion, and activity of glucagon-like peptide-1 (GLP-1), an incretin hormone produced primarily by enteroendocrine L-cells in the distal small intestine and colon. It's important to note that "GLP-1 balance" is a conceptual description rather than a recognized diagnostic entity or measurable clinical target in standard practice.
In medical terms, a balanced GLP-1 system means the body produces adequate amounts of this hormone in response to nutrient intake, and that the hormone functions effectively at its target receptors throughout the body.
GLP-1 has a remarkably short half-life of approximately 1.5 to 2 minutes in circulation due to rapid degradation by the enzyme dipeptidyl peptidase-4 (DPP-4). Despite this brief duration, GLP-1 exerts significant physiological effects on glucose homeostasis, appetite regulation, and gastric emptying. When GLP-1 function is optimal, the hormone appropriately stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner, suppresses inappropriate glucagon release from alpha cells, and signals satiety to the central nervous system.
Imbalanced GLP-1 function may manifest as either insufficient production or impaired receptor sensitivity, though there is no official clinical definition of "GLP-1 imbalance" as a distinct diagnostic entity. Research suggests that individuals with type 2 diabetes may have reduced GLP-1 secretion or diminished incretin effect compared to those without diabetes, though this finding is not universal across all studies. The concept of GLP-1 balance has gained clinical relevance with the development of GLP-1 receptor agonists (such as semaglutide and liraglutide) for glycemic control and, at specific FDA-approved doses, chronic weight management. DPP-4 inhibitors are also used therapeutically to enhance endogenous GLP-1 activity, but only for glycemic control, as they are weight-neutral. Per American Diabetes Association guidance, GLP-1 receptor agonists and DPP-4 inhibitors should not be used in combination.
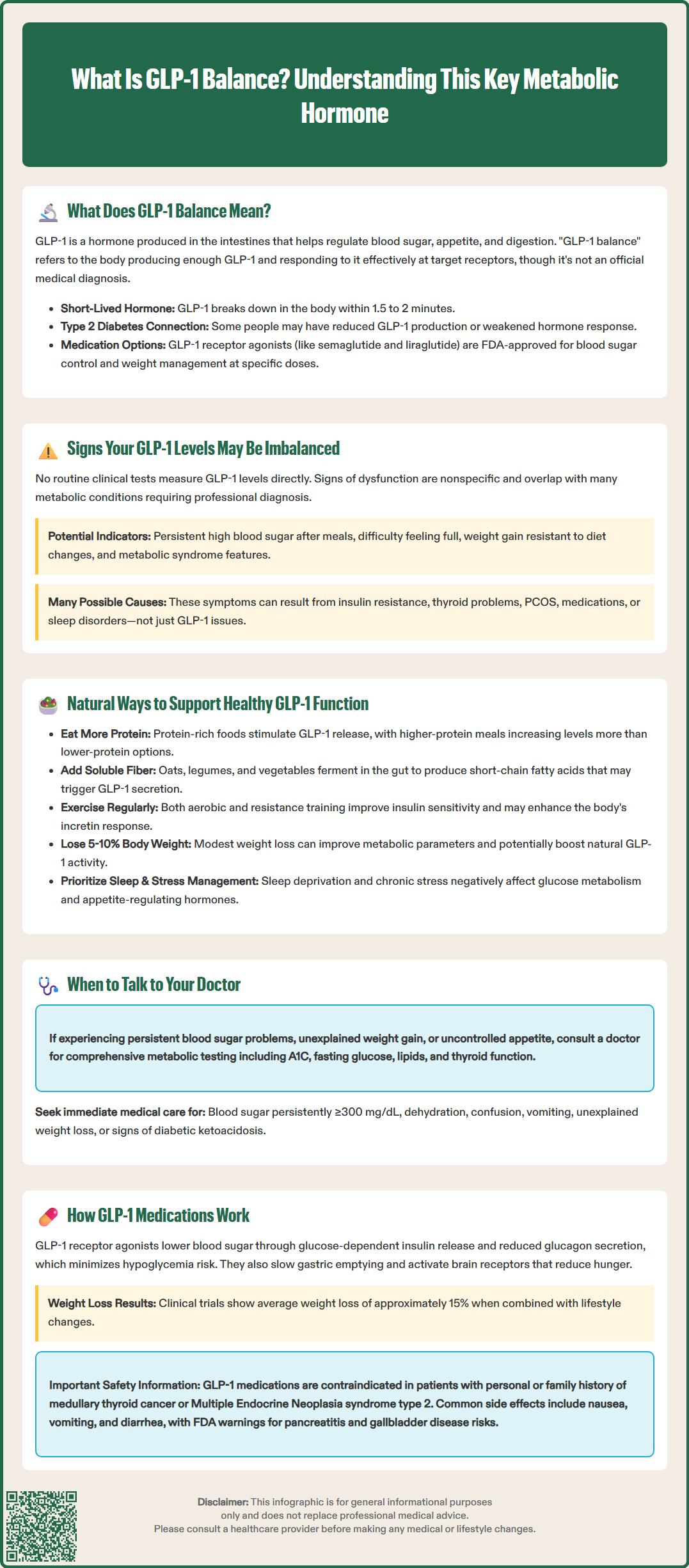
There are no specific clinical tests routinely used to measure GLP-1 levels in standard medical practice, and symptoms of potential GLP-1 dysfunction are nonspecific and overlap with many other metabolic conditions. However, certain clinical presentations may suggest suboptimal GLP-1 function, though these should never be self-diagnosed.
Metabolic indicators that may correlate with reduced GLP-1 activity include:
Persistent hyperglycemia despite dietary modifications, particularly elevated postprandial (after-meal) blood glucose levels
Difficulty achieving satiety after meals, leading to continued hunger and frequent snacking
Progressive weight gain that is resistant to conventional dietary interventions
Diagnosis of prediabetes or type 2 diabetes, conditions associated with impaired incretin response
Metabolic syndrome features, including central obesity, hypertension, and dyslipidemia
It is important to emphasize that these signs are not diagnostic of GLP-1 imbalance specifically, as they can result from numerous metabolic, endocrine, or lifestyle factors. Insulin resistance, thyroid dysfunction, polycystic ovary syndrome (PCOS), medication side effects, and sleep disorders can all produce similar clinical pictures.
If you experience persistent difficulties with blood sugar control, unexplained weight gain, or uncontrolled appetite despite appropriate lifestyle measures, consultation with a primary care physician or endocrinologist is warranted. Clinical evaluation should include comprehensive metabolic assessment with fasting glucose, hemoglobin A1C, lipid panel, and thyroid function tests.
According to American Diabetes Association guidelines, diabetes is diagnosed when A1C ≥6.5%, fasting plasma glucose ≥126 mg/dL, 2-hour plasma glucose ≥200 mg/dL during an oral glucose tolerance test, or random plasma glucose ≥200 mg/dL with classic symptoms. Prediabetes is defined as A1C 5.7–6.4%, fasting glucose 100–125 mg/dL, or 2-hour glucose 140–199 mg/dL.
Seek immediate medical attention if you experience: marked hyperglycemia (persistent glucose ≥300 mg/dL), dehydration, confusion, vomiting, unexplained weight loss, excessive urination, extreme thirst, or signs of diabetic ketoacidosis (abdominal pain, rapid breathing, fruity breath odor).
While pharmaceutical GLP-1 receptor agonists provide potent therapeutic effects, several evidence-based lifestyle and dietary strategies may support endogenous GLP-1 secretion. These approaches should be viewed as complementary to, not replacements for, medical treatment when indicated, and may not produce significant GLP-1-mediated clinical effects on their own.
Dietary modifications that may influence GLP-1 secretion include:
Protein-rich foods: Dietary protein can stimulate GLP-1 release. Some studies suggest that meals containing adequate protein may increase postprandial GLP-1 levels compared to lower-protein meals, though specific gram targets vary by individual needs.
Fiber intake: Soluble fiber, particularly from sources like oats, legumes, and vegetables, undergoes fermentation by gut microbiota to produce short-chain fatty acids (SCFAs), which may stimulate L-cell GLP-1 secretion.
Dietary fat: Dietary fat can stimulate GLP-1 acutely; evidence for specific effects of omega-3 fatty acids or monounsaturated fats on GLP-1 secretion is limited and preliminary.
Fermented foods: Probiotics and fermented foods may support a healthy gut microbiome, which plays a role in metabolic health, though clinical evidence specifically linking these to enhanced GLP-1 production remains preliminary.
Lifestyle factors that support metabolic health and may influence GLP-1 function:
Regular physical activity: Exercise improves insulin sensitivity and may enhance incretin response, with both aerobic and resistance training showing benefits.
Weight management: Modest weight loss (5-10% of body weight) in individuals with overweight or obesity can improve metabolic parameters and potentially enhance endogenous GLP-1 activity.
Adequate sleep: Sleep deprivation impairs glucose metabolism and may affect appetite-regulating hormones, including GLP-1.
Stress management: Chronic stress and elevated cortisol levels can negatively impact metabolic health and appetite regulation.
These strategies align with the Dietary Guidelines for Americans 2020-2025 and should be implemented as part of comprehensive lifestyle modification under medical guidance, particularly for individuals with diabetes or other metabolic conditions requiring ongoing monitoring.
GLP-1 exerts its metabolic effects through activation of GLP-1 receptors (GLP-1R) distributed throughout multiple organ systems, including the pancreas, brain, gastrointestinal tract, and cardiovascular system. Understanding this mechanism clarifies why GLP-1-based therapies have become central to modern diabetes and obesity management.
Glucose regulation mechanisms:
GLP-1's primary glucoregulatory effect occurs through glucose-dependent insulin secretion from pancreatic beta cells. When blood glucose levels are elevated, GLP-1 binding to beta-cell receptors triggers intracellular signaling cascades that enhance insulin synthesis and release. Critically, this effect is glucose-dependent, meaning insulin secretion diminishes as blood glucose normalizes, substantially reducing hypoglycemia risk compared to sulfonylureas or exogenous insulin. Simultaneously, GLP-1 suppresses glucagon secretion from pancreatic alpha cells, reducing hepatic glucose production when it is not needed. This dual action—enhancing insulin while suppressing glucagon—creates a powerful glucose-lowering effect during hyperglycemic states.
Additionally, GLP-1 slows gastric emptying, which moderates the rate at which nutrients enter the small intestine and are absorbed into the bloodstream. This effect attenuates postprandial glucose excursions, though tachyphylaxis (reduced response over time) to this particular effect may occur with chronic GLP-1 receptor agonist therapy.
Appetite regulation mechanisms:
GLP-1 receptors in the hypothalamus and brainstem mediate satiety signaling. GLP-1 crosses the blood-brain barrier in limited amounts, but more importantly, it activates vagal afferent neurons that communicate with central appetite centers. This signaling reduces hunger, increases satiety, and decreases food intake. Clinical trials with GLP-1 receptor agonists consistently demonstrate significant weight loss, with higher doses (such as semaglutide 2.4 mg weekly) producing approximately 15% average weight loss in adults without diabetes in clinical trials (somewhat less in type 2 diabetes) when combined with lifestyle modification.
Safety considerations:
GLP-1 receptor agonists are contraindicated in patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2. FDA warnings include risks of pancreatitis and gallbladder disease. While the risk of hypoglycemia is low with GLP-1 receptor agonists alone, this risk increases when combined with insulin or sulfonylureas. Common side effects include nausea, vomiting, and diarrhea, which are typically transient.
No, there are no routine clinical tests to measure GLP-1 levels in standard medical practice, and no home testing options exist. Evaluation of metabolic health requires comprehensive laboratory assessment including fasting glucose, hemoglobin A1C, and lipid panels performed by healthcare providers.
GLP-1 receptor agonists directly activate GLP-1 receptors and are FDA-approved for both glycemic control and weight management at specific doses, while DPP-4 inhibitors prevent breakdown of endogenous GLP-1, are used only for glycemic control, and are weight-neutral. Per American Diabetes Association guidance, these medication classes should not be combined.
GLP-1 receptor agonists are contraindicated in patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2. FDA warnings also include risks of pancreatitis and gallbladder disease, requiring careful patient selection and monitoring.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.