LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Metformin is the most commonly prescribed medication for type 2 diabetes, yet many patients wonder: does metformin use the pancreas to lower blood sugar? Understanding how this medication works is essential for anyone taking it or considering diabetes treatment options. Unlike some diabetes drugs that force the pancreas to produce more insulin, metformin operates through different mechanisms that primarily target the liver and muscle tissues. This pancreas-independent action makes metformin uniquely safe and effective for long-term diabetes management, with minimal risk of hypoglycemia when used alone.
Quick Answer: Metformin does not use or stimulate the pancreas to produce insulin; it works primarily by reducing glucose production in the liver and improving insulin sensitivity in muscle tissue.
Metformin is a first-line medication for type 2 diabetes that works primarily through mechanisms independent of the pancreas. Unlike medications that stimulate insulin release, metformin exerts its glucose-lowering effects mainly in the liver and peripheral tissues. The drug belongs to the biguanide class and has been used safely for decades in diabetes management.
The primary mechanism of metformin involves reducing hepatic glucose production. The liver normally releases glucose into the bloodstream, particularly during fasting states. Metformin suppresses this process by inhibiting gluconeogenesis—the metabolic pathway that creates new glucose molecules. This action likely occurs through multiple mechanisms, including inhibition of mitochondrial complex I, with downstream effects that may involve AMP-activated protein kinase (AMPK) activation, a cellular energy sensor that influences glucose and lipid metabolism.
Additionally, metformin enhances insulin sensitivity in peripheral tissues, particularly skeletal muscle. This improvement allows cells to take up and utilize glucose more effectively from the bloodstream without requiring additional insulin production. The medication also appears to reduce glucose absorption in the intestines and may influence gut hormones like GLP-1, contributing to its overall glucose-lowering effect.
Importantly, metformin does not directly stimulate the pancreas to produce more insulin. This pancreas-independent mechanism explains why metformin rarely causes hypoglycemia when used alone. The medication works with the body's existing insulin levels rather than forcing the pancreas to increase insulin secretion, making it fundamentally different from sulfonylureas or meglitinides that directly target pancreatic beta cells.
Metformin does not increase insulin production by the pancreas, which distinguishes it from several other diabetes medications. This characteristic is clinically significant because it means metformin does not place additional demand on pancreatic beta cells—the specialized cells responsible for insulin secretion. For patients with type 2 diabetes, whose beta cells may already be stressed or declining in function, this pancreas-sparing effect is advantageous.
Some research suggests that metformin may have protective effects on pancreatic beta cells, though this remains an area of ongoing investigation. Observational and preclinical studies indicate the medication might help preserve beta cell function over time by reducing glucotoxicity—the harmful effects of chronically elevated blood glucose on insulin-producing cells. By lowering blood glucose through hepatic and peripheral mechanisms, metformin may indirectly reduce the workload on the pancreas, though this is not an FDA-approved indication.
The FDA-approved prescribing information for metformin confirms that the drug improves glucose control without stimulating insulin secretion in healthy individuals. When metformin lowers blood glucose in people with type 2 diabetes, any associated changes in insulin levels are typically modest and represent improved insulin sensitivity rather than increased pancreatic output.
This mechanism explains why metformin monotherapy carries minimal risk of hypoglycemia. Since the pancreas is not being stimulated to release more insulin than physiologically appropriate, blood glucose rarely drops to dangerously low levels. However, when metformin is combined with insulin or insulin secretagogues (medications that do stimulate the pancreas), hypoglycemia risk increases, and dose adjustments of these other medications may be necessary. It's important to note that metformin is not appropriate for treating type 1 diabetes or diabetic ketoacidosis when used alone.
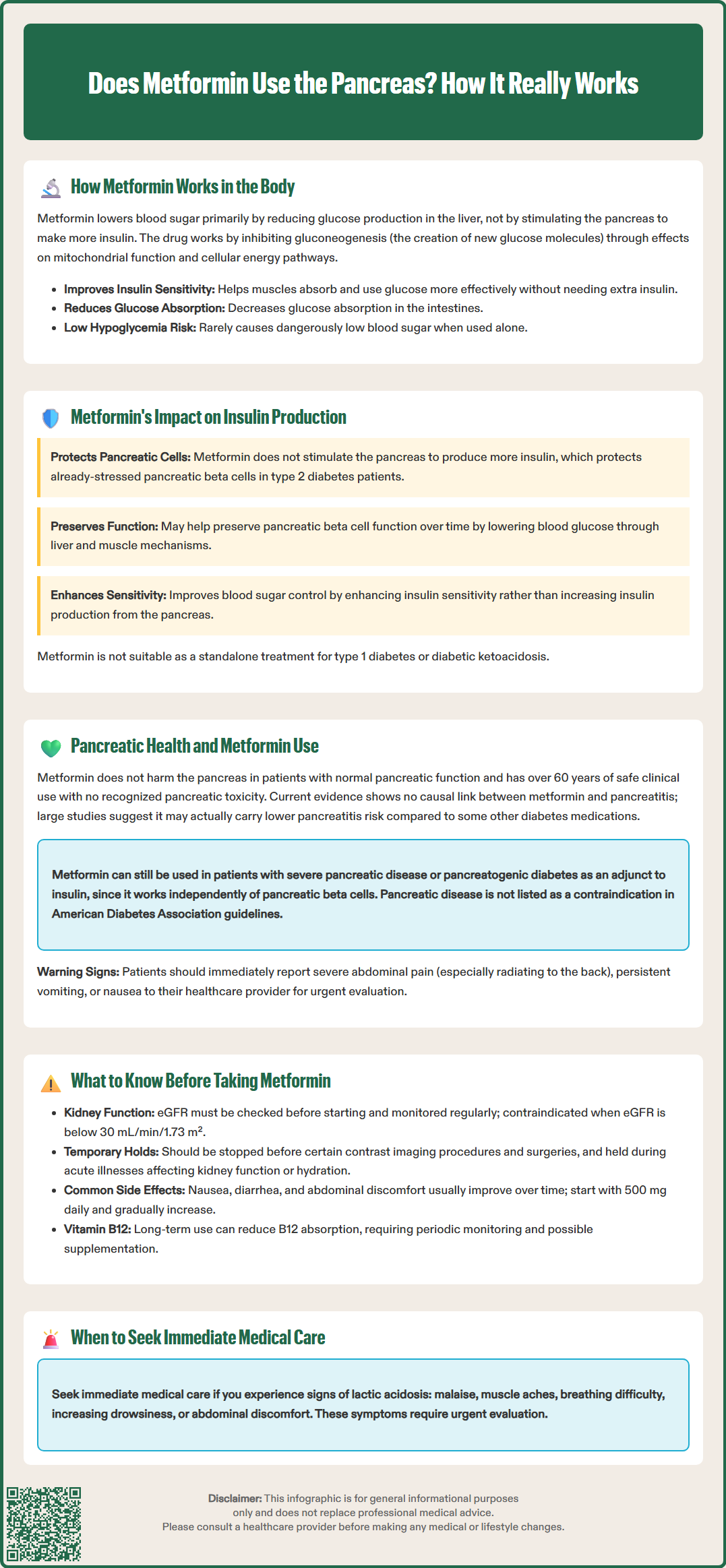
There is no established evidence that metformin causes harm to the pancreas in patients with normal pancreatic function. The medication has an extensive safety record spanning over six decades of clinical use, and pancreatic toxicity is not recognized as an adverse effect of metformin therapy. This safety profile makes metformin suitable for long-term use in diabetes management.
Concerns occasionally arise regarding metformin and pancreatitis, but current evidence does not support a causal relationship. Large observational studies and meta-analyses have not demonstrated an increased risk of acute pancreatitis with metformin use. Some observational research suggests metformin may be associated with a lower risk of pancreatitis compared to certain other diabetes medications, though this relationship is not definitively established and requires further investigation.
Patients with pre-existing pancreatic disease require individualized assessment. While metformin itself does not damage the pancreas, conditions such as chronic pancreatitis or pancreatic insufficiency may affect diabetes management strategies. In cases of severe pancreatic disease where insulin production is significantly impaired (such as pancreatogenic diabetes), metformin may still be used as an adjunct to insulin therapy, as its mechanisms do not depend on functional beta cells. Patients with pancreatogenic diabetes may benefit from endocrinology referral for specialized management.
The American Diabetes Association guidelines do not list pancreatic disease as a contraindication to metformin use, though clinical judgment is essential. Healthcare providers should evaluate each patient's complete medical history, including any history of pancreatitis, pancreatic cancer, or pancreatic surgery. Patients should report any new onset of severe abdominal pain (especially epigastric pain radiating to the back), persistent vomiting, or nausea to their healthcare provider immediately, as these symptoms warrant urgent evaluation regardless of medication use.
Before starting metformin, patients should undergo assessment of kidney function, as the medication is primarily eliminated through the kidneys. The FDA recommends checking estimated glomerular filtration rate (eGFR) before initiation and periodically thereafter. Metformin is contraindicated in severe renal impairment (eGFR below 30 mL/min/1.73 m²). For patients with eGFR between 30-45 mL/min/1.73 m², initiation is generally not recommended, though continuation with dose reduction and close monitoring may be appropriate in some cases.
Patients should inform their healthcare provider about all medical conditions, particularly:
Kidney disease or reduced kidney function
Liver disease, as hepatic impairment increases lactic acidosis risk
Heart failure, especially unstable or acute heart failure (stable, treated heart failure may allow metformin use with monitoring)
History of lactic acidosis
Planned surgical procedures or imaging studies with iodinated contrast
For iodinated contrast procedures, current guidelines recommend holding metformin for patients with eGFR <30 mL/min/1.73 m², acute kidney injury, or when receiving intra-arterial contrast. For intravenous contrast with eGFR ≥30 and no acute kidney injury, metformin generally does not need to be held. If metformin is held, kidney function should be rechecked approximately 48 hours post-procedure before resuming.
For surgical procedures, metformin should be temporarily discontinued when oral intake is restricted and restarted when renal function and oral intake are stable. Similarly, the medication should be held during acute illnesses that may affect kidney function or hydration status.
Typical dosing starts at 500 mg once daily with food, gradually increasing by 500 mg weekly as tolerated to a target of 1500-2000 mg/day. Common side effects include gastrointestinal symptoms such as nausea, diarrhea, and abdominal discomfort, which typically improve with continued use or dose adjustment. Extended-release formulations may be better tolerated in some patients.
Patients should be aware of lactic acidosis warning signs (malaise, muscle aches, breathing difficulty, increasing drowsiness, abdominal discomfort) and seek immediate medical attention if these develop. Long-term metformin use may affect vitamin B12 absorption, and periodic monitoring of B12 levels is recommended, particularly in patients with anemia or peripheral neuropathy. Supplementation may be necessary if deficiency develops. Patients should maintain regular follow-up appointments to monitor diabetes control, kidney function, and overall medication tolerance, ensuring safe and effective long-term therapy.
No, metformin does not damage the pancreas and has an extensive safety record spanning over six decades. Current evidence does not support an increased risk of pancreatitis with metformin use.
Metformin rarely causes hypoglycemia because it does not stimulate the pancreas to produce more insulin. It works by reducing glucose production in the liver and improving how the body uses existing insulin, rather than forcing additional insulin release.
Metformin may still be appropriate for patients with pancreatic disease, as it does not depend on pancreatic beta cell function. However, individualized assessment by a healthcare provider is essential, and patients with pancreatogenic diabetes may benefit from endocrinology referral.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.