LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide (Mounjaro for type 2 diabetes, Zepbound for weight management) is a dual GIP/GLP-1 receptor agonist that produces significant weight loss through appetite suppression and metabolic effects. When discontinued, patients commonly experience weight regain as the medication's effects fade—clinical trials show approximately 14% weight regain over one year after stopping treatment. Successfully weaning off tirzepatide without gaining weight requires strategic planning, including potential dose tapering under medical supervision, intensified lifestyle modifications, and realistic expectations about the biological challenges of weight maintenance. This guide provides evidence-based strategies for transitioning off tirzepatide while minimizing weight regain.
Quick Answer: Weaning off tirzepatide without weight regain requires medical supervision for potential dose tapering, intensified lifestyle modifications including 200–300 minutes weekly of physical activity, protein-optimized nutrition, behavioral strategies like regular self-weighing, and realistic expectations about the biological tendency toward weight regain after discontinuation.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). The medication works by enhancing insulin secretion, suppressing glucagon release, slowing gastric emptying, and reducing appetite through central nervous system pathways. These mechanisms collectively promote significant weight loss, with clinical trials demonstrating average reductions of 15–22% of body weight over 72 weeks, though individual results vary by dose and patient factors.
When tirzepatide is discontinued, the pharmacological effects that supported weight loss gradually diminish. The medication has a half-life of approximately five days, meaning therapeutic effects persist for several weeks after the final dose but eventually resolve completely. As gastric emptying normalizes and appetite-suppressing signals fade, patients commonly experience reduced fullness and increased appetite as the medication's effects wane.
Weight regain after stopping tirzepatide is well-documented in clinical literature. The SURMOUNT-4 trial demonstrated that participants who discontinued tirzepatide after initial weight loss regained approximately 14% of their body weight over 52 weeks, compared to those who continued treatment. This phenomenon reflects both the reversal of medication effects and the body's metabolic adaptation to weight loss, including decreased energy expenditure and hormonal changes that favor weight regain.
Understanding that weight regain is a biological response rather than personal failure is essential for patients and clinicians. The body's homeostatic mechanisms actively defend against sustained weight loss, making pharmacological support withdrawal a vulnerable period requiring proactive management strategies and realistic expectations about the challenges ahead.
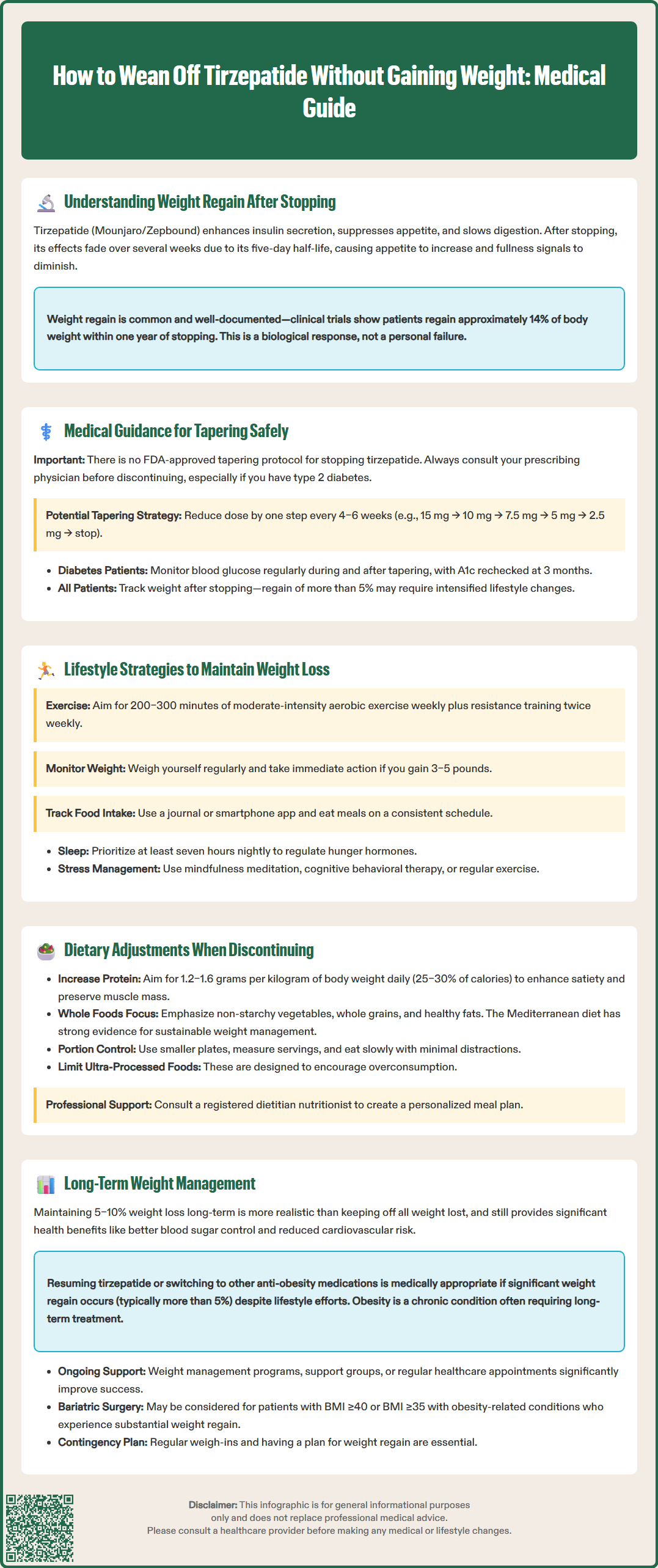
Patients considering tirzepatide discontinuation should consult their prescribing physician before making any changes to their medication regimen. The decision to stop treatment should be individualized, considering factors such as achievement of weight loss goals, medication tolerability, financial constraints, insurance coverage changes, or personal preference. For patients with type 2 diabetes, discontinuation requires careful consideration of glycemic control and potential need for alternative glucose-lowering therapies.
A potential tapering approach, based solely on clinical judgment rather than formal guidelines or comparative studies, might involve reducing the dose by one step every 4–6 weeks. For example, a patient on the 15 mg maintenance dose could step down to 10 mg, then 7.5 mg, then 5 mg, and finally 2.5 mg before complete discontinuation. This gradual reduction may allow patients to adapt to increasing appetite and implement behavioral strategies progressively. However, the clinical benefit of tapering versus abrupt discontinuation has not been formally studied for tirzepatide.
During the tapering period and after discontinuation, patients should maintain regular follow-up appointments. For those with diabetes, monitoring should include blood glucose checks as clinically indicated and hemoglobin A1c reassessment approximately 3 months after therapy changes, per American Diabetes Association guidelines. Patients should be educated about signs of worsening hyperglycemia (increased thirst, frequent urination, unexplained weight loss, blurred vision) that warrant prompt medical attention. For all patients, monitoring weight and waist circumference allows early identification of significant weight regain (typically defined as >5% of body weight), enabling timely intervention with intensified lifestyle modifications or consideration of medication resumption if clinically appropriate and meeting FDA-indicated criteria.
Successful weight maintenance after tirzepatide discontinuation requires a comprehensive approach addressing physical activity, behavioral modification, sleep hygiene, and stress management. Evidence from the National Weight Control Registry, which tracks individuals who have maintained significant weight loss long-term, provides valuable insights into effective strategies, though these findings are observational.
Physical Activity is strongly associated with sustained weight loss maintenance. The American College of Sports Medicine recommends 200–300 minutes of moderate-intensity aerobic activity weekly for weight loss maintenance, substantially more than the 150 minutes recommended for general health. This translates to approximately 45–60 minutes of activity most days of the week. Combining aerobic exercise (walking, cycling, swimming) with resistance training at least twice weekly helps preserve lean muscle mass, which is critical for maintaining metabolic rate. Increased daily movement through non-exercise activity thermogenesis—taking stairs, parking farther away, standing desks—also contributes meaningfully to energy expenditure.
Behavioral strategies proven effective for weight maintenance include regular self-weighing, which allows early detection of weight trends before significant regain occurs. A weight gain of 3–5 pounds should trigger immediate reassessment of dietary and activity patterns. Food journaling or using smartphone applications to track intake maintains awareness and accountability. Establishing a consistent eating schedule with regular meal times helps regulate appetite hormones disrupted by weight loss.
Sleep and stress management are physiologically important components of weight management. Sleep deprivation (less than seven hours nightly) is associated with disruptions in hunger hormones that may increase appetite. Chronic stress has been linked to higher cortisol levels and, in some studies, to increased abdominal fat and emotional eating behaviors. Evidence-based stress reduction techniques include mindfulness meditation, cognitive behavioral therapy, regular physical activity, and maintaining social connections. Patients should be screened for depression and anxiety, which commonly co-occur with obesity and may worsen during weight regain, potentially requiring mental health referral.
As tirzepatide's appetite-suppressing effects wane, patients typically experience increased hunger, larger portion sizes, and more frequent eating occasions. Proactive dietary modifications can help counteract these changes and support weight maintenance without the pharmacological assistance previously provided.
Protein optimization is particularly important during this transition. Increasing protein intake to 1.2–1.6 grams per kilogram of body weight daily (approximately 0.54–0.73 grams per pound, or 25–30% of total calories) may enhance satiety and preserve lean muscle mass. This target should be individualized, particularly for patients with chronic kidney disease who may require lower protein intake—consultation with a registered dietitian nutritionist (RDN) is recommended. Practical strategies include incorporating protein sources at every meal and snack: Greek yogurt, eggs, lean poultry, fish, legumes, and plant-based proteins. Including protein at breakfast may help improve satiety throughout the day for some individuals.
Dietary patterns associated with successful long-term weight management emphasize whole, minimally processed foods with high nutrient density and satiety value. Vegetables, particularly non-starchy varieties, provide volume and fiber with minimal calories. Whole grains offer sustained energy release compared to refined carbohydrates. Healthy fats from sources like nuts, avocados, and olive oil contribute to meal satisfaction. The Mediterranean dietary pattern has robust evidence for cardiovascular health and weight management sustainability, as recognized by the American Heart Association and Dietary Guidelines for Americans.
Portion control becomes increasingly important as gastric emptying normalizes and meal-induced satiety diminishes. Using smaller plates, measuring portions initially to recalibrate perception, and practicing mindful eating techniques—eating slowly, minimizing distractions, recognizing fullness cues—help prevent overconsumption. Limiting ultra-processed foods, which are engineered for palatability and overconsumption, reduces passive calorie intake. Establishing clear boundaries around high-risk foods and situations identified during treatment helps maintain dietary structure.
Patients may benefit from consultation with a registered dietitian nutritionist experienced in weight management to develop an individualized meal plan that accounts for personal preferences, cultural considerations, and metabolic needs while creating a modest caloric deficit or maintenance level appropriate for their goals.
Long-term weight management after discontinuing tirzepatide requires acknowledging that obesity is a chronic, relapsing condition with biological underpinnings that persist after weight loss. Realistic expectations, ongoing support systems, and contingency planning for weight regain are essential components of a sustainable approach.
Realistic goal-setting is critical for psychological well-being and adherence. While patients may hope to maintain their lowest achieved weight, research suggests that maintaining a portion of initial weight loss is a more achievable long-term outcome for many individuals. Even modest sustained weight loss of 5–10% provides meaningful health benefits, including improved glycemic control, reduced cardiovascular risk factors, and decreased joint stress. Reframing success around health improvements rather than solely scale numbers may improve long-term adherence and reduce discouragement.
Ongoing support structures significantly improve maintenance outcomes. Options include commercial weight management programs with demonstrated efficacy (Weight Watchers/WW, Noom), hospital-based medical weight management programs, support groups, or regular appointments with healthcare providers, dietitians, or health coaches. Accountability through regular weigh-ins, whether self-directed or professionally supervised, helps maintain focus and allows early intervention when weight trends upward.
Pharmacological considerations should be discussed openly. For some patients, weight regain despite intensive lifestyle efforts may warrant consideration of resuming tirzepatide or transitioning to alternative anti-obesity medications, provided they meet FDA-indicated criteria (BMI ≥30 kg/m² or ≥27 kg/m² with weight-related comorbidity). The American Gastroenterological Association guidelines recognize that long-term or indefinite pharmacotherapy may be appropriate for many patients with obesity, similar to treatment approaches for other chronic conditions like hypertension or diabetes. Data on intermittent GLP-1 receptor agonist use are limited; safety and efficacy of this approach are not established.
Bariatric surgery may be an appropriate consideration for eligible patients experiencing significant weight regain. Current guidelines from the American Society for Metabolic and Bariatric Surgery recommend surgical evaluation for individuals with BMI ≥40 kg/m² or BMI ≥35 kg/m² with obesity-related comorbidities.
Patients should be counseled that requesting medication resumption is medically appropriate if significant weight regain occurs (typically >5% of body weight) despite adherence to lifestyle modifications. This decision should be made collaboratively with their healthcare provider, considering individual circumstances, comorbidities, and treatment goals. The chronic nature of obesity means that long-term management strategies may need to evolve over time, and flexibility in approach supports better outcomes than rigid adherence to initial plans that prove unsustainable.
No, the FDA has not approved a specific tapering protocol for tirzepatide discontinuation. Any dose reduction strategy represents off-label clinical judgment and should be discussed with your prescribing physician, who may suggest gradually reducing the dose by one step every 4–6 weeks based on individual circumstances.
Clinical trials show that patients who discontinue tirzepatide after initial weight loss regain approximately 14% of their body weight over 52 weeks. Individual results vary based on lifestyle modifications, metabolic factors, and adherence to weight maintenance strategies implemented after discontinuation.
Yes, resuming tirzepatide may be medically appropriate if you experience significant weight regain (typically >5% of body weight) despite adherence to lifestyle modifications, provided you meet FDA criteria (BMI ≥30 kg/m² or ≥27 kg/m² with weight-related comorbidity). This decision should be made collaboratively with your healthcare provider based on your individual circumstances and treatment goals.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.