LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Why does GLP-1 increase heart rate? GLP-1 receptor agonists—medications like semaglutide (Ozempic, Wegovy), liraglutide (Victoza, Saxenda), and dulaglutide (Trulicity)—are widely prescribed for type 2 diabetes and weight management. While these drugs offer proven cardiovascular benefits, clinical trials consistently show a modest heart rate increase of 1–4 beats per minute in most patients. Understanding the mechanisms behind this effect is essential for clinicians and patients alike. This article explores the biological pathways, clinical evidence, and practical management strategies for heart rate changes associated with GLP-1 therapy.
Quick Answer: GLP-1 receptor agonists increase heart rate by an average of 1–4 beats per minute through mechanisms including sympathetic nervous system activation, hemodynamic changes, and potential effects on cardiovascular regulation pathways.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) is an incretin hormone naturally produced in the intestinal L-cells in response to food intake. GLP-1 receptor agonists, a class of medications that mimic this hormone, have become widely prescribed for type 2 diabetes management and weight loss. These medications include semaglutide (Ozempic, Wegovy), liraglutide (Victoza, Saxenda), dulaglutide (Trulicity), and tirzepatide (Mounjaro, Zepbound), which is a dual GIP/GLP-1 receptor agonist.
Beyond their well-established effects on glucose metabolism and appetite regulation, GLP-1 receptor agonists exert multiple cardiovascular effects. Large cardiovascular outcome trials have demonstrated that several agents in this class reduce major adverse cardiovascular events (MACE) in patients with type 2 diabetes, with benefits extending beyond just those with established cardiovascular disease in some trials. For example, the REWIND trial with dulaglutide included a broader population with cardiovascular risk factors. These benefits include reductions in cardiovascular death, non-fatal myocardial infarction, and non-fatal stroke, as shown in landmark trials such as LEADER (liraglutide), SUSTAIN-6 (semaglutide), and REWIND (dulaglutide).
However, alongside these cardiovascular benefits, clinical trials and real-world observations have consistently noted a modest increase in resting heart rate among patients taking GLP-1 receptor agonists. According to FDA prescribing information, this heart rate elevation typically averages approximately 1-4 beats per minute above baseline, though a subset of patients may experience more pronounced increases of 10 beats per minute or more. While this increase is generally well-tolerated, it has raised questions among clinicians and patients about the underlying mechanisms and clinical implications. Understanding why GLP-1 therapy affects heart rate requires examining both the direct pharmacological actions of these medications and their indirect metabolic and hemodynamic effects on the cardiovascular system.
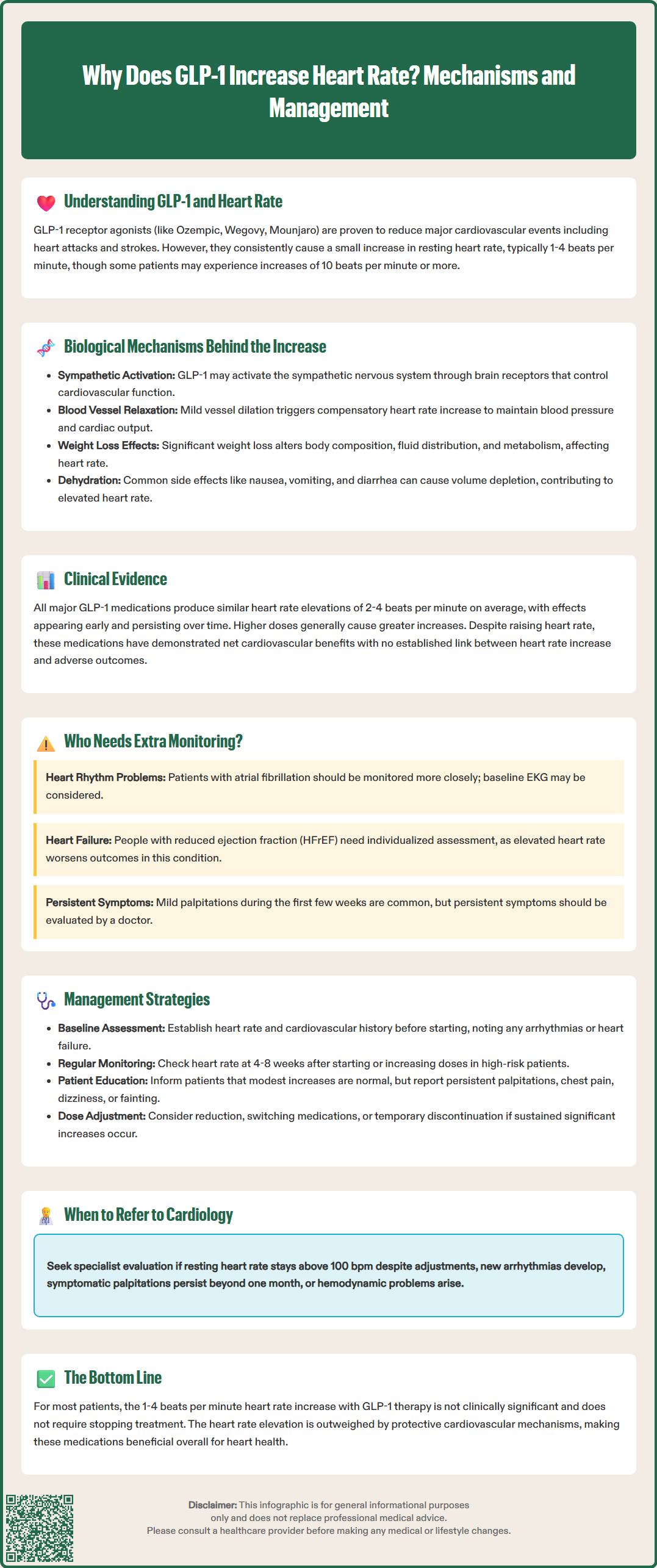
The mechanisms underlying GLP-1-associated heart rate increases are multifactorial and not fully understood. Several biological pathways have been proposed, though the evidence in humans remains limited for many of these hypotheses.
Sympathetic nervous system effects may contribute to heart rate changes. GLP-1 receptors have been identified in various tissues involved in cardiovascular regulation, including areas of the central nervous system that influence autonomic function. Some studies suggest that GLP-1 receptor activation might influence sympathetic outflow, potentially affecting heart rate through autonomic pathways, though human data are mixed and largely inferential.
Animal studies have demonstrated that GLP-1 receptor agonists can increase sympathetic nerve activity, particularly to the heart and kidneys. This sympathetic activation may be mediated through central nervous system pathways, as GLP-1 receptors are present in the hypothalamus and brainstem regions that regulate cardiovascular function. However, the exact neuroanatomical circuits and their relevance to humans remain under investigation.
Hemodynamic changes associated with GLP-1 therapy may also contribute to heart rate elevation. Some research suggests these medications may cause mild vasodilation and potentially reduce systemic vascular resistance, which could trigger a compensatory increase in heart rate to maintain cardiac output and blood pressure. Additionally, the significant weight loss achieved with GLP-1 receptor agonists leads to changes in body composition, fluid distribution, and metabolic rate, all of which can influence cardiovascular hemodynamics.
Other proposed mechanisms include potential effects on cardiac ion channels and alterations in baroreceptor sensitivity, though these remain speculative in humans. More practical contributors to heart rate increases, especially early in therapy, may include volume depletion from gastrointestinal side effects such as nausea, vomiting, and diarrhea, which are common during GLP-1 receptor agonist initiation.
The relative contribution of each mechanism likely varies among individuals and may depend on baseline cardiovascular status, concurrent medications, and the specific GLP-1 receptor agonist used. Further research is needed to better characterize these mechanisms in humans.
Clinical trial data consistently demonstrate modest heart rate increases with GLP-1 receptor agonist therapy. In the LEADER trial evaluating liraglutide, patients experienced a mean heart rate increase of approximately 3 beats per minute compared to placebo over the study duration. The SUSTAIN-6 trial with semaglutide showed similar findings, with heart rate elevations of 2-3 beats per minute. These increases were observed early in treatment and generally persisted throughout the trial periods.
The magnitude of heart rate increase appears to vary among different GLP-1 receptor agonists. According to FDA prescribing information, liraglutide typically produces mean increases of approximately 2-3 beats per minute, though some individuals may experience more pronounced elevations. Dulaglutide and semaglutide generally cause similar average increases (2-4 beats per minute), with individual responses varying considerably. Exenatide, available in both immediate-release and extended-release formulations, shows comparable effects on heart rate. Tirzepatide, the dual GIP/GLP-1 receptor agonist, has demonstrated mean heart rate increases of approximately 2-4 beats per minute in the SURPASS clinical trial program, as reflected in the Mounjaro and Zepbound prescribing information.
Importantly, no clear association has been established between the heart rate increase with GLP-1 therapy and adverse cardiovascular outcomes. Despite the elevated heart rate, cardiovascular outcome trials have shown net cardiovascular benefits, suggesting that the modest chronotropic effect is outweighed by other protective mechanisms. Post-hoc analyses from these trials have not identified heart rate increase as a predictor of cardiovascular events, though these analyses have limitations.
The degree of heart rate response may vary among patients, though specific predictors are not well-established in the literature. The heart rate elevation is generally dose-dependent, with higher doses producing greater increases, though this relationship is not strictly linear across all agents.
For the majority of patients, the heart rate increase associated with GLP-1 receptor agonist therapy is not clinically significant and does not require treatment modification. The typical elevation of 1-4 beats per minute falls within normal physiological variation and is comparable to the heart rate changes seen with routine daily activities. Current evidence from large cardiovascular outcome trials provides reassurance that this modest chronotropic effect does not translate into increased cardiovascular risk for most patients.
However, certain patient populations warrant closer monitoring. Patients with pre-existing tachyarrhythmias, particularly atrial fibrillation or atrial flutter, should be evaluated carefully before initiating GLP-1 therapy. While there is no definitive evidence that GLP-1 receptor agonists worsen arrhythmia control, the additional heart rate increase could theoretically affect symptoms or ventricular rate control in susceptible individuals. Baseline electrocardiography may be considered in patients with known arrhythmias or significant cardiac history.
Patients with heart failure with reduced ejection fraction (HFrEF) represent another group requiring individualized assessment. Elevated resting heart rate is an independent risk factor for adverse outcomes in heart failure, and beta-blocker therapy to reduce heart rate is a cornerstone of HFrEF management. Small clinical trials of liraglutide in HFrEF (FIGHT and LIVE) have shown heart rate increases and potential safety signals, suggesting caution in this population. It's important to note that GLP-1 receptor agonists are not indicated for heart failure treatment, and SGLT2 inhibitors are the preferred agents with established benefits in heart failure according to current guidelines. The SELECT trial with semaglutide showed cardiovascular benefits in a population with established cardiovascular disease but did not specifically address outcomes in patients with decompensated heart failure.
Symptomatic considerations are also important. Some patients may experience palpitations, particularly during the initial weeks of GLP-1 therapy. These symptoms often improve with continued treatment, but persistent or bothersome palpitations warrant clinical evaluation to exclude other causes and assess whether the heart rate increase is excessive. Patients should be counseled that mild awareness of heartbeat is not uncommon during treatment initiation.
FDA prescribing information for some GLP-1 receptor agonists (particularly those approved for weight management) includes recommendations to monitor heart rate at regular intervals and consider discontinuation for sustained increases in resting heart rate. This guidance should be incorporated into clinical decision-making when evaluating the significance of heart rate changes in individual patients.
Baseline assessment is the foundation of appropriate management. Before initiating GLP-1 receptor agonist therapy, clinicians should document baseline heart rate and review the patient's cardiovascular history, including any arrhythmias, heart failure, or symptoms such as palpitations. Patients taking medications that affect heart rate, particularly beta-blockers, calcium channel blockers, or antiarrhythmic drugs, should be identified, as these may modify the heart rate response to GLP-1 therapy.
Monitoring strategies should be individualized based on patient risk factors and align with FDA prescribing information, which recommends monitoring heart rate at regular intervals for some GLP-1 receptor agonists. For most patients without cardiovascular disease, routine heart rate monitoring at follow-up visits is appropriate. However, patients with established cardiovascular disease, particularly those with heart failure or arrhythmias, may benefit from more structured monitoring. This could include:
Heart rate assessment at 4-8 weeks after initiation or dose escalation
Periodic electrocardiography if arrhythmias are suspected
Patient self-monitoring of pulse if symptomatic palpitations occur
Evaluation of heart rate control in patients with atrial fibrillation
When evaluating tachycardia in patients on GLP-1 therapy, clinicians should assess for other potential causes, including dehydration (especially from GI side effects), anemia, hyperthyroidism, stimulant use, infection, or other medications.
Patient education is essential for appropriate management. Patients should be informed that a modest heart rate increase is an expected effect of GLP-1 therapy and does not typically indicate a problem. They should be advised to report persistent palpitations, chest discomfort, lightheadedness, or syncope, as these symptoms warrant further evaluation. Reassurance that the heart rate increase is generally well-tolerated can alleviate anxiety.
Medication adjustments may be necessary in some cases, particularly if patients experience sustained significant heart rate increases. FDA prescribing information for some GLP-1 receptor agonists advises considering discontinuation for sustained increases in resting heart rate. Management options include dose reduction of the GLP-1 receptor agonist, switching to an alternative agent in the class, or temporarily discontinuing therapy to assess whether heart rate normalizes. However, such interventions should be balanced against the metabolic and cardiovascular benefits of continued GLP-1 therapy.
For patients with heart failure taking beta-blockers, optimization of beta-blocker dosing should be prioritized to maintain target heart rate goals in accordance with heart failure guidelines. If the addition of GLP-1 therapy results in heart rate elevation above target ranges, increasing the beta-blocker dose (if tolerated) may be considered. Close collaboration between endocrinology and cardiology is beneficial in complex cases.
Referral triggers include: sustained resting heart rate >100 beats per minute despite dose adjustment, new or worsening arrhythmias temporally related to GLP-1 initiation, symptomatic palpitations that persist beyond the first month of therapy, or signs of hemodynamic compromise. Cardiology consultation should be considered for patients with complex cardiovascular disease when questions arise about the appropriateness of continuing GLP-1 therapy in the context of heart rate changes. In most cases, however, the modest heart rate increase associated with GLP-1 receptor agonists can be managed effectively in the primary care or endocrinology setting with appropriate monitoring and patient education.
For most patients, the 1–4 beat per minute increase is not clinically significant and does not increase cardiovascular risk. Large outcome trials have demonstrated net cardiovascular benefits despite this modest heart rate elevation.
All GLP-1 receptor agonists cause similar modest heart rate increases of approximately 2–4 beats per minute on average, including liraglutide, semaglutide, dulaglutide, and tirzepatide. Individual responses vary considerably among patients.
Most patients do not need to discontinue GLP-1 therapy for modest heart rate increases. However, FDA prescribing information recommends considering discontinuation for sustained significant increases in resting heart rate, and patients with persistent palpitations or heart rate above 100 bpm should consult their healthcare provider.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.