LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Semaglutide, a GLP-1 receptor agonist approved by the FDA for type 2 diabetes and chronic weight management, has important effects on liver enzymes that clinicians and patients should understand. Clinical evidence demonstrates that semaglutide typically improves liver enzyme profiles, particularly in patients with metabolic dysfunction-associated steatotic liver disease (MASLD). These hepatic benefits appear to result primarily from weight loss and improved metabolic parameters rather than direct liver effects. While semaglutide has a favorable hepatic safety profile, understanding its relationship with liver function helps optimize patient monitoring and outcomes.
Quick Answer: Semaglutide typically improves liver enzyme levels in patients with metabolic dysfunction-associated steatotic liver disease through weight loss and metabolic improvements rather than direct hepatic effects.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management and chronic weight management. Understanding its effects on liver enzymes is important for both patients and healthcare providers, particularly given the high prevalence of fatty liver disease in populations with obesity and diabetes.
Semaglutide works by mimicking the natural hormone GLP-1, which enhances insulin secretion in response to meals, suppresses glucagon release, slows gastric emptying, and reduces appetite through central nervous system pathways. These mechanisms lead to improved glycemic control and significant weight loss. Semaglutide is not metabolized by the liver's cytochrome P450 enzyme system; instead, it undergoes proteolytic degradation similar to endogenous proteins, which contributes to its low drug-drug interaction potential via hepatic pathways.
Clinical observations suggest that semaglutide may improve liver enzyme levels in many patients, particularly those with metabolic dysfunction-associated steatotic liver disease (MASLD, formerly known as non-alcoholic fatty liver disease or NAFLD). This beneficial effect appears to be primarily indirect, resulting from weight loss and improved metabolic parameters rather than direct hepatic action. As visceral adiposity decreases and insulin sensitivity improves, hepatic steatosis often diminishes, leading to normalization of elevated transaminases.
While semaglutide generally has a favorable hepatic safety profile, individual responses vary. Some patients may experience transient elevations in liver enzymes, though these are typically mild and resolve without intervention. It's also important to note that GLP-1 receptor agonists, including semaglutide, carry an FDA-labeled risk of gallbladder disease, which can sometimes present with abnormal liver function tests.
Substantial clinical trial data demonstrate semaglutide's effects on liver enzymes and hepatic health. The SUSTAIN clinical trial program, which evaluated semaglutide for type 2 diabetes, showed improvements in liver enzyme profiles among participants. In these studies, patients receiving semaglutide experienced reductions in alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels compared to baseline, with greater improvements observed in those achieving more substantial weight loss.
The STEP trials, which examined semaglutide 2.4 mg for weight management, provided additional evidence of hepatic benefits. In STEP 1, participants receiving semaglutide had reductions in ALT levels, with more pronounced decreases observed in those with elevated baseline ALT values. These improvements correlated strongly with the degree of weight reduction, supporting the hypothesis that metabolic improvement drives hepatic benefits. Importantly, the incidence of treatment-emergent elevations in liver enzymes was low and comparable to placebo groups.
More targeted research has examined semaglutide's effects specifically in patients with liver disease. A 2021 study published in the New England Journal of Medicine found that semaglutide 0.4 mg daily led to resolution of non-alcoholic steatohepatitis (NASH) in 59% of participants compared to 17% in the placebo group. This was accompanied by significant reductions in liver enzyme levels and hepatic fat content measured by MRI. However, it's important to note that the trial did not meet its primary endpoint of fibrosis improvement, and semaglutide is not FDA-approved for the treatment of NASH or metabolic dysfunction-associated steatohepatitis (MASH).
Post-marketing surveillance data from the FDA Adverse Event Reporting System (FAERS) indicate that serious hepatic adverse events with semaglutide are rare, though such spontaneous reporting systems have inherent limitations and cannot establish true incidence or definitive causality. The overall evidence supports a favorable hepatic safety profile, with potential therapeutic benefits for patients with underlying liver disease related to metabolic syndrome.
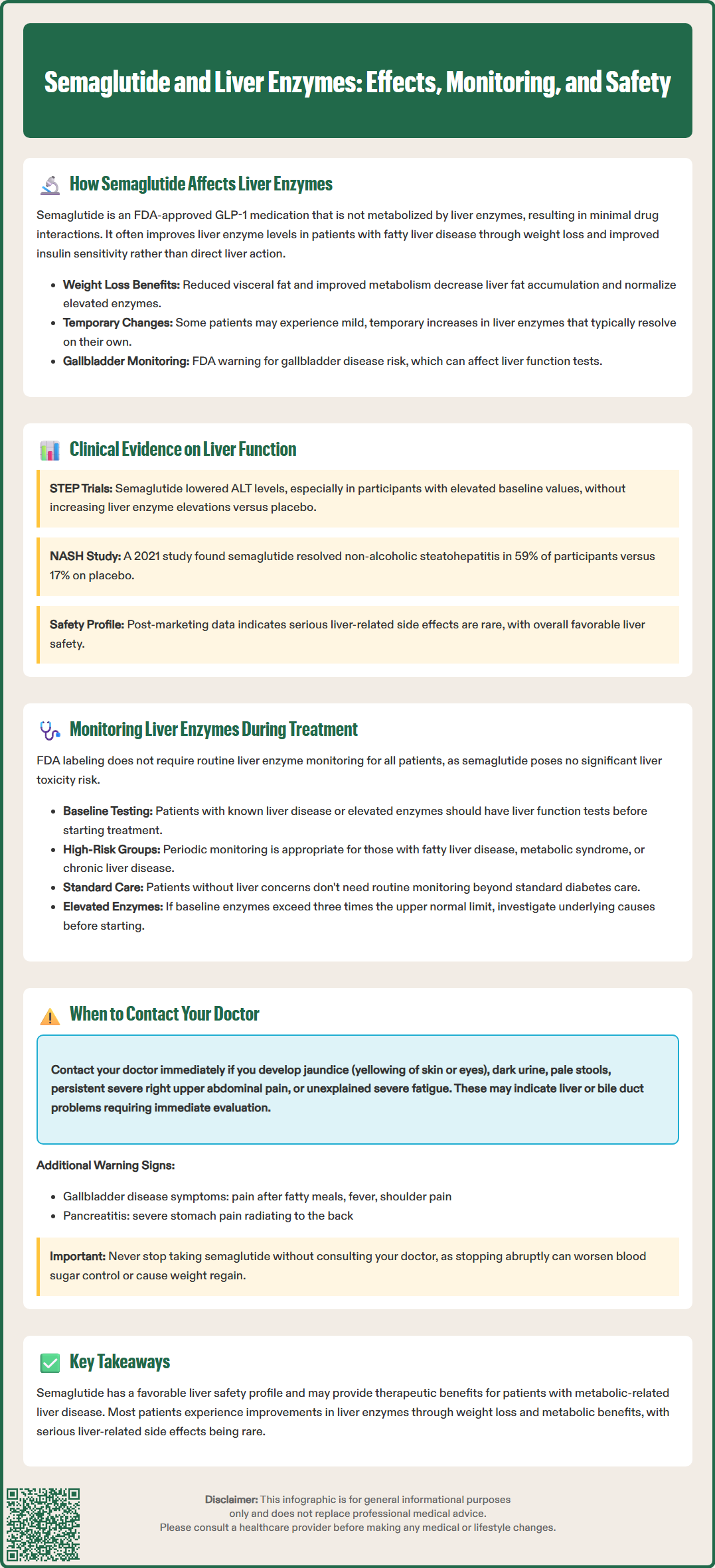
Current FDA labeling for semaglutide does not mandate routine liver enzyme monitoring in all patients, as the medication is not associated with significant hepatotoxicity risk. However, clinical judgment should guide individualized monitoring strategies based on patient-specific factors and baseline hepatic status. The American Diabetes Association (ADA) and American Association of Clinical Endocrinologists (AACE) guidelines do not specify unique monitoring requirements for semaglutide beyond standard diabetes care protocols.
For patients with known liver disease or elevated baseline transaminases, obtaining liver function tests (LFTs) before initiating semaglutide provides a valuable reference point. A comprehensive hepatic panel typically includes ALT, AST, alkaline phosphatase (ALP), total and direct bilirubin, and albumin. Baseline assessment helps distinguish pre-existing hepatic abnormalities from treatment-related changes and allows clinicians to track improvements that often accompany metabolic optimization.
During treatment, periodic monitoring may be appropriate for specific populations. Patients with MASLD, MASH, or metabolic syndrome may benefit from LFT assessment at intervals consistent with American Association for the Study of Liver Diseases (AASLD) guidance. For patients with suspected advanced liver disease, calculating the Fibrosis-4 (FIB-4) index can help determine the need for hepatology referral. Those with pre-existing chronic liver disease warrant closer surveillance, though semaglutide is not contraindicated in compensated liver disease. If baseline ALT or AST levels exceed three times the upper limit of normal (ULN), evaluation for underlying causes is appropriate, though this need not necessarily delay semaglutide initiation if benefits are deemed to outweigh risks.
Patients without baseline hepatic concerns typically do not require routine LFT monitoring beyond what is standard for diabetes or obesity management. However, if symptoms suggestive of hepatic dysfunction develop—such as jaundice, dark urine, persistent right upper quadrant pain, or unexplained fatigue—prompt laboratory evaluation is warranted. Additionally, clinicians should be aware that semaglutide carries labeled warnings for gallbladder disease and pancreatitis, which can present with abnormal liver enzymes and require appropriate evaluation.
While semaglutide has a favorable hepatic safety profile, patients should remain alert to symptoms that may indicate liver problems requiring medical evaluation. Understanding when to seek medical attention empowers patients to participate actively in their care and ensures timely intervention if complications arise.
Patients should contact their healthcare provider promptly if they develop jaundice—yellowing of the skin or whites of the eyes—which may indicate significant liver dysfunction or bile duct obstruction. Similarly, dark-colored urine (resembling tea or cola) or pale, clay-colored stools suggest altered bilirubin metabolism warranting investigation. These signs, while rare with semaglutide, should never be ignored regardless of the medication involved.
Persistent or severe abdominal pain, particularly in the right upper quadrant where the liver is located, requires medical assessment. While semaglutide commonly causes mild gastrointestinal symptoms like nausea during dose escalation, severe or persistent right-sided abdominal pain differs from typical GI side effects and may indicate hepatobiliary issues. Patients should also report unexplained fatigue that seems disproportionate to their usual experience, especially if accompanied by other symptoms, as this can reflect impaired hepatic function.
Certain symptoms warrant urgent medical attention, including jaundice with fever or confusion, severe abdominal pain with vomiting, or signs of gastrointestinal bleeding. Patients should also be aware that GLP-1 receptor agonists like semaglutide carry an FDA-labeled risk of gallbladder disease (symptoms may include fever, pain after fatty meals, or pain radiating to the right shoulder) and pancreatitis (severe epigastric pain often radiating to the back).
It is important to emphasize that most patients tolerate semaglutide well without hepatic complications. The medication often improves liver health markers in individuals with fatty liver disease. However, maintaining open communication with healthcare providers about any unusual symptoms ensures appropriate evaluation and continued safe use of this effective therapeutic agent. Patients should never discontinue semaglutide without medical guidance, as abrupt cessation may lead to worsening glycemic control or weight regain.
Current FDA labeling does not mandate routine liver enzyme monitoring for all patients taking semaglutide, as the medication is not associated with significant hepatotoxicity risk. However, baseline liver function tests may be appropriate for patients with known liver disease or elevated transaminases, with individualized monitoring based on clinical judgment.
Yes, clinical evidence shows that semaglutide often improves liver enzyme levels in patients with metabolic dysfunction-associated steatotic liver disease (MASLD). These improvements result primarily from weight loss and enhanced metabolic parameters, leading to reduced hepatic steatosis and normalization of elevated transaminases.
Contact your healthcare provider promptly if you develop jaundice (yellowing of skin or eyes), dark-colored urine, pale stools, persistent right upper quadrant abdominal pain, or unexplained severe fatigue. While semaglutide has a favorable hepatic safety profile, these symptoms warrant medical evaluation to rule out hepatobiliary complications.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.