LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Why does metformin cause blurry vision? Many patients taking this first-line diabetes medication report visual disturbances, raising concerns about medication safety. While metformin itself does not directly damage eye structures, blurry vision commonly occurs as an indirect effect of blood glucose fluctuations. When metformin effectively lowers elevated blood sugar levels, the resulting osmotic changes temporarily alter the lens shape and refractive properties. Understanding this mechanism helps patients distinguish between benign, self-limiting vision changes and serious complications requiring immediate medical attention. This article examines the relationship between metformin therapy and vision disturbances, providing evidence-based guidance for patients and clinicians.
Quick Answer: Metformin does not directly cause blurry vision but blood glucose fluctuations during treatment create osmotic changes in the eye's lens, temporarily altering its shape and causing refractive vision changes that typically resolve within 6-8 weeks.
Metformin is a first-line oral medication for type 2 diabetes mellitus, prescribed to millions of Americans to help control blood glucose levels. As a biguanide antihyperglycemic agent, metformin works primarily by decreasing hepatic glucose production, reducing intestinal glucose absorption, and improving insulin sensitivity in peripheral tissues. The medication does not stimulate insulin secretion, which significantly reduces the risk of hypoglycemia compared to other diabetes medications.
The most frequently reported side effects of metformin are gastrointestinal in nature, affecting approximately 20-30% of patients. These include diarrhea, nausea, abdominal discomfort, and metallic taste. Most gastrointestinal symptoms are dose-dependent and typically resolve within the first few weeks of treatment. Starting with a low dose and gradually titrating upward, or using extended-release formulations, can minimize these effects.
Less common but clinically significant adverse effects include vitamin B12 deficiency with long-term use. Periodic B12 monitoring is recommended for long-term users, especially those with anemia or neuropathy. Lactic acidosis, though rare (fewer than 10 cases per 100,000 patient-years), represents the most serious potential complication. According to FDA labeling, metformin is contraindicated in patients with an estimated glomerular filtration rate (eGFR) below 30 mL/min/1.73 m² or in those with acute or chronic metabolic acidosis. It should be used cautiously or avoided in unstable heart failure, hypoxic states, or hepatic impairment due to increased lactic acidosis risk.
Metformin should be temporarily discontinued before or at the time of procedures involving iodinated contrast media in patients with eGFR 30-60 mL/min/1.73 m², liver disease, alcoholism, or heart failure. Renal function should be reassessed 48 hours after the procedure.
Vision changes, including blurry vision, are reported by some patients taking metformin, though the relationship between metformin and visual disturbances requires careful clinical evaluation to determine the underlying cause.
Metformin is not known to have direct toxic effects on ocular structures, the lens, retina, or optic nerve. The medication does not appear in the FDA labeling as having vision changes as a primary adverse effect attributable to the drug's chemical action. However, patients taking metformin may experience visual disturbances for several indirect reasons related to diabetes management.
The most common explanation for blurry vision in patients starting or adjusting metformin therapy relates to fluctuations in blood glucose levels. When metformin effectively lowers elevated blood sugar, the resulting change in glucose concentration can temporarily affect the lens of the eye. The crystalline lens is highly sensitive to osmotic changes, and shifts in blood glucose alter the fluid balance within the lens, changing its shape and refractive properties. This phenomenon is well-documented in diabetes management and typically resolves as glucose levels stabilize.
Another consideration involves the underlying progression of diabetic eye disease. Patients with type 2 diabetes are at increased risk for diabetic retinopathy, macular edema, and cataracts—conditions that can cause vision changes independent of medication use. The timing of starting metformin may coincidentally overlap with the natural progression of these complications, leading patients to attribute vision changes to the medication rather than the disease process itself.
Importantly, rapid improvement in glycemic control can sometimes temporarily worsen existing diabetic retinopathy in some patients. This paradoxical effect is well-recognized and should be considered when vision changes occur after initiating or intensifying diabetes treatment.
Additionally, some patients may experience vision changes related to other factors such as dehydration (particularly if experiencing gastrointestinal side effects), changes in blood pressure, or concurrent medications. A thorough clinical evaluation is essential to differentiate between these various potential causes and ensure appropriate management.
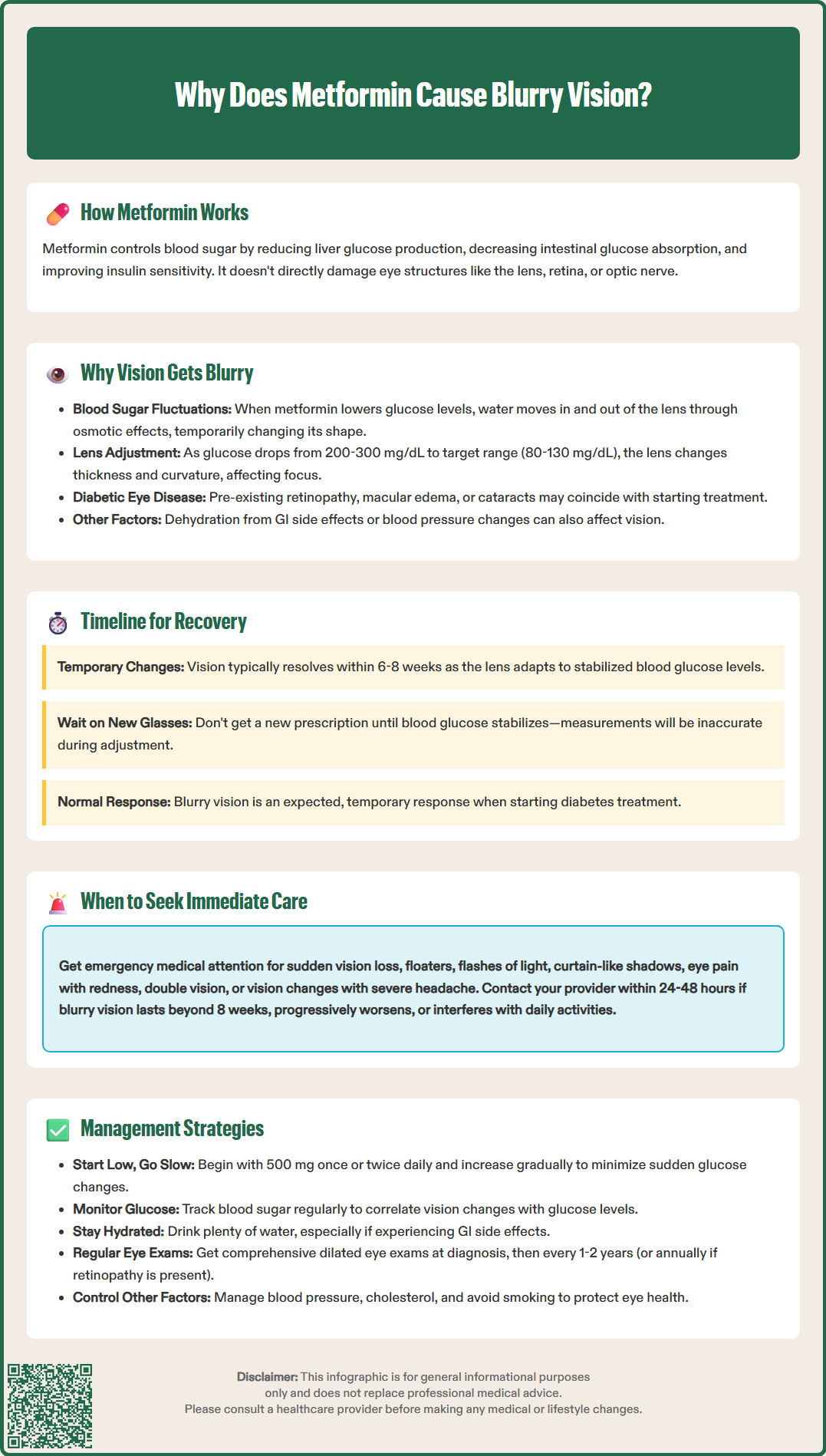
The relationship between blood glucose fluctuations and vision changes is well-established in diabetes care and represents the most likely explanation for blurry vision in patients taking metformin. When blood glucose levels change—whether rising or falling—the osmotic gradient between the bloodstream and ocular tissues shifts, directly affecting the lens of the eye.
The mechanism involves osmotic lens swelling or shrinkage. In hyperglycemia, excess glucose enters the lens and is converted to sorbitol through the aldose reductase pathway. Sorbitol accumulates because it cannot easily cross cell membranes, drawing water into the lens and causing it to swell. Conversely, when metformin effectively lowers elevated blood glucose levels, water moves out of the lens, causing temporary changes in lens thickness and curvature. These refractive changes alter how light focuses on the retina, resulting in blurred vision.
Patients newly diagnosed with diabetes or those with previously uncontrolled blood glucose often experience vision changes when treatment begins. As metformin brings glucose levels from elevated ranges (often 200-300 mg/dL or higher) down toward target ranges (typically 80-130 mg/dL fasting for many nonpregnant adults, though targets should be individualized), the lens undergoes adaptation. This adjustment period typically lasts several weeks, often up to 6-8 weeks, as the lens stabilizes to the new glucose environment.
Clinical guidance emphasizes that patients should be counseled about this temporary phenomenon. Vision typically improves and stabilizes once blood glucose control is maintained consistently. Importantly, patients should be advised against obtaining new eyeglass prescriptions until their blood glucose levels have stabilized, as refractive error measurements will be inaccurate during this period of fluctuation. This recommendation is particularly important for patients experiencing significant glucose reduction with metformin initiation.
While temporary blurry vision related to blood glucose stabilization is generally benign and self-limiting, certain vision changes warrant prompt medical evaluation. Patients should be educated about warning signs that require immediate attention versus those that can be monitored during routine follow-up.
Seek immediate medical attention if you experience:
Sudden vision loss or significant vision reduction in one or both eyes
Sudden painless severe vision loss (possible central retinal artery occlusion)
Floaters, flashes of light, or a curtain-like shadow across your visual field (possible retinal detachment)
Eye pain, redness, or discharge accompanying vision changes
Double vision or new onset of seeing halos around lights
Vision changes accompanied by severe headache, confusion, or neurological symptoms
These symptoms may indicate serious conditions such as retinal detachment, acute angle-closure glaucoma, diabetic macular edema, or other emergencies requiring urgent ophthalmologic evaluation.
Contact your healthcare provider within 24-48 hours if:
Blurry vision persists beyond 8 weeks of stable metformin therapy
Vision changes worsen progressively rather than improving
You experience vision disturbances along with symptoms of hypoglycemia (shakiness, sweating, confusion) or hyperglycemia (excessive thirst, frequent urination, fatigue)
You have difficulty performing daily activities due to vision changes
Your healthcare provider can assess whether vision changes are related to glucose fluctuations, medication effects, or underlying diabetic eye disease. Blood glucose monitoring records are invaluable during this evaluation, as they help correlate vision symptoms with glucose patterns. According to American Diabetes Association guidelines, all patients with type 2 diabetes should receive comprehensive dilated eye examinations by an ophthalmologist or optometrist at diagnosis. If no retinopathy is present and glycemic control is good, examinations every 1-2 years may be considered; otherwise, annual examinations are recommended.
Effective management of vision changes during metformin therapy focuses on glucose stabilization, patient education, and appropriate monitoring. A systematic approach can minimize discomfort and ensure patient safety while achieving glycemic control.
Optimize metformin dosing and titration. Starting metformin at a low dose (500 mg once or twice daily) and gradually increasing over several weeks allows for more gradual glucose reduction, potentially minimizing the magnitude of osmotic lens changes. Extended-release formulations may help reduce gastrointestinal side effects, which can improve medication adherence.
Monitor blood glucose consistently. Regular self-monitoring of blood glucose (SMBG) helps identify patterns and correlate vision changes with glucose levels. Patients should check fasting glucose and post-meal readings as recommended by their healthcare provider. Continuous glucose monitoring (CGM) systems, when available, provide comprehensive data about glucose trends and variability.
Maintain adequate hydration. Proper fluid intake supports overall metabolic function. This is particularly important for patients experiencing gastrointestinal side effects from metformin, which can lead to dehydration and potentially worsen vision symptoms.
Delay vision correction. Patients should postpone obtaining new eyeglass or contact lens prescriptions until blood glucose levels have stabilized for several weeks. Refractive measurements during periods of fluctuating glucose will not accurately reflect stable vision.
Ensure comprehensive eye care. All patients with diabetes require regular ophthalmologic evaluation regardless of symptoms. Dilated eye examinations can detect diabetic retinopathy, macular edema, and other complications early when treatment is most effective. Patients with known retinopathy may require more frequent monitoring.
Address contributing factors. Review all medications for potential interactions or additive effects. Optimize management of hypertension and hyperlipidemia, which contribute to diabetic eye disease progression. Smoking cessation should be strongly encouraged, as tobacco use significantly increases risk of diabetic complications including retinopathy.
Blurry vision related to blood glucose stabilization typically resolves within 6-8 weeks as glucose levels stabilize. If vision changes persist beyond this period or worsen, contact your healthcare provider for evaluation.
Do not stop metformin without consulting your healthcare provider. Temporary blurry vision from glucose fluctuations is usually benign and self-limiting, but your provider should evaluate the cause and determine appropriate management.
Metformin does not have direct toxic effects on eye structures and does not cause permanent vision damage. However, all patients with diabetes require regular comprehensive eye examinations to monitor for diabetic retinopathy and other complications.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.