LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Heartburn is one of the most commonly reported side effects among patients taking semaglutide (Ozempic, Wegovy, Rybelsus), a GLP-1 receptor agonist used for type 2 diabetes and weight management. Understanding why semaglutide causes heartburn can help patients and healthcare providers anticipate and manage this uncomfortable symptom effectively. The mechanism primarily involves delayed gastric emptying, which increases stomach pressure and promotes acid reflux into the esophagus. While heartburn can be bothersome, it is typically manageable through dietary modifications, lifestyle adjustments, and when necessary, acid-suppressing medications. Most patients experience improvement as their bodies adapt to treatment.
Quick Answer: Semaglutide causes heartburn by delaying gastric emptying, which increases stomach pressure and allows acidic contents to flow backward into the esophagus.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus (under brand names Ozempic and Rybelsus) and chronic weight management (Wegovy). This medication works by mimicking the action of naturally occurring GLP-1, a hormone that regulates blood glucose levels and appetite. By binding to GLP-1 receptors throughout the body, semaglutide enhances insulin secretion in response to meals, suppresses glucagon release, and slows gastric emptying—the rate at which food moves from the stomach into the small intestine.
The gastrointestinal system contains a high concentration of GLP-1 receptors, which explains why digestive side effects are among the most commonly reported adverse reactions to semaglutide therapy. According to FDA prescribing information, gastrointestinal adverse effects occur in a substantial proportion of patients, particularly during dose initiation and escalation. These effects include nausea, vomiting, diarrhea, abdominal pain, constipation, and gastroesophageal reflux disease (GERD) symptoms such as heartburn.
The mechanism by which semaglutide affects the digestive tract primarily involves slowing gastric emptying, though this effect tends to diminish over time with continued use. It's important to note that semaglutide is not recommended for patients with severe gastroparesis, as it could potentially worsen this condition. While digestive side effects can be uncomfortable, they are generally predictable, dose-dependent, and often improve with continued treatment as the body adapts to the medication.
Heartburn associated with semaglutide use results primarily from the medication's effect on gastric emptying and gastrointestinal motility. By activating GLP-1 receptors in the stomach and gastrointestinal tract, semaglutide significantly delays the movement of food from the stomach into the duodenum. This delayed gastric emptying means that stomach contents remain in the gastric chamber for extended periods, increasing intragastric pressure and the likelihood of gastroesophageal reflux—the backward flow of stomach acid into the esophagus.
When gastric contents are retained longer, the prolonged distension of the stomach can create mechanical conditions that favor reflux, particularly when lying down or bending over. The increased volume and pressure within the stomach may make it easier for acidic contents to flow back into the esophagus, especially in patients with pre-existing risk factors.
The relationship between semaglutide and heartburn is further complicated by individual patient factors. Patients with pre-existing GERD, hiatal hernia, or obesity (a common indication for semaglutide) may be more susceptible to reflux symptoms. Most digestive side effects, including heartburn, typically improve with continued treatment or dose adjustment. However, it's worth noting that rare cases of persistent gastrointestinal dysmotility have been reported in postmarketing surveillance, reinforcing why semaglutide is not recommended for patients with severe gastroparesis.
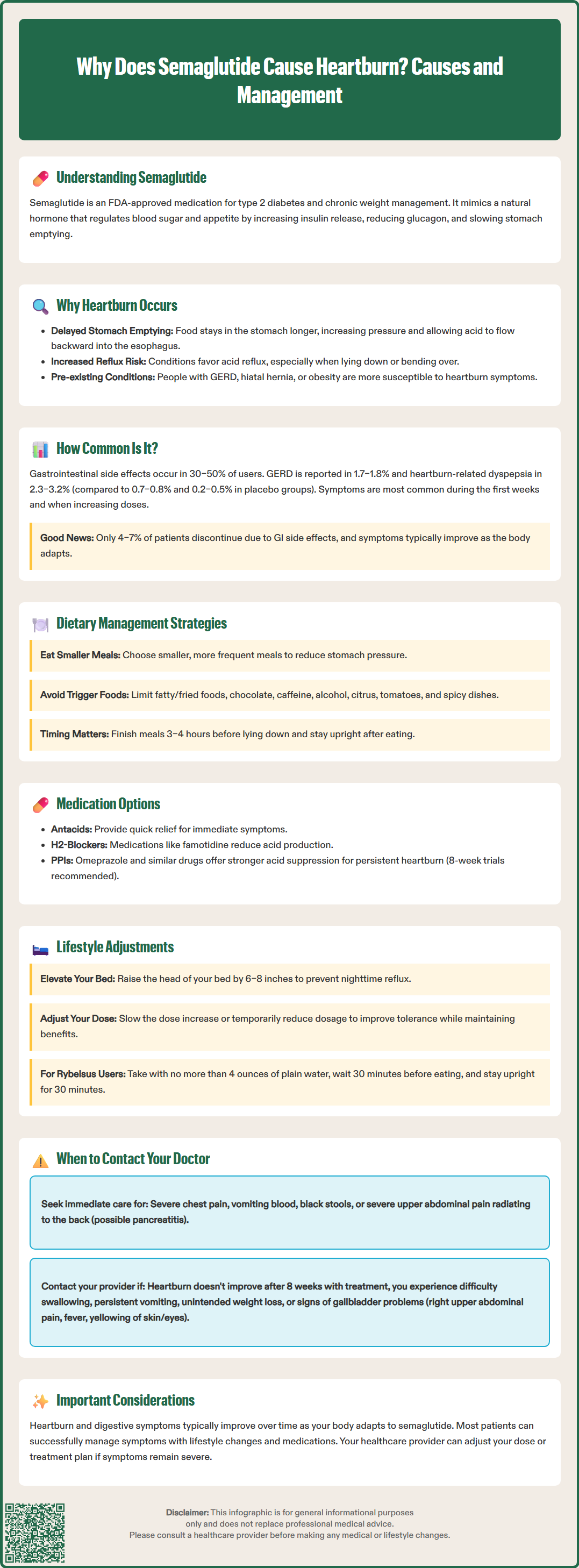
Gastrointestinal side effects are the most frequently reported adverse reactions to semaglutide across all approved formulations and indications. According to FDA prescribing information and clinical trial data, the incidence of GERD-related symptoms, including heartburn, varies depending on the dose, formulation, and patient population studied. In the SUSTAIN clinical trial program evaluating injectable semaglutide for type 2 diabetes, gastrointestinal adverse events occurred in 30–50% of participants, with nausea being most common.
In the STEP trials examining semaglutide 2.4 mg (Wegovy) for weight management, gastrointestinal adverse events were reported by approximately 44–74% of participants receiving semaglutide compared to 25–47% receiving placebo. Specifically, GERD was reported in 1.7–1.8% of Wegovy patients versus 0.7–0.8% of placebo patients according to FDA prescribing information. Dyspepsia (which includes heartburn symptoms) occurred in 2.3–3.2% of those on Wegovy compared to 0.2–0.5% on placebo. The oral formulation (Rybelsus) demonstrates comparable gastrointestinal tolerability profiles.
Several factors influence the likelihood and severity of heartburn with semaglutide use. The incidence is typically highest during the initial weeks of treatment and during dose escalation periods. Most clinical trials employed gradual dose titration protocols specifically to minimize gastrointestinal side effects, with discontinuation rates due to GI adverse events ranging from 4–7% in the STEP trials. Patient-specific factors also play a role—individuals with pre-existing GERD, those taking higher doses, and patients with delayed baseline gastric emptying may experience more pronounced symptoms. Importantly, for many patients, heartburn and other gastrointestinal symptoms diminish over time as physiological adaptation occurs, though a subset of patients may experience persistent symptoms requiring intervention or medication discontinuation.
Effective management of semaglutide-related heartburn involves both lifestyle modifications and, when necessary, pharmacological interventions. Patient education regarding expected side effects and practical strategies can help minimize discomfort while maintaining therapeutic benefit from diabetes or weight management treatment.
Dietary and lifestyle modifications form the foundation of heartburn management:
Meal size and frequency: Consuming smaller, more frequent meals reduces gastric distension and pressure, decreasing reflux likelihood. Given semaglutide's effect on gastric emptying, avoiding large meals is particularly important.
Food choices: Limiting foods that trigger reflux—including fatty or fried foods, chocolate, caffeine, alcohol, citrus, tomatoes, and spicy dishes—can significantly reduce symptoms.
Eating schedule: Finishing meals at least 3–4 hours before lying down allows more time for gastric emptying and reduces nocturnal reflux.
Positional strategies: Elevating the head of the bed by 6–8 inches and avoiding lying flat immediately after eating helps prevent acid reflux through gravitational assistance.
Weight and clothing: While weight loss from semaglutide may ultimately improve GERD, avoiding tight-fitting clothing around the abdomen reduces external pressure on the stomach.
Pharmacological management may be appropriate for persistent or bothersome symptoms. Over-the-counter antacids (calcium carbonate, magnesium hydroxide) provide rapid but short-term relief by neutralizing stomach acid. H2-receptor antagonists (famotidine) reduce acid production and can be used as needed or regularly. For more severe or persistent heartburn, proton pump inhibitors (PPIs) such as omeprazole or esomeprazole offer potent acid suppression. According to American College of Gastroenterology guidelines, an 8-week trial of daily PPI therapy is appropriate for typical GERD symptoms, with potential step-down therapy thereafter. Long-term PPI use requires medical supervision due to potential adverse effects.
Medication adjustments may also help. Slowing the semaglutide dose titration schedule or temporarily reducing the dose can improve tolerability. For Rybelsus (oral semaglutide), taking the medication exactly as directed—with no more than 4 ounces of plain water, at least 30 minutes before the first food, beverage, or other oral medications of the day, and remaining upright for at least 30 minutes—may help minimize GI effects.
Patients should discuss any additional medications with their healthcare provider to assess for drug interactions, as semaglutide's effect on gastric emptying may affect absorption of some medications.
While mild to moderate heartburn is a recognized and often manageable side effect of semaglutide, certain symptoms warrant prompt medical evaluation. Patients should be educated about warning signs that may indicate more serious complications or conditions requiring clinical assessment and potential treatment modification.
Contact your healthcare provider if you experience:
Severe or persistent heartburn that does not respond to over-the-counter medications or lifestyle modifications, or that significantly impacts quality of life and daily functioning
Difficulty swallowing (dysphagia) or painful swallowing (odynophagia), which may indicate esophageal inflammation, stricture, or other complications
Persistent nausea and vomiting that prevents adequate food or fluid intake, raising concerns about dehydration and nutritional status
Unintended weight loss beyond expected therapeutic effects, or inability to maintain adequate nutrition
Chest pain that is severe, persistent, or different from typical heartburn—call 911 immediately if you experience severe chest pain or symptoms suggestive of a heart attack
Signs of gastrointestinal bleeding, including vomiting blood or material resembling coffee grounds, black tarry stools, or blood in stool
Severe abdominal pain, particularly if localized to the upper abdomen and radiating to the back, which could indicate pancreatitis—a rare but serious adverse effect of GLP-1 receptor agonists
Right upper quadrant pain, fever, or yellowing of the skin or eyes, which could indicate gallbladder disease, a known potential complication of weight loss and GLP-1 receptor agonist therapy
According to American College of Gastroenterology guidelines, patients with alarm features or those whose symptoms persist despite an 8-week trial of daily PPI therapy should be referred for endoscopic evaluation. Healthcare providers may need to adjust the semaglutide dose, slow the titration schedule, or consider alternative therapeutic options if heartburn symptoms are severe or refractory to management strategies. The decision to continue, modify, or discontinue semaglutide should be individualized, weighing the cardiovascular and metabolic benefits of the medication against the impact of gastrointestinal side effects on patient well-being and treatment adherence.
Heartburn from semaglutide is typically most pronounced during the first few weeks of treatment and during dose escalation periods. For most patients, symptoms improve over time as the body adapts to the medication, though some individuals may experience persistent symptoms requiring ongoing management or dose adjustment.
Yes, antacids, H2-receptor antagonists, and proton pump inhibitors can generally be used safely with semaglutide to manage heartburn symptoms. However, you should discuss any additional medications with your healthcare provider, as semaglutide's effect on gastric emptying may affect the absorption of some oral medications.
No, not everyone experiences heartburn on semaglutide. Clinical trial data shows GERD symptoms occur in approximately 1.7–1.8% of patients taking Wegovy, while dyspepsia (including heartburn) affects 2.3–3.2% of patients. Individual risk factors such as pre-existing GERD, obesity, and hiatal hernia may increase susceptibility to reflux symptoms.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.