LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
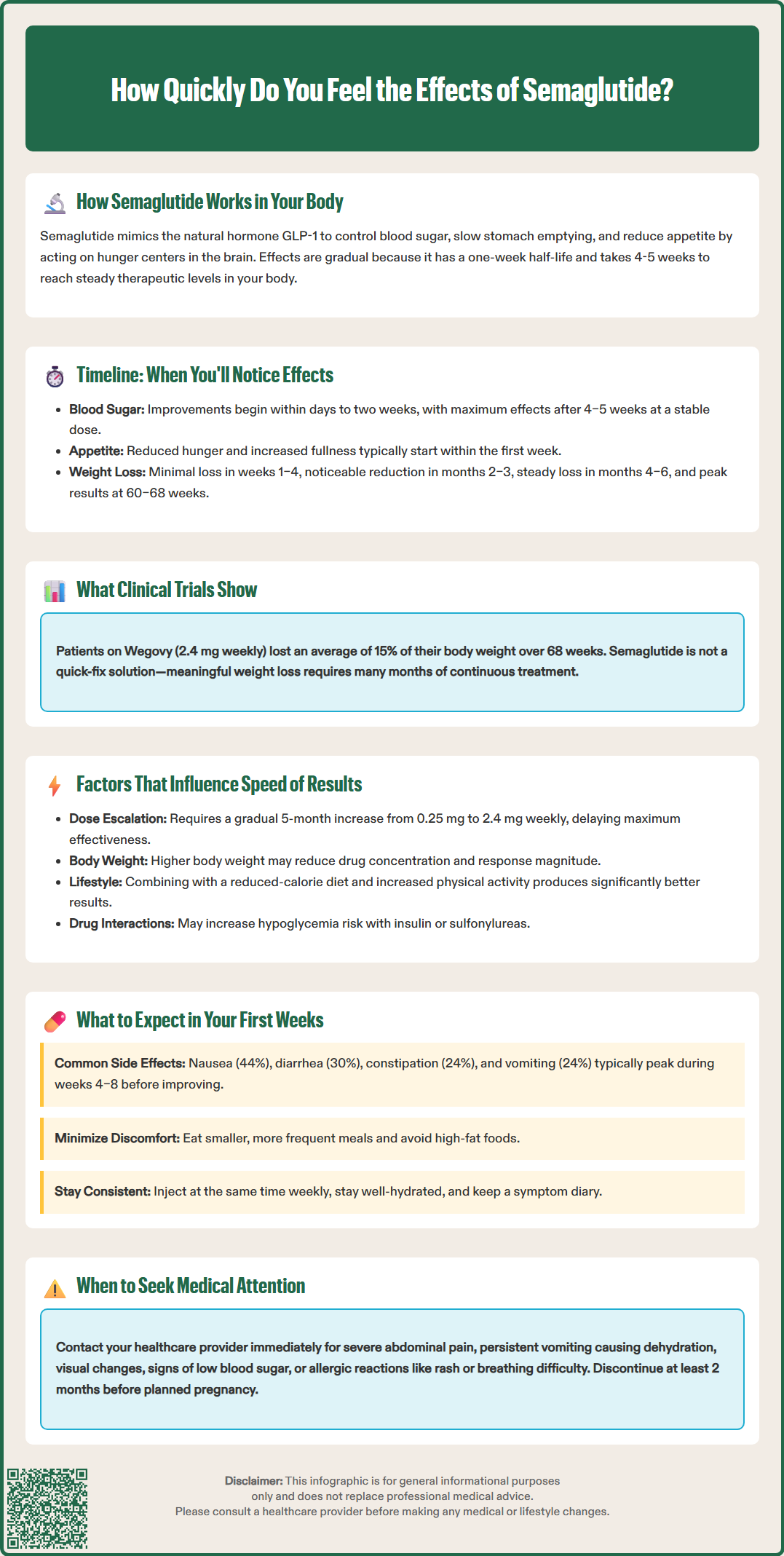
Semaglutide (Ozempic, Wegovy) doesn't work overnight—understanding the timeline helps set realistic expectations. Most patients notice reduced appetite within days to weeks, while blood sugar improvements typically begin within 1–2 weeks. However, maximum effects require 4–5 weeks to reach steady-state drug levels, and significant outcomes develop gradually over months. The medication's once-weekly dosing and slow titration schedule mean patience is essential. This article explains when you'll feel semaglutide's effects, what influences response timing, and what to expect during your first weeks of treatment.
Quick Answer: Most patients notice reduced appetite within days to weeks of starting semaglutide, while blood sugar improvements begin within 1–2 weeks, but maximum effects require 4–5 weeks to reach steady-state drug levels.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (under the brand name Ozempic) and chronic weight management (as Wegovy). Understanding its mechanism of action helps explain why effects occur gradually rather than immediately.
Mechanism of Action
Semaglutide mimics the naturally occurring hormone GLP-1, which your body releases after eating. Once administered, it binds to GLP-1 receptors throughout your body, triggering several physiological responses:
Pancreatic effects: Stimulates insulin secretion when blood glucose levels are elevated and suppresses glucagon release, helping to normalize blood sugar
Gastric effects: Slows gastric emptying, meaning food stays in your stomach longer, promoting feelings of fullness
Central nervous system effects: Acts on appetite centers in the brain to reduce hunger and food cravings
Cardiovascular benefits: Reduces the risk of major adverse cardiovascular events in adults with established cardiovascular disease and overweight/obesity (Wegovy) or type 2 diabetes (Ozempic)
The medication has a long half-life of approximately one week, which allows for once-weekly subcutaneous injection. This extended half-life means semaglutide accumulates gradually in your system over several weeks before reaching steady-state concentrations (typically 4-5 weeks). This pharmacokinetic profile is why you won't experience immediate effects—the medication needs time to build up to therapeutic levels and exert its full biological activity on multiple organ systems.
The timeline for experiencing semaglutide's effects varies depending on which outcomes you're monitoring. Clinical evidence provides clear guidance on what to expect and when.
Blood Sugar Effects (Days to Weeks)
For individuals with type 2 diabetes, blood glucose improvements typically begin within the first few days to two weeks of treatment. However, maximal glucose-lowering effects generally occur after 4–5 weeks at a stable dose, once steady-state drug levels are achieved. A1C reflects the prior ~3 months of glycemia; the American Diabetes Association recommends reassessing A1C about every 3 months after therapy changes.
Appetite and Satiety Changes (Days to Weeks)
Many patients report reduced appetite and increased feelings of fullness within the first week of treatment, though individual experiences vary considerably. These effects tend to become more pronounced as the dose is gradually increased. Some individuals notice changes after their first injection, while others require several weeks at therapeutic doses.
Weight Loss (Weeks to Months)
Weight reduction follows a more gradual trajectory. Clinical trials demonstrate:
Weeks 1–4: Minimal weight loss as your body adjusts
Months 2–3: More noticeable weight reduction as dose escalation continues
Months 4–6: Steady, consistent weight loss
Peak effect: Maximum weight loss typically occurs at 60–68 weeks of continuous treatment
According to FDA-approved labeling, patients on Wegovy (2.4 mg weekly) lost an average of 15% of their body weight over 68 weeks in clinical trials (STEP 1). Individual results vary significantly, with some people experiencing more or less weight loss than the average. It's important to understand that semaglutide is not a rapid weight-loss solution—results accumulate gradually over many months.
Multiple variables affect how quickly you'll experience semaglutide's effects, making individual responses somewhat unpredictable.
Dosing Schedule and Titration
Semaglutide requires gradual dose escalation to minimize gastrointestinal side effects. The standard titration schedule for Wegovy involves:
Month 1: 0.25 mg weekly
Month 2: 0.5 mg weekly
Month 3: 1.0 mg weekly
Month 4: 1.7 mg weekly
Month 5 onward: 2.4 mg weekly (maintenance dose)
This FDA-approved titration schedule means you won't reach therapeutic doses immediately, which delays the onset of maximal effects. Your healthcare provider may need to delay dose increases if you experience significant side effects, but should not accelerate the schedule beyond what's recommended in the FDA labeling.
Individual Metabolic Factors
Your baseline metabolic characteristics influence response:
Body weight and composition: Higher body weight results in lower drug concentrations at a given dose, potentially affecting response magnitude (though time to steady state remains ~4-5 weeks)
Insulin resistance severity: Those with more severe metabolic dysfunction may experience slower glucose improvements
Age: Age has no clinically meaningful effect on semaglutide pharmacokinetics
Kidney function: No dose adjustment is needed for renal impairment, as it doesn't significantly alter semaglutide pharmacokinetics
Lifestyle Factors
Semaglutide works most effectively when combined with lifestyle modifications. According to FDA labeling and clinical guidelines, semaglutide should be used with a reduced-calorie diet and increased physical activity. Patients who implement these dietary and activity changes typically experience more substantial results than those relying on medication alone.
Concurrent Medications
Because semaglutide slows gastric emptying, it may affect the absorption of some oral medications. Key considerations include:
Increased risk of hypoglycemia when used with insulin or sulfonylureas
Possible need for INR monitoring if taking warfarin
Limited clinically relevant effects on most other oral medications
Understanding what's normal during the initial treatment period helps set realistic expectations and identify situations requiring medical attention.
Common Early Experiences
During the first 4–8 weeks, most patients experience:
Gastrointestinal effects: Nausea is the most frequently reported side effect, affecting approximately 44% of patients in Wegovy clinical trials. This typically peaks during dose escalation and often improves with continued use. Other common GI symptoms include:
Diarrhea (approximately 30% of patients)
Constipation (24%)
Vomiting (24%)
Abdominal discomfort or bloating
Decreased appetite (which is therapeutic but can feel uncomfortable initially)
These effects are generally mild to moderate and resolve within several weeks as your body adjusts. Eating smaller, more frequent meals and avoiding high-fat foods can help minimize discomfort.
Subtle metabolic changes: You may notice reduced cravings for certain foods, particularly high-sugar or high-fat options. Some patients report feeling satisfied with smaller portions earlier than expected. These changes reflect semaglutide's effects on appetite regulation centers in your brain.
When to Contact Your Healthcare Provider
While most side effects are manageable, certain symptoms warrant immediate medical evaluation:
Severe, persistent abdominal pain (especially if radiating to your back)—may indicate pancreatitis
Right upper abdominal pain, fever, or yellowing of skin/eyes—may indicate gallbladder problems
Persistent vomiting leading to dehydration or decreased urination/swelling (possible acute kidney injury)
Visual changes or symptoms of diabetic retinopathy worsening
Signs of hypoglycemia if taking semaglutide with insulin or sulfonylureas (shakiness, confusion, rapid heartbeat)
Rash, swelling, or trouble breathing—may indicate hypersensitivity reaction
Symptoms of thyroid tumors (neck mass, difficulty swallowing, persistent hoarseness)—though extremely rare
Practical Management Tips
To optimize your early experience with semaglutide:
Inject at the same time each week for consistency
Stay well-hydrated, especially if experiencing GI symptoms
Monitor blood glucose if diabetic, as you may need adjustments to other diabetes medications
Keep a symptom diary to track patterns and discuss with your provider
Don't expect dramatic changes immediately—patience is essential for successful treatment
Important: If you're pregnant, planning pregnancy, or breastfeeding, discuss with your doctor. Semaglutide should be discontinued at least 2 months before a planned pregnancy and is not recommended during pregnancy or while breastfeeding.
Remember that semaglutide is a long-term therapy. The gradual onset of effects, while sometimes frustrating, reflects the medication's design to minimize side effects while maximizing sustainable metabolic benefits over time.
Many patients report reduced appetite and increased feelings of fullness within the first week of treatment, though individual experiences vary considerably. These effects tend to become more pronounced as the dose is gradually increased over subsequent months.
For individuals with type 2 diabetes, blood glucose improvements typically begin within the first few days to two weeks of treatment. However, maximal glucose-lowering effects generally occur after 4–5 weeks at a stable dose, once steady-state drug levels are achieved.
Semaglutide requires gradual dose escalation over 4–5 months to minimize gastrointestinal side effects like nausea, which affects approximately 44% of patients. The FDA-approved titration schedule allows your body to adjust while building up to the therapeutic maintenance dose of 2.4 mg weekly.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.