LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Many patients prescribed glucagon-like peptide-1 (GLP-1) receptor agonists for type 2 diabetes or weight management wonder whether these medications will be detected on routine blood work. GLP-1 drugs like semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda) do not appear on standard blood tests, drug screenings, or employment panels. While the medications themselves remain undetectable in routine laboratory work, their therapeutic effects—including improved hemoglobin A1c, fasting glucose, and lipid profiles—are clearly measurable. Understanding what blood tests monitor during GLP-1 therapy helps patients navigate treatment confidently and communicate effectively with their healthcare providers.
Quick Answer: GLP-1 receptor agonist medications do not appear on standard blood tests, drug screenings, or employment panels.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily used to manage type 2 diabetes and, more recently, for chronic weight management in adults with obesity or overweight with weight-related comorbidities. These medications include semaglutide (Ozempic, Wegovy, Rybelsus), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), and others. Tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 receptor agonist that works through similar mechanisms.
GLP-1 medications work by mimicking the action of naturally occurring GLP-1, an incretin hormone released by the intestines in response to food intake. These drugs bind to GLP-1 receptors on pancreatic beta cells, stimulating glucose-dependent insulin secretion—meaning they promote insulin release only when blood glucose levels are elevated. This mechanism reduces the risk of hypoglycemia when used alone, though this risk increases when combined with insulin or sulfonylureas. Additionally, these medications suppress glucagon secretion from pancreatic alpha cells, which helps prevent excessive glucose production by the liver.
Beyond glycemic control, GLP-1 medications slow gastric emptying, which prolongs the feeling of fullness after meals and contributes to reduced caloric intake. They also act on appetite centers in the brain, particularly the hypothalamus, to decrease hunger and food cravings. These combined effects make these medications effective for both blood sugar management and weight loss.
Most GLP-1 medications are administered via subcutaneous injection, either daily or weekly depending on the specific formulation. Oral semaglutide (Rybelsus) is also available. Common adverse effects include nausea, vomiting, diarrhea, and constipation, which typically improve over time. Important safety considerations include boxed warnings for thyroid C-cell tumors (based on animal studies), and cautions regarding pancreatitis and gallbladder disease. These medications are not indicated for type 1 diabetes.
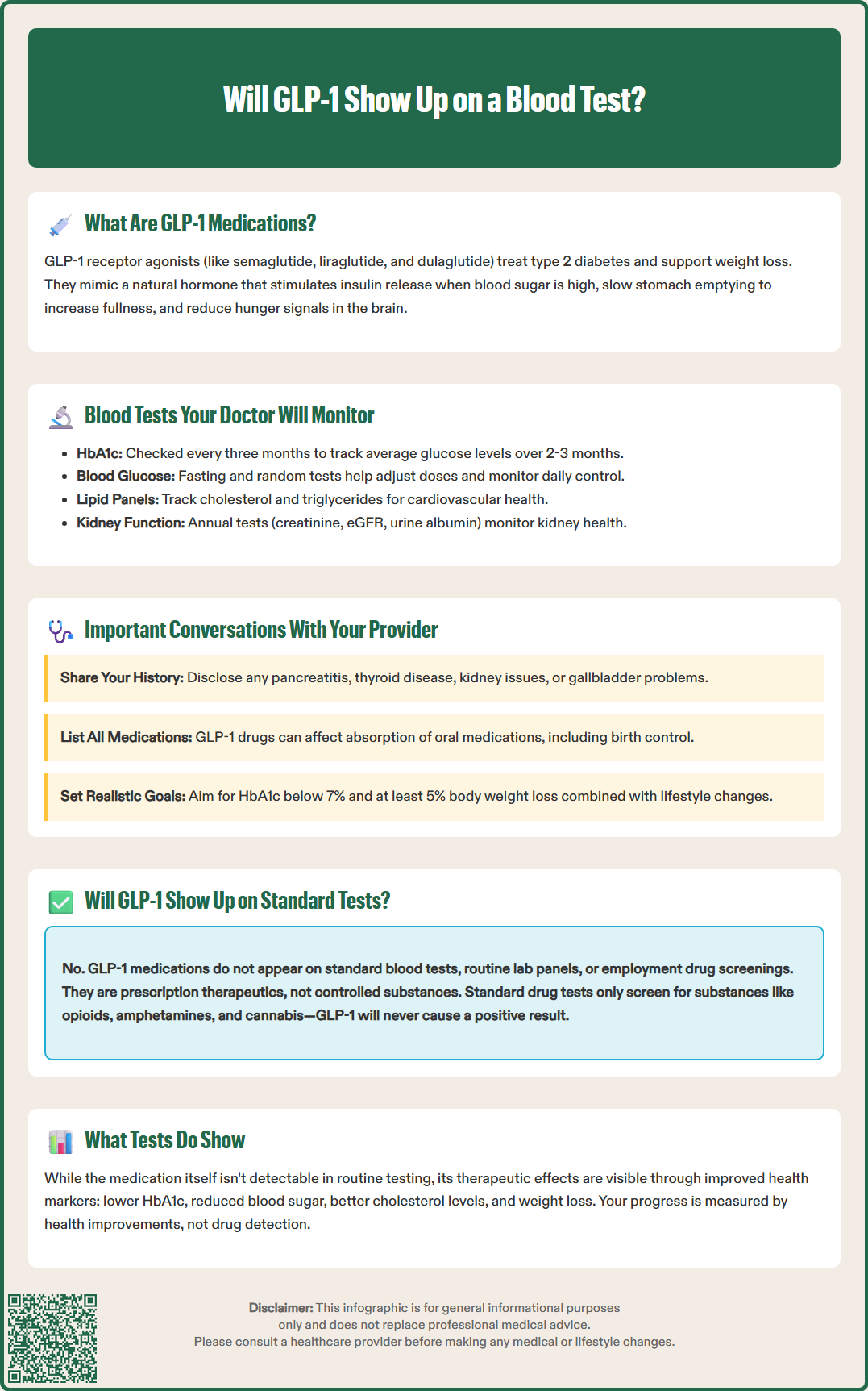
When patients take GLP-1 receptor agonists, healthcare providers typically monitor several blood parameters to assess treatment efficacy and safety, though none of these tests directly measure the GLP-1 medication itself. The most important marker is hemoglobin A1c (HbA1c), which reflects average blood glucose levels over the preceding two to three months. For patients with type 2 diabetes, the American Diabetes Association recommends checking HbA1c every three months until glycemic targets are achieved, then at least twice yearly thereafter.
Fasting blood glucose and random glucose measurements provide additional information about day-to-day glycemic control. These tests help clinicians adjust medication dosages and identify patterns that may require intervention. Patients using GLP-1 medications for diabetes management should expect regular glucose monitoring as part of routine care.
Lipid panels are also relevant, as GLP-1-based therapies may modestly improve cardiovascular risk factors. Some studies have shown small reductions in total cholesterol, LDL cholesterol, and triglycerides in certain patients, though these medications are not substitutes for statins when lipid-lowering therapy is indicated. Monitoring lipid levels helps assess overall cardiovascular health, particularly important given that many patients with type 2 diabetes have concurrent dyslipidemia.
Kidney function tests, including serum creatinine, estimated glomerular filtration rate (eGFR), and urine albumin-to-creatinine ratio (UACR), warrant attention. The UACR should be checked at least annually, or more frequently in patients with chronic kidney disease. Some GLP-1 medications have demonstrated renal protective effects in clinical trials, though evidence varies by specific agent. Liver function tests may be monitored in patients with pre-existing liver conditions. While pancreatic enzymes (lipase, amylase) are not routinely monitored, they might be checked if pancreatitis is suspected based on symptoms. Patients with diabetic retinopathy may need appropriate eye follow-up, especially with rapid improvement in glucose control.
Open communication with your healthcare provider about GLP-1 medication use is essential for safe and effective treatment. Before starting therapy, discuss your complete medical history, including any history of pancreatitis, thyroid disease (particularly medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2), diabetic retinopathy, kidney disease, gallbladder disease, or gastrointestinal disorders. GLP-1 receptor agonists carry a boxed warning regarding thyroid C-cell tumors observed in animal studies, and while the relevance to humans remains uncertain, patients with personal or family history of medullary thyroid carcinoma should not use these medications.
Inform your provider about all medications and supplements you take. Some GLP-1 medications can affect the absorption of oral medications due to delayed gastric emptying. This is particularly important with tirzepatide, which can reduce oral contraceptive exposure during initiation and dose escalation, potentially requiring backup contraception. Your provider may need to adjust dosing schedules or consider alternative formulations for certain medications.
Discuss realistic treatment goals and expectations. For diabetes management, the target HbA1c is typically below 7% for most adults, though individualized targets may be appropriate based on age, comorbidities, and hypoglycemia risk. For weight management, clinically meaningful weight loss is generally defined as 5% or more of initial body weight. Understanding that GLP-1 medications work best when combined with lifestyle modifications—including dietary changes and increased physical activity—is crucial for optimal outcomes.
If you're using insulin or sulfonylureas with GLP-1 medications, discuss hypoglycemia prevention and recognition, as dose adjustments of these medications may be needed. For women of childbearing potential, note that GLP-1 medications for weight management are contraindicated during pregnancy, and some agents should be discontinued at least two months before planned conception.
Report any concerning symptoms promptly, including severe abdominal pain (which may indicate pancreatitis), right upper quadrant pain (possible gallbladder issues), persistent nausea or vomiting leading to dehydration, changes in vision, symptoms of thyroid nodules (neck mass, difficulty swallowing), or signs of kidney problems (decreased urination, swelling). Regular follow-up appointments allow your provider to monitor treatment response, adjust dosages as needed, and address any adverse effects.
GLP-1 receptor agonist medications do not appear on standard blood tests ordered in routine clinical practice or employment screenings. These drugs are peptide-based therapeutic agents, not substances typically screened for in conventional laboratory panels. Standard blood work—including complete blood counts, comprehensive metabolic panels, lipid profiles, or HbA1c measurements—assesses various health markers and metabolic parameters but does not identify or quantify GLP-1 medications in the bloodstream.
Drug screening tests, whether for employment, legal, or medical purposes, focus on detecting substances of abuse such as opioids, amphetamines, benzodiazepines, cannabis, and cocaine. GLP-1 medications are prescription therapeutics that are not controlled substances and are not included in standard drug screening panels, including those outlined in the Substance Abuse and Mental Health Services Administration (SAMHSA) guidelines for federal workplace drug testing. There is no link between GLP-1 use and positive results on employment or legal drug tests.
Specialized assays can measure endogenous GLP-1 levels or detect synthetic GLP-1 analogs, but these tests are used exclusively in research settings or highly specialized clinical scenarios—not in routine medical care. Such testing requires specific laboratory techniques and is not part of standard clinical practice. Healthcare providers do not routinely measure circulating levels of GLP-1 medications because dosing is standardized based on clinical response (glycemic control, weight loss, tolerability) rather than blood concentrations.
Patients should understand that while the medication itself won't show up on blood tests, the therapeutic effects of GLP-1 drugs are clearly evident through improved metabolic markers: lower HbA1c, reduced fasting glucose, potential improvements in lipid profiles, and weight loss. These changes reflect successful treatment and are the intended outcomes healthcare providers monitor. If you have concerns about medication detection for employment, insurance, or other purposes, discuss them openly with your healthcare provider. GLP-1-based therapies are legitimate prescription medications for approved medical conditions, and their use is protected health information under HIPAA regulations in the United States.
No, GLP-1 medications are not controlled substances and do not appear on standard employment drug screenings, which test for substances of abuse like opioids, amphetamines, and cannabis.
Healthcare providers typically monitor hemoglobin A1c, fasting blood glucose, lipid panels, kidney function tests (creatinine, eGFR, UACR), and liver function tests to assess treatment efficacy and safety.
Specialized laboratory assays can detect synthetic GLP-1 analogs, but these tests are used exclusively in research settings and are not part of routine clinical practice or standard medical care.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.