LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide, marketed as Mounjaro for type 2 diabetes and Zepbound for weight management, is a dual GIP and GLP-1 receptor agonist that has transformed metabolic disease treatment. While generally well-tolerated, allergic reactions to tirzepatide can occur, ranging from mild injection site reactions to serious systemic hypersensitivity including anaphylaxis and angioedema. The FDA prescribing information identifies serious hypersensitivity as a contraindication to continued use. Understanding the signs, risk factors, and appropriate responses to allergic reactions is essential for healthcare providers and patients to ensure safe medication use and optimal therapeutic outcomes.
Quick Answer: Allergic reactions to tirzepatide range from mild local injection site reactions to serious systemic hypersensitivity including anaphylaxis and angioedema, which are contraindications to continued use.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus (marketed as Mounjaro) and chronic weight management (marketed as Zepbound). As a dual incretin mimetic, tirzepatide has demonstrated significant effects on glycemic control and weight reduction in clinical trials.
The medication works through a dual mechanism of action. By activating GIP receptors, tirzepatide enhances insulin secretion and has been associated with improved insulin sensitivity in preclinical studies. Simultaneously, GLP-1 receptor activation stimulates glucose-dependent insulin release from pancreatic beta cells, suppresses inappropriate glucagon secretion, slows gastric emptying, and promotes satiety through central nervous system pathways. This combined approach results in improved postprandial and fasting glucose levels, reduced hemoglobin A1c, and clinically meaningful weight loss.
Tirzepatide is administered as a once-weekly subcutaneous injection, with doses ranging from 2.5 mg to 15 mg depending on the indication and individual patient response. The medication is a synthetic peptide consisting of 39 amino acids with a C20 fatty diacid moiety that enables albumin binding and prolongs the half-life to approximately 5 days. Common adverse effects include gastrointestinal symptoms such as nausea, vomiting, and diarrhea, which typically diminish with continued use. According to FDA prescribing information, serious hypersensitivity reactions, including anaphylaxis and angioedema, have been reported in patients treated with tirzepatide. A history of serious hypersensitivity to tirzepatide or any of its excipients is a contraindication to its use.
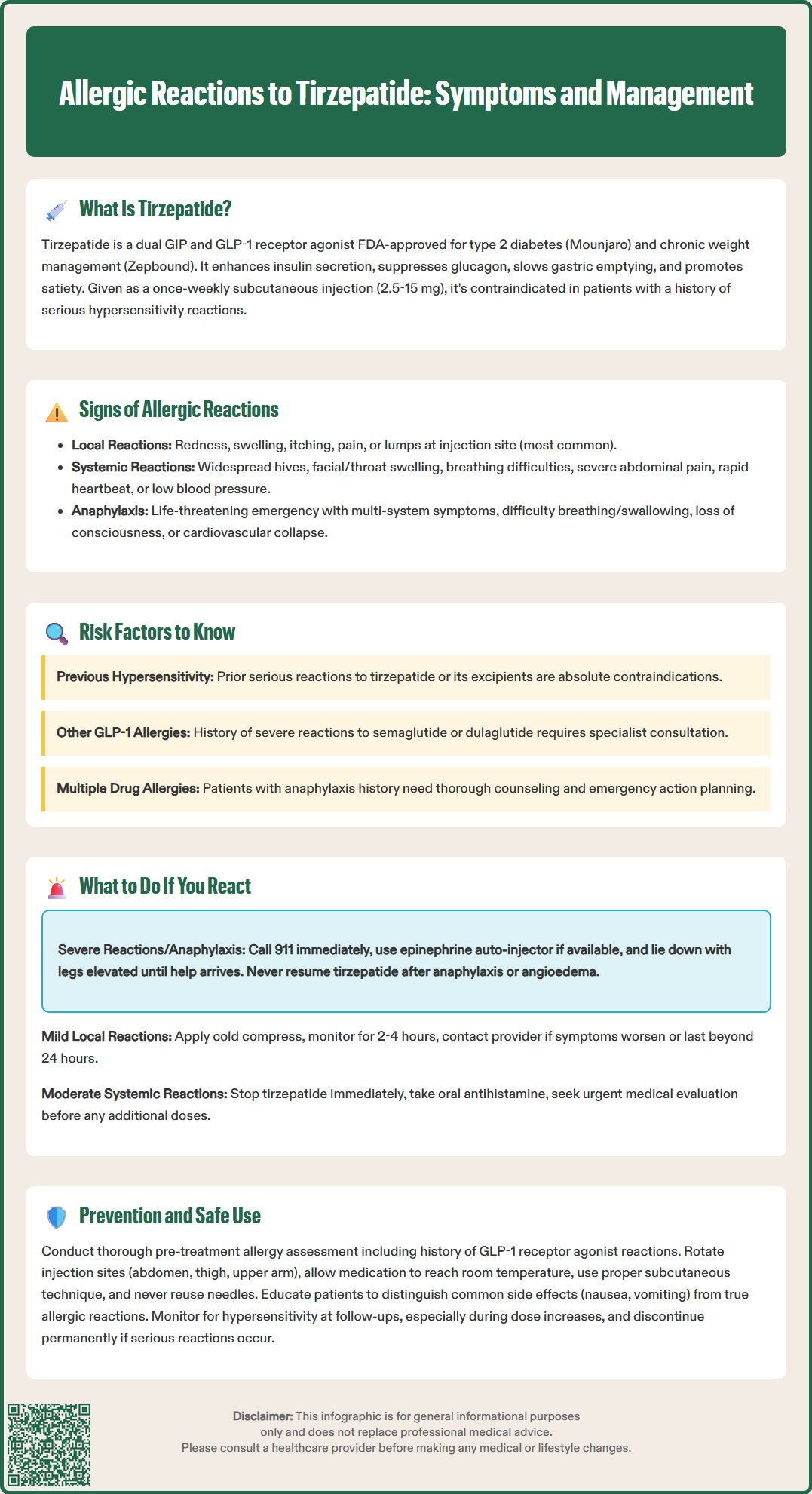
Allergic reactions to tirzepatide can range from mild local reactions to severe systemic hypersensitivity. According to FDA prescribing information, serious hypersensitivity reactions including anaphylaxis and angioedema have been reported in patients treated with tirzepatide, though the overall incidence remains low. Healthcare providers and patients must be able to recognize the spectrum of allergic manifestations to ensure timely intervention.
Local injection site reactions are the most common form of hypersensitivity and may include:
Erythema, swelling, or induration at the injection site
Pruritus or burning sensation localized to the area
Persistent pain or tenderness beyond typical injection discomfort
Development of nodules or persistent lumps
These reactions typically occur within hours to days of injection and may resolve spontaneously, though persistent or worsening symptoms warrant medical evaluation.
Systemic allergic reactions are more concerning and require immediate medical attention. Signs and symptoms include:
Generalized urticaria (hives) or widespread pruritic rash
Angioedema affecting the face, lips, tongue, or throat
Respiratory symptoms including wheezing, dyspnea, or throat tightness
Gastrointestinal symptoms such as severe abdominal cramping, nausea, or vomiting (distinct from common GI side effects)
Cardiovascular manifestations including tachycardia, hypotension, or dizziness
Anaphylaxis represents the most severe form of allergic reaction and constitutes a medical emergency. Warning signs include rapid onset of symptoms affecting multiple organ systems, difficulty breathing or swallowing, sense of impending doom, loss of consciousness, or cardiovascular collapse. Any patient experiencing symptoms suggestive of anaphylaxis requires immediate emergency medical services activation and epinephrine administration. After anaphylaxis or angioedema, tirzepatide should be permanently discontinued. It is important to distinguish true allergic reactions from common medication side effects, as gastrointestinal symptoms are expected with tirzepatide therapy and do not typically indicate allergy unless accompanied by other hypersensitivity features.
While allergic reactions to tirzepatide are uncommon, certain patient characteristics and clinical factors may increase susceptibility. Understanding these risk factors enables clinicians to identify potentially vulnerable individuals and implement appropriate monitoring strategies.
Previous allergic history represents an important consideration. A history of serious hypersensitivity to tirzepatide or its excipients is a contraindication to its use, as stated in the FDA prescribing information. For patients with documented hypersensitivity to other GLP-1 receptor agonists (such as semaglutide, dulaglutide, or liraglutide), cross-reactivity is uncertain due to differences in molecular structure. Each case requires individual assessment, and consultation with an allergy specialist may be warranted for patients with prior severe reactions to related medications. Additionally, patients with multiple drug allergies or a personal history of anaphylaxis to any substance should be counseled about recognizing allergic symptoms.
Atopic conditions such as asthma, allergic rhinitis, atopic dermatitis, or food allergies are common in the general population. While these conditions do not contraindicate tirzepatide use and are not specifically identified as risk factors in the FDA label, patients with these conditions should receive thorough education about recognizing allergic symptoms.
Excipient sensitivity should be considered, though reactions to the inactive ingredients in tirzepatide are rare. According to the FDA prescribing information, tirzepatide formulations contain sodium phosphate, sodium chloride, and water for injection, with pH adjusters as needed. Patients with known sensitivities to these components should be evaluated before initiating therapy.
It is important to note that having potential risk factors does not preclude tirzepatide use, but rather indicates the need for patient education, appropriate monitoring during treatment initiation, and readily available emergency management resources. Clinicians should document allergic history thoroughly and discuss emergency action plans with patients before prescribing tirzepatide.
Prompt recognition and appropriate response to allergic reactions are critical for patient safety. The management approach depends on reaction severity, and both patients and healthcare providers must understand the appropriate steps for different scenarios.
For mild local reactions limited to the injection site without systemic symptoms:
Discontinue the injection if still in progress
Apply a cold compress to reduce swelling and discomfort
Avoid rubbing or massaging the affected area
Monitor for progression over the next 2-4 hours
Contact your healthcare provider if symptoms worsen or persist beyond 24 hours
Document the reaction, including timing, appearance, and duration
Mild local reactions may not require treatment discontinuation, but medical evaluation is necessary to determine whether subsequent doses are safe.
For moderate systemic reactions such as generalized hives, mild angioedema without airway involvement, or widespread itching:
Stop using tirzepatide immediately
Take an oral antihistamine if available and not contraindicated (such as diphenhydramine 25-50 mg, noting it may cause sedation and impair driving, or non-sedating options like cetirizine or loratadine for milder symptoms)
Contact your healthcare provider or seek urgent care evaluation
Do not administer additional doses until evaluated by a physician
Monitor closely for progression to more severe symptoms
For severe reactions or suspected anaphylaxis, immediate emergency action is required:
Call 911 immediately — do not delay or attempt to drive yourself
If you have an epinephrine auto-injector, use it immediately into the outer thigh
Lie down with legs elevated (unless breathing is difficult, then sit upright)
If symptoms do not improve or worsen after 5-10 minutes, administer a second epinephrine dose if available
Remain with the patient until emergency services arrive
All patients treated for anaphylaxis should be transported to the emergency department for observation due to the risk of biphasic reactions
After any allergic reaction, patients should not resume tirzepatide without explicit guidance from their healthcare provider. Serious hypersensitivity reactions, including anaphylaxis or angioedema, are contraindications to further tirzepatide use. Suspected adverse reactions should be reported to the FDA MedWatch program (www.fda.gov/medwatch or 1-800-FDA-1088). Medical evaluation should include documentation of the reaction, assessment of alternative treatment options, and consideration of allergy specialist referral if the diagnosis is uncertain.
Minimizing the risk of allergic reactions requires a comprehensive approach encompassing careful patient selection, proper administration technique, and ongoing monitoring. Healthcare providers and patients share responsibility for ensuring safe medication use.
Pre-treatment assessment is essential before initiating tirzepatide. Clinicians should obtain a detailed allergy history, including previous reactions to GLP-1 receptor agonists, other injectable medications, and any history of anaphylaxis. The FDA label does not require routine allergy testing before starting tirzepatide, but individual risk assessment should guide clinical decision-making. Patients with a history of serious hypersensitivity to tirzepatide or its excipients should not receive the medication, as this is a contraindication per the FDA prescribing information.
Proper injection technique can reduce local reactions:
Rotate injection sites among the abdomen, thigh, and upper arm to prevent localized sensitization
Allow the medication to reach room temperature before injection (according to the Instructions for Use)
Use proper subcutaneous technique with appropriate needle angle
Avoid injecting into areas with skin abnormalities, scars, or previous reaction sites
Do not reuse needles or share pens between patients
Note that upper arm injections may require administration by another person
Patient education forms the cornerstone of safe use. Before prescribing tirzepatide, ensure patients understand:
The difference between expected side effects (nausea, GI symptoms) and allergic reactions
Warning signs requiring immediate medical attention
The importance of having emergency contact information readily available
Proper injection technique according to the device Instructions for Use
Ongoing monitoring should include assessment for hypersensitivity symptoms at follow-up visits, particularly during dose escalation. Patients should be instructed to report any unusual symptoms promptly. Serious hypersensitivity reactions, including anaphylaxis or angioedema, are contraindications to further tirzepatide use.
Alternative treatment options should be discussed with patients who experience confirmed allergic reactions. Other diabetes medications or weight management strategies may be appropriate depending on individual clinical circumstances. Consultation with endocrinology or allergy specialists can help optimize therapeutic approaches while maintaining patient safety. Suspected adverse reactions should be reported to the FDA MedWatch program.
Allergic reactions range from local injection site reactions (erythema, swelling, pruritus) to serious systemic symptoms including generalized urticaria, angioedema affecting the face or throat, respiratory difficulty, and anaphylaxis with cardiovascular collapse. Severe reactions require immediate emergency medical attention and epinephrine administration.
Serious hypersensitivity reactions including anaphylaxis or angioedema are contraindications to further tirzepatide use per FDA prescribing information. Mild local reactions may not require discontinuation, but medical evaluation is necessary to determine whether subsequent doses are safe.
Patients with a history of serious hypersensitivity to tirzepatide or its excipients should not use the medication. Those with previous allergic reactions to other GLP-1 receptor agonists, multiple drug allergies, or a history of anaphylaxis to any substance require careful assessment and thorough education about recognizing allergic symptoms.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.