LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does tirzepatide make you throw up? Yes, tirzepatide (Mounjaro, Zepbound) can cause nausea and vomiting, which are among the most common side effects of this dual GIP and GLP-1 receptor agonist. Approved by the FDA for type 2 diabetes and chronic weight management, tirzepatide slows gastric emptying and stimulates receptors in the brainstem that trigger nausea. While these gastrointestinal effects are dose-dependent and typically occur during initial treatment or dose escalation, most patients find symptoms diminish over time. Understanding how to manage and when to seek medical attention for these side effects is essential for successful treatment.
Quick Answer: Tirzepatide can cause nausea and vomiting in 12–31% of patients, with symptoms typically occurring during initial treatment or dose increases and generally diminishing over time.
Tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved for type 2 diabetes management and chronic weight management. Yes, tirzepatide can cause nausea and vomiting, and these are among the most frequently reported gastrointestinal side effects associated with this medication.
The mechanism underlying these adverse effects relates primarily to tirzepatide's GLP-1 receptor activity. As a GLP-1 receptor agonist, tirzepatide slows gastric emptying—the rate at which food moves from the stomach into the small intestine. This delayed emptying contributes to increased satiety and reduced appetite, which supports weight loss, but it also creates a sensation of fullness that can trigger nausea. Additionally, GLP-1 receptors are present in the brainstem area postrema, a region involved in the vomiting reflex, and direct stimulation of these receptors may contribute to nausea and emesis.
According to the FDA prescribing information, gastrointestinal adverse reactions are dose-dependent and typically occur during dose escalation. Most patients experience these symptoms during the initial weeks of treatment or following dose increases. The intensity and frequency generally diminish over time as the body adapts to the medication, with gastric emptying effects showing tachyphylaxis (diminishing response) over time. Other common gastrointestinal side effects include diarrhea, constipation, and dyspepsia. Understanding that nausea and vomiting are common, mechanism-based side effects can help patients and clinicians anticipate and manage these symptoms proactively.
Clinical trial data provide clear insight into the incidence of nausea and vomiting with tirzepatide. In the pivotal SURPASS trials evaluating tirzepatide for type 2 diabetes, nausea occurred in 12–22% of patients depending on the dose (5 mg, 10 mg, or 15 mg weekly), compared to approximately 5–8% with placebo. Vomiting was reported in 5–10% of tirzepatide-treated patients, versus 1–3% with placebo. The SURMOUNT-1 trial, which assessed tirzepatide for weight management, showed higher rates, with nausea affecting approximately 31% of participants at the 15 mg dose.
These gastrointestinal side effects demonstrate a clear dose-response relationship. Higher doses of tirzepatide are generally associated with increased rates of nausea and vomiting, though rates vary by indication (type 2 diabetes vs. obesity) and individual trial design. The 15 mg weekly dose typically showed the highest incidence of gastrointestinal effects across studies. Importantly, most cases were classified as mild to moderate in severity, and the majority resolved within several weeks without intervention.
Discontinuation rates due to gastrointestinal adverse effects ranged from 4–7% across clinical trials, as reported in the FDA prescribing information, indicating that while nausea and vomiting are common, they are tolerable for most patients. The gradual dose escalation schedule recommended in the prescribing information—starting at 2.5 mg weekly and increasing every four weeks—was specifically designed to minimize these effects. Patients who experience gastrointestinal symptoms should be reassured that these reactions are common, generally temporary, and manageable with appropriate strategies.
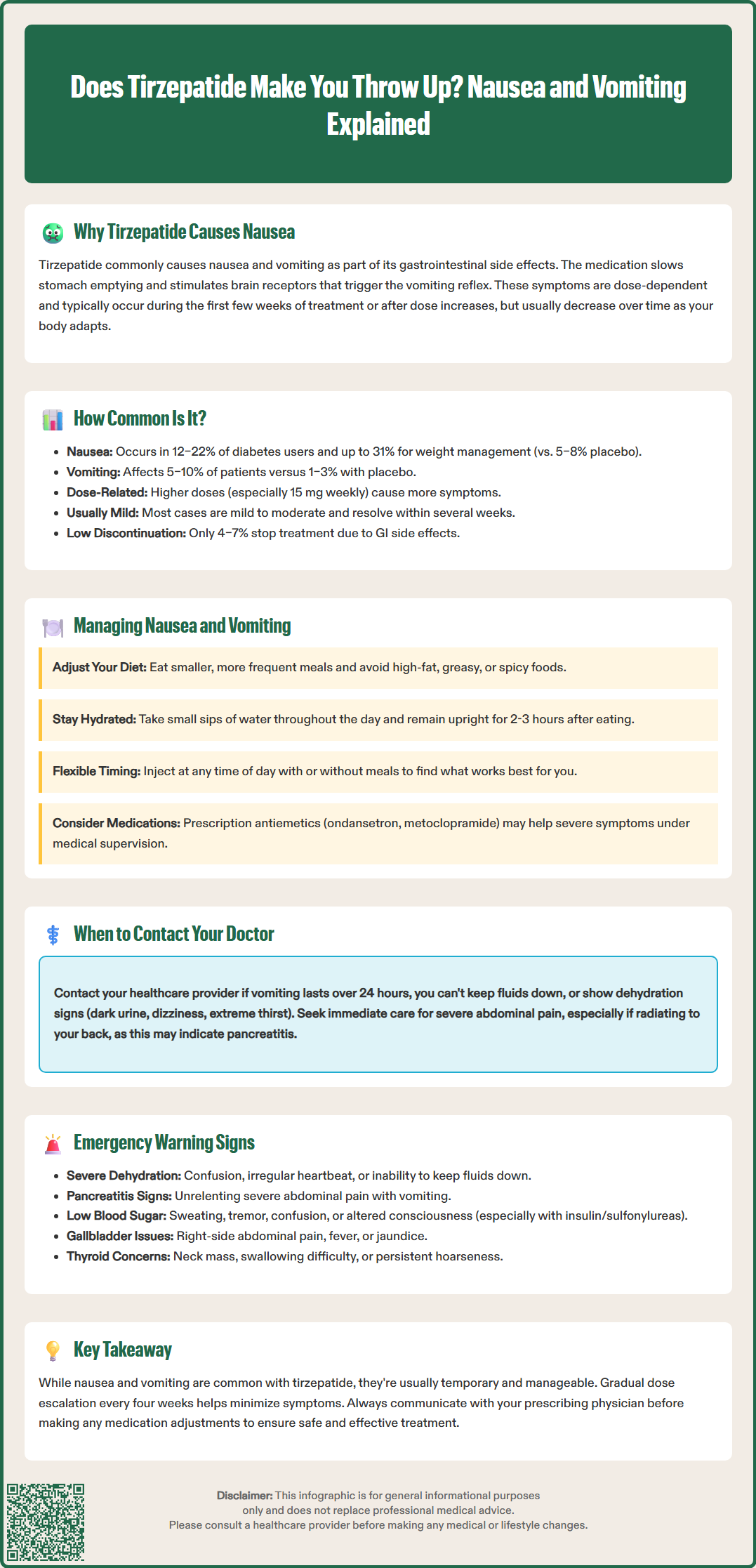
Effective management of nausea and vomiting can significantly improve treatment adherence and patient quality of life. Dietary modifications represent the first-line approach. Patients should be advised to:
Eat smaller, more frequent meals rather than large portions, which can overwhelm delayed gastric emptying
Avoid high-fat, greasy, or spicy foods that are more difficult to digest and may exacerbate nausea
Stay well-hydrated with small sips of water throughout the day, particularly important if vomiting occurs
Eat slowly and chew thoroughly to facilitate digestion
Avoid lying down immediately after eating; remaining upright for 2–3 hours post-meal can reduce reflux and nausea
Timing considerations can also help. Some patients anecdotally report that administering tirzepatide at bedtime reduces daytime nausea, though this strategy is not evidence-based and should be individualized. The injection can be given at any time of day, with or without meals, providing flexibility to optimize tolerability.
If dietary measures prove insufficient, pharmacological interventions may be appropriate. Over-the-counter options include ginger supplements or vitamin B6, though evidence for their efficacy is limited and these supplements are not FDA-approved for this use and may interact with medications or be inappropriate during pregnancy. For more severe symptoms, clinicians may consider prescribing antiemetics such as ondansetron (4–8 mg as needed; caution with QT prolongation risk), metoclopramide (10 mg before meals; boxed warning for tardive dyskinesia with use >12 weeks), or prochlorperazine (risk of extrapyramidal symptoms and sedation). These medications should only be used under healthcare provider supervision.
Dose adjustment represents another management strategy. If nausea or vomiting is severe or persistent, temporarily maintaining the current dose for an additional 4 weeks before escalating, or even reducing to the previous tolerated dose, may be warranted—but any dose modifications must be directed by the prescribing healthcare provider. The American Diabetes Association Standards of Care emphasize individualized dose titration based on tolerability and glycemic response. Communication with the prescribing physician is essential before making any dose modifications.
While mild nausea is common and generally manageable, certain symptoms warrant prompt medical evaluation. Patients should contact their healthcare provider if they experience:
Persistent vomiting lasting more than 24 hours or inability to keep down fluids, which raises concern for dehydration
Signs of dehydration including decreased urination, dark urine, dizziness upon standing, extreme thirst, or dry mouth
Severe abdominal pain, particularly if constant and radiating to the back, which may indicate pancreatitis—a rare but serious adverse effect
Hypoglycemia symptoms including sweating, tremor, palpitations, confusion, dizziness, or irritability—especially in patients taking concurrent insulin or sulfonylureas
Right upper quadrant pain, fever, or jaundice which may indicate gallbladder disease, a reported adverse effect with tirzepatide
Symptoms interfering with daily activities or causing significant distress despite conservative management
Immediate emergency care is warranted for:
Severe, unrelenting abdominal pain with vomiting
Signs of acute pancreatitis (severe epigastric pain radiating to the back, fever, rapid pulse)
Symptoms of severe dehydration or electrolyte imbalance (confusion, irregular heartbeat, muscle weakness)
Suspected hypoglycemia with altered consciousness
The FDA prescribing information specifically warns about the risk of acute kidney injury secondary to dehydration from gastrointestinal adverse effects. Patients with pre-existing renal impairment require particularly careful monitoring. Additionally, tirzepatide carries a boxed warning regarding thyroid C-cell tumors observed in rodent studies; tirzepatide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Patients should report any neck mass, dysphagia, or persistent hoarseness.
Tirzepatide is not recommended in patients with severe gastrointestinal disease, including severe gastroparesis. If pancreatitis is suspected, tirzepatide should be discontinued pending evaluation. Clinicians should maintain a low threshold for evaluating persistent gastrointestinal symptoms, as distinguishing medication side effects from other acute conditions requires clinical judgment. Shared decision-making regarding continuation, dose adjustment, or discontinuation of tirzepatide should incorporate patient preferences, therapeutic goals, and overall risk-benefit assessment.
Nausea from tirzepatide typically occurs during the first few weeks of treatment or after dose increases and generally diminishes within several weeks as the body adapts to the medication. Most cases are mild to moderate and resolve without intervention.
Yes, healthcare providers may prescribe antiemetics such as ondansetron, metoclopramide, or prochlorperazine for severe nausea with tirzepatide, but these medications should only be used under medical supervision due to potential side effects and drug interactions.
Do not stop tirzepatide without consulting your healthcare provider. Contact your doctor if vomiting persists beyond 24 hours, you cannot keep down fluids, or you experience signs of dehydration, as dose adjustment or temporary discontinuation may be necessary.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.