LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide, marketed as Mounjaro for type 2 diabetes and Zepbound for chronic weight management, is administered as a once-weekly subcutaneous injection. Understanding the proper areas to inject tirzepatide is essential for optimal drug absorption, treatment effectiveness, and minimizing injection-related complications. The FDA-approved prescribing information specifies three anatomical sites for tirzepatide administration: the abdomen, thigh, and upper arm. Proper site selection and systematic rotation between these areas help prevent tissue changes that can impair medication absorption and ensure consistent therapeutic outcomes. This guide provides comprehensive information on FDA-approved injection sites, proper technique, and best practices for safe tirzepatide administration.
Quick Answer: Tirzepatide should be injected subcutaneously in one of three FDA-approved areas: the abdomen (at least two inches from the navel), the front of the thigh (middle third between hip and knee), or the back of the upper arm (with caregiver assistance).
Tirzepatide is a glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus under the brand name Mounjaro and for chronic weight management in adults with obesity or overweight with weight-related comorbidities under the brand name Zepbound. Tirzepatide is not indicated for patients with type 1 diabetes.
IMPORTANT SAFETY INFORMATION: Tirzepatide has a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
The medication works through activation of both GIP and GLP-1 receptors, which are incretin hormones naturally produced in the gastrointestinal tract. GLP-1 receptor activation enhances glucose-dependent insulin secretion from pancreatic beta cells, suppresses glucagon secretion, and slows gastric emptying. These effects collectively improve glycemic control while reducing appetite and food intake. The GIP component may further contribute to the glucose-lowering effects, though the precise mechanisms in humans continue to be studied.
Tirzepatide is administered as a once-weekly subcutaneous injection, with dosing typically initiated at 2.5 mg for treatment initiation (not intended for glycemic control). For Mounjaro, dosing is gradually titrated based on glycemic response and tolerability, with maximum doses reaching 15 mg weekly. For Zepbound, the maximum dose is 15 mg weekly, with a similar titration schedule. The extended half-life allows for weekly dosing, which may improve adherence compared to daily therapies.
In clinical trials, tirzepatide demonstrated significant reductions in hemoglobin A1c levels in patients with type 2 diabetes. Weight loss effects varied by population, with patients with obesity without diabetes (SURMOUNT-1 trial) showing greater reductions than those with type 2 diabetes. Common adverse effects include gastrointestinal symptoms such as nausea, diarrhea, vomiting, and constipation, which are typically mild to moderate and often diminish over time.
Additional important safety considerations include risks of pancreatitis, gallbladder disease, acute kidney injury from dehydration, hypoglycemia (when used with insulin or sulfonylureas), and potential effects on diabetic retinopathy. Tirzepatide may reduce the effectiveness of oral contraceptives, requiring use of an additional contraceptive method for 4 weeks after initiation and after each dose increase.
The FDA-approved prescribing information for tirzepatide specifies three anatomical areas suitable for subcutaneous injection: the abdomen, thigh, and upper arm. These sites have been selected based on clinical trial data demonstrating consistent drug absorption, patient tolerability, and safety profiles. Healthcare providers should educate patients on proper site selection to optimize therapeutic outcomes and minimize injection-related complications.
Abdomen: The abdominal area is often the preferred injection site for many patients due to ease of access and consistent subcutaneous tissue depth. Injections should be administered at least two inches away from the navel (umbilicus) to avoid areas with increased vascularity and potential discomfort. The entire abdominal region, excluding the area immediately surrounding the belly button, provides ample surface area for site rotation. Patients should avoid injecting into areas with scars, stretch marks, or visible blood vessels, as well as skin that is tender, bruised, scaly, or hard.
Thigh: The front of the thigh, specifically the middle third between the hip and knee, constitutes the second approved injection site. This area typically contains adequate subcutaneous tissue and is easily accessible for self-injection. Patients should avoid the inner thigh due to increased sensitivity and proximity to major blood vessels and nerves. The thigh may be particularly suitable for patients with limited abdominal subcutaneous tissue or those who prefer alternating between different body regions.
Upper Arm: The back of the upper arm, specifically the area between the shoulder and elbow on the outer posterior surface, represents the third FDA-approved site. According to the Instructions for Use, this location requires administration by a caregiver due to the difficulty of reaching this area independently. The upper arm site should only be used when adequate subcutaneous tissue is present, as insufficient tissue depth may result in inadvertent intramuscular injection, potentially altering absorption kinetics.
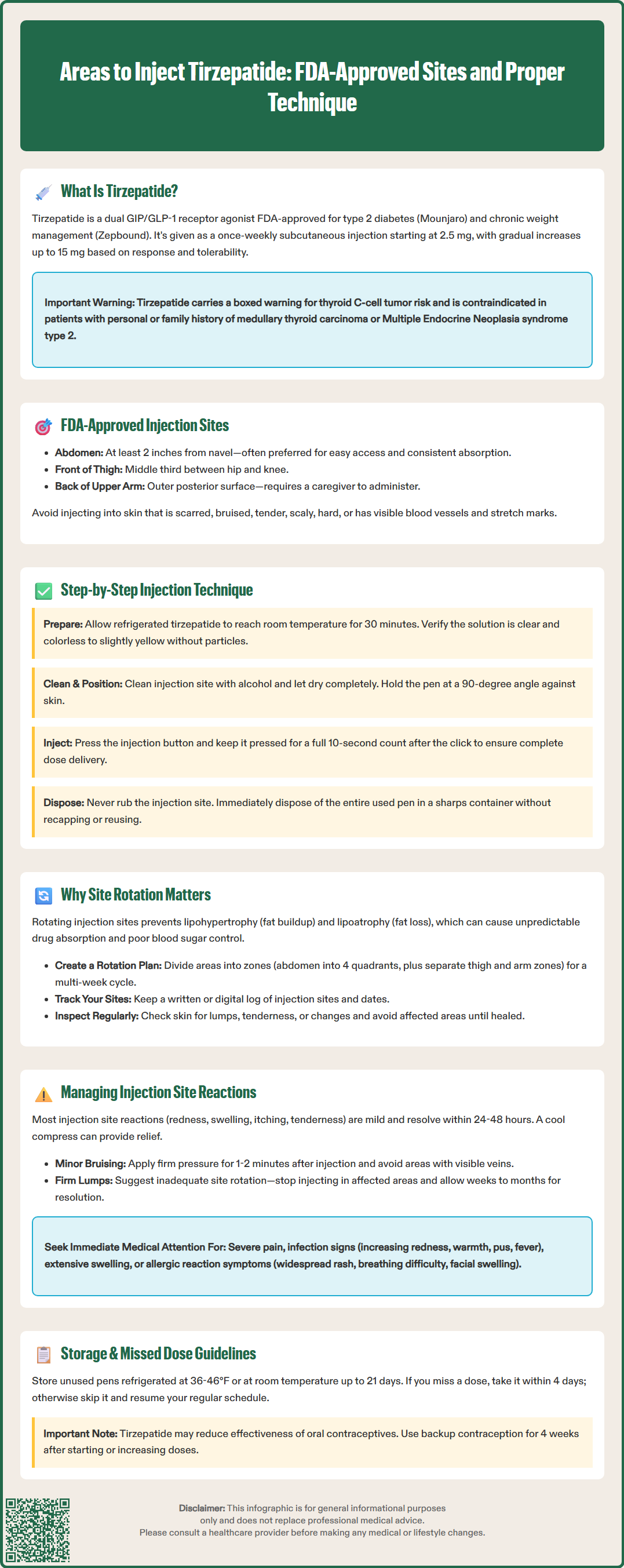
Proper injection technique is essential for ensuring optimal drug delivery, minimizing discomfort, and reducing the risk of injection site complications. Patients should receive comprehensive training from their healthcare provider or diabetes educator before initiating self-administration.
Preparation: Remove the tirzepatide single-dose pen or prefilled syringe from refrigerated storage and allow it to reach room temperature for approximately 30 minutes before injection, as cold medication may cause increased discomfort. Wash hands thoroughly with soap and water. Inspect the medication through the pen window to ensure it appears clear and colorless to slightly yellow; do not use if the solution is cloudy, discolored, or contains particles. Check the expiration date and ensure you have the correct medication and dose.
Site Selection and Cleaning: Choose an injection site from the three approved areas (abdomen, front of thigh, or upper arm with caregiver assistance), ensuring rotation from the previous week's location. Clean the selected site with an alcohol wipe using a circular motion from the center outward, and allow the skin to air dry completely. Injecting into wet skin may cause stinging and increase infection risk.
Injection Technique for Single-Dose Pen: Remove the base cap from the pen and place the clear base flat against the skin at the injection site at a 90-degree angle. Unlock the pen if required by your specific device. Press and hold the injection button until you hear a click, then continue holding the pen against your skin while slowly counting to 10 to ensure complete dose delivery. You may hear a second click. Remove the pen from your skin and verify the completion indicator shows the injection is complete.
Post-Injection Care: Do not rub the injection site, as this may affect absorption. Safely dispose of the entire used pen or syringe in an FDA-cleared sharps container immediately. Do not recap, reuse, or share devices. Monitor for any immediate adverse reactions such as severe pain, bleeding, or signs of allergic response.
Storage and Missed Doses: Unused pens/syringes should be stored in the refrigerator between 36°F and 46°F (2°C to 8°C) in the original carton to protect from light. Do not freeze. If needed, tirzepatide may be stored at room temperature (up to 86°F/30°C) for up to 21 days. If a dose is missed, administer as soon as possible within 4 days (96 hours); if more than 4 days have passed, skip the missed dose and administer the next dose on the regularly scheduled day.
Systematic rotation of injection sites is a critical component of safe and effective tirzepatide administration. Repeated injections into the same anatomical location can lead to lipohypertrophy—the abnormal accumulation of subcutaneous fat tissue—or lipoatrophy, characterized by localized loss of fat tissue. These structural changes not only create cosmetic concerns but can potentially impair drug absorption, leading to unpredictable glycemic control and suboptimal therapeutic outcomes.
Lipohypertrophy develops through chronic local trauma and inflammatory responses triggered by repeated needle insertion and medication deposition. The affected tissue becomes firm, lumpy, and may appear raised compared to surrounding skin. When medications are injected into lipohypertrophic areas, absorption may become erratic due to altered tissue architecture and reduced vascularity. This phenomenon has been well-documented with insulin therapy, and similar principles are believed to apply to other injectable medications including tirzepatide.
Recommended Rotation Strategy: Patients should develop a systematic rotation plan that uses a different site each week, as specified in the tirzepatide Instructions for Use. A practical approach involves dividing each anatomical area into multiple zones and using a different zone each week. For example, the abdomen can be divided into four quadrants (upper right, upper left, lower right, lower left), while each thigh and upper arm represents separate zones. This creates a rotation cycle spanning several weeks before returning to the initial site, allowing adequate tissue recovery time.
Maintaining a written or digital log of injection sites and dates helps ensure consistent rotation and prevents inadvertent reuse of recent sites. Patients should inspect injection sites regularly for signs of lipohypertrophy, tenderness, or skin changes, and avoid using affected areas until complete resolution occurs. Healthcare providers should perform periodic skin examinations during follow-up visits to identify early tissue changes and reinforce proper rotation techniques according to American Diabetes Association and Association of Diabetes Care and Education Specialists recommendations.
While tirzepatide is generally well-tolerated, local injection site reactions can occur. Understanding these reactions and appropriate management strategies is essential for maintaining treatment adherence and patient comfort.
Mild Reactions: The most common injection site reactions include transient redness (erythema), mild swelling, itching, and tenderness at the injection site. These reactions typically appear within hours of injection and resolve spontaneously within 24-48 hours without intervention. According to the FDA prescribing information, injection site reactions are generally infrequent with tirzepatide. Applying a cool compress for 10-15 minutes after injection may provide symptomatic relief. Over-the-counter antihistamines can be considered for persistent itching, though patients should consult their healthcare provider before adding any new medications.
Bruising and Bleeding: Minor bruising or small amounts of bleeding may occur if the needle inadvertently punctures a small blood vessel. This is generally harmless and resolves within several days. To minimize bruising risk, patients should avoid injecting into areas with visible veins and apply firm pressure (without rubbing) for 1-2 minutes immediately after injection if bleeding occurs. Patients taking anticoagulants or antiplatelet medications may experience increased bruising frequency but should continue their prescribed therapy unless otherwise directed by their healthcare provider. These patients may need to apply pressure for a longer period after injection.
Nodules and Lumps: Firm nodules or lumps at injection sites may indicate lipohypertrophy from inadequate site rotation or, less commonly, localized inflammatory reactions. Patients should discontinue injecting into affected areas and implement strict site rotation protocols. Most nodules gradually resolve over weeks to months with avoidance. Persistent or enlarging nodules warrant medical evaluation to exclude rare complications such as abscess formation.
When to Seek Medical Attention: Patients should contact their healthcare provider promptly if they experience severe pain at the injection site, signs of infection (increasing redness, warmth, purulent drainage, fever), extensive swelling, or symptoms suggesting allergic reaction (widespread rash, difficulty breathing, facial swelling). These findings may indicate serious complications requiring immediate medical assessment and potential treatment modification. Any injection site reaction that persists beyond one week or progressively worsens should also prompt clinical evaluation to ensure appropriate management and rule out alternative diagnoses.
No, you should rotate injection sites each week to prevent lipohypertrophy (abnormal fat accumulation) or lipoatrophy (fat tissue loss), which can impair drug absorption and lead to unpredictable blood sugar control. Use a different area or zone within the three FDA-approved sites (abdomen, thigh, upper arm) each week.
The FDA Instructions for Use specify that the upper arm injection site requires caregiver assistance due to difficulty reaching the correct area (back of the upper arm between shoulder and elbow) independently. Self-injection in this location may result in improper technique or inadvertent intramuscular injection if adequate subcutaneous tissue is not accessed.
Stop injecting into the affected area immediately and implement strict site rotation to allow the tissue to heal. Most lumps (lipohypertrophy) resolve gradually over weeks to months with avoidance, but persistent or enlarging nodules should be evaluated by your healthcare provider to exclude complications such as infection.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.