LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does tirzepatide cross the blood-brain barrier? This question matters for clinicians prescribing this dual GIP/GLP-1 receptor agonist for type 2 diabetes and weight management. Tirzepatide (Mounjaro, Zepbound) is a large peptide molecule that likely has minimal direct blood-brain barrier penetration due to its molecular size. However, the medication still produces central nervous system effects through indirect pathways, including vagal signaling and action at circumventricular organs. Understanding tirzepatide's mechanism helps clinicians counsel patients on its safety profile and therapeutic benefits for glycemic control and weight management.
Quick Answer: Tirzepatide likely has minimal direct blood-brain barrier penetration due to its large molecular size (approximately 4,800 daltons), but produces central nervous system effects through indirect pathways.
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Marketed under the brand names Mounjaro (for diabetes) and Zepbound (for weight management), tirzepatide represents the first dual incretin receptor agonist available in clinical practice.
The medication works through a unique dual mechanism of action. As a GIP receptor agonist, tirzepatide enhances insulin secretion in a glucose-dependent manner, reduces glucagon secretion, and may improve insulin sensitivity. Simultaneously, its GLP-1 receptor agonist activity stimulates insulin release, suppresses glucagon secretion, slows gastric emptying, and reduces appetite. This dual action contributes to effective glycemic control and weight loss.
Tirzepatide is administered as a once-weekly subcutaneous injection, with doses ranging from 2.5 mg to 15 mg depending on the indication and patient tolerance. The medication is metabolized by proteolysis and beta-oxidation with excretion of metabolites in urine and feces, and has a half-life of approximately five days. In clinical trials, tirzepatide demonstrated significant reductions in hemoglobin A1c (up to 2.5% reduction) in patients with type 2 diabetes. For weight management, Zepbound is indicated for adults with a BMI ≥30 kg/m² or ≥27 kg/m² with at least one weight-related comorbidity, as an adjunct to reduced-calorie diet and increased physical activity. In the SURMOUNT-1 trial, adults with obesity without diabetes achieved weight loss of up to 22.5%, while those with type 2 diabetes typically experienced somewhat lower weight reductions.
The pharmacological profile of tirzepatide makes it particularly effective for patients requiring both glycemic control and weight management, addressing two critical components of metabolic disease management simultaneously.
Understanding the distinction between central (brain-mediated) and peripheral effects of incretin-based therapies is essential for comprehending how tirzepatide exerts its therapeutic benefits. GLP-1 and GIP receptors are distributed throughout the body, including the pancreas, gastrointestinal tract, cardiovascular system, and central nervous system.
Peripheral mechanisms appear to account for many of tirzepatide's metabolic effects. In the pancreas, the medication enhances glucose-dependent insulin secretion from beta cells while suppressing glucagon release from alpha cells. In the gastrointestinal tract, GLP-1 receptor activation slows gastric emptying, which contributes to improved postprandial glucose control and increased satiety. These peripheral actions occur without requiring the medication to enter the brain.
Central nervous system effects also likely contribute to the therapeutic profile of incretin-based medications. GLP-1 receptors are present in several brain regions, including the hypothalamus, brainstem, and areas involved in appetite regulation and reward processing. Activation of these central receptors may reduce food intake, modulate eating behavior, and influence energy expenditure. The role of central GIP receptors remains less well characterized and is an area of ongoing investigation.
Current evidence suggests that large peptide molecules like tirzepatide primarily exert their central effects through indirect pathways rather than direct brain penetration. These include activation of GLP-1 receptors on vagal afferent neurons in the gastrointestinal tract, which transmit signals to the brainstem, and potential action at circumventricular organs—specialized brain regions with a more permeable blood-brain barrier. These indirect mechanisms allow for central nervous system modulation without requiring substantial penetration of the blood-brain barrier, though direct human data on CNS distribution of long-acting incretin agonists remain limited.
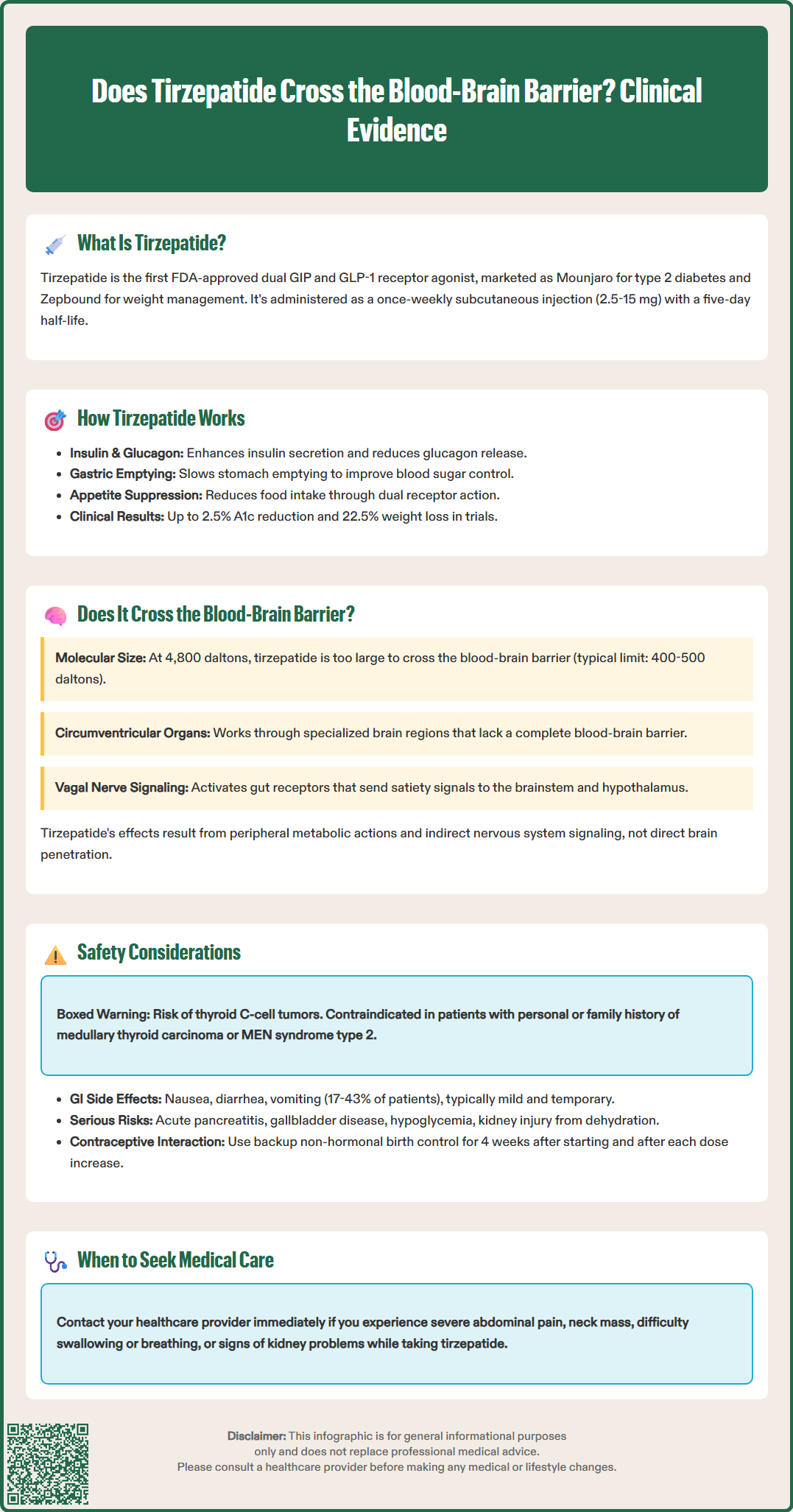
Tirzepatide has demonstrated a generally favorable safety profile in clinical trials, though clinicians should be aware of common adverse effects and important contraindications. The most frequently reported side effects are gastrointestinal in nature, with dose-dependent rates that vary by indication. For Mounjaro, these include nausea (17-25%), diarrhea (13-24%), vomiting (6-12%), and constipation (10-17%). For Zepbound, rates are generally higher, with nausea affecting up to 43% of patients at the highest dose. These effects are typically mild to moderate and tend to diminish over time with continued use.
Serious adverse effects require clinical vigilance. Tirzepatide carries a boxed warning regarding the risk of thyroid C-cell tumors, based on rodent studies showing increased incidence of medullary thyroid carcinoma. The medication is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2. Other serious risks include acute pancreatitis (reported as 0.23 cases per 100 patient-years), acute gallbladder disease, hypoglycemia (particularly when combined with insulin or sulfonylureas), acute kidney injury (often secondary to dehydration from gastrointestinal effects), and hypersensitivity reactions. Zepbound carries an additional warning to monitor for depression or suicidal thoughts.
Patient counseling should emphasize the importance of gradual dose escalation to minimize gastrointestinal side effects, adequate hydration, and recognition of warning symptoms. Patients should be instructed to seek immediate medical attention for severe abdominal pain (possible pancreatitis), symptoms of thyroid tumors (neck mass, dysphagia, dyspnea), or signs of acute kidney injury. Dose adjustments of concomitant diabetes medications may be necessary to prevent hypoglycemia. Tirzepatide is not recommended in patients with severe gastrointestinal disease, including severe gastroparesis.
Special populations require additional consideration. No dosage adjustment is needed for patients with renal impairment, though renal function should be monitored in patients experiencing severe adverse gastrointestinal reactions. The medication should be discontinued upon recognition of pregnancy, and women planning pregnancy should discuss timing with their healthcare provider. Tirzepatide may decrease the exposure of oral contraceptives, so patients should use an additional non-hormonal method for 4 weeks after initiation and after each dose escalation. Coadministration with other GLP-1 receptor agonists or tirzepatide-containing products is not recommended.
The question of whether tirzepatide crosses the blood-brain barrier is clinically relevant given the medication's effects on appetite, food intake, and eating behavior. Based on available evidence, tirzepatide likely has minimal blood-brain barrier penetration in its intact form, primarily due to its molecular characteristics.
Tirzepatide is a large peptide molecule with a molecular weight of approximately 4,800 daltons. The blood-brain barrier is highly selective, generally restricting passage to small, lipophilic molecules (typically <400-500 daltons). Large hydrophilic peptides like tirzepatide face significant barriers to direct brain penetration. Preclinical studies with other GLP-1 receptor agonists have demonstrated limited brain uptake, suggesting minimal blood-brain barrier penetration, though tirzepatide-specific human data are limited.
Despite likely minimal direct penetration, tirzepatide produces central nervous system effects through alternative mechanisms. The medication can activate GLP-1 and GIP receptors in circumventricular organs—specialized brain regions including the area postrema and median eminence that lack a complete blood-brain barrier. These regions serve as sensory interfaces between the peripheral circulation and central nervous system. Additionally, tirzepatide activates GLP-1 receptors on vagal afferent neurons in the gastrointestinal tract, which transmit satiety signals to the nucleus tractus solitarius in the brainstem, subsequently influencing hypothalamic appetite centers.
Current evidence suggests that tirzepatide's therapeutic effects do not require direct blood-brain barrier penetration. The medication's appetite suppression and weight loss benefits appear to result from a combination of peripheral metabolic effects, vagal signaling, and action at circumventricular organs. This mechanism is consistent with other GLP-1 receptor agonists and represents an important distinction from centrally acting weight loss medications that directly penetrate the blood-brain barrier. Understanding this mechanism helps clinicians counsel patients appropriately regarding the medication's safety profile and expected effects.
Tirzepatide reduces appetite through indirect pathways including activation of GLP-1 receptors on vagal afferent neurons in the gastrointestinal tract and action at circumventricular organs—specialized brain regions with incomplete blood-brain barriers. These mechanisms allow central nervous system modulation without requiring direct brain penetration.
The most common side effects are gastrointestinal, including nausea (17-43% depending on dose and indication), diarrhea (13-24%), vomiting (6-12%), and constipation (10-17%). These effects are typically mild to moderate and tend to diminish over time with continued use and gradual dose escalation.
Tirzepatide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2. It should be discontinued upon recognition of pregnancy and is not recommended in patients with severe gastrointestinal disease, including severe gastroparesis.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.