LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide injection site reaction treatment focuses on managing localized symptoms that can occur with Mounjaro and Zepbound injections. These dual GIP/GLP-1 receptor agonists, administered weekly for type 2 diabetes and weight management, cause injection site reactions in approximately 2-5% of patients. Most reactions—including redness, swelling, tenderness, and itching—are mild and self-limiting, resolving within days. Understanding proper treatment approaches, from cold compresses and topical corticosteroids to preventive injection techniques, helps patients manage discomfort effectively while recognizing when medical evaluation is necessary for signs of infection or allergic response.
Quick Answer: Tirzepatide injection site reactions are typically treated with cold compresses, over-the-counter hydrocortisone cream, oral antihistamines for itching, and proper injection technique to prevent future occurrences.
Tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management and chronic weight management. Administered as a once-weekly subcutaneous injection, tirzepatide can cause localized reactions at the injection site, similar to other injectable medications.
Injection site reactions occur when the body responds to the physical trauma of needle insertion, the medication itself, or both. These reactions are generally mild and self-limiting, representing a common adverse effect rather than a serious safety concern. According to FDA prescribing information, injection site reactions vary by dose and formulation, with clinical trials showing rates of approximately 1.7-5.2% for Mounjaro and 2.4-5.3% for Zepbound, depending on the dose used.
The mechanism behind these reactions typically involves a localized inflammatory response. When tirzepatide is injected into subcutaneous tissue, the immune system may recognize the medication or the injection process as a minor insult, triggering the release of inflammatory mediators such as histamine and cytokines. This localized inflammation manifests as redness, swelling, or discomfort at the injection site. Understanding that these reactions are usually benign helps patients manage expectations and reduces anxiety when they occur. Most injection site reactions resolve spontaneously within a few days without specific intervention, though proper management techniques can improve comfort.
Injection site reactions to tirzepatide present with characteristic local symptoms that patients should recognize. The most frequently reported symptoms include erythema (redness), mild swelling or induration, tenderness or pain, and itching (pruritus) at the injection site. These symptoms typically appear within hours of injection and generally peak within 24-48 hours before gradually resolving.
Typical presentation includes:
Localized redness: A circular or irregular area of pink to red discoloration, usually 1-3 cm in diameter, centered around the injection point
Swelling: Mild elevation of the skin with a firm or slightly boggy texture, reflecting subcutaneous fluid accumulation and inflammation
Tenderness: Discomfort ranging from mild sensitivity to moderate pain when the area is touched or pressed
Pruritus: Itching sensation that may be mild to moderate, occasionally accompanied by a desire to scratch
Warmth: The affected area may feel slightly warmer than surrounding skin due to increased blood flow
Less commonly, patients may notice small bruises (ecchymoses) or minor bleeding at the injection site, particularly if a small blood vessel was inadvertently punctured during injection. Some individuals report a small, firm nodule or lump under the skin that persists for several days, representing localized medication depot or minor tissue reaction.
It is important to distinguish normal injection site reactions from signs of infection or allergic response. Symptoms that remain localized, mild, and self-limiting within 3-5 days are consistent with typical injection site reactions. However, symptoms that worsen progressively, spread beyond the immediate injection area, or are accompanied by systemic symptoms such as fever or malaise warrant prompt medical evaluation.
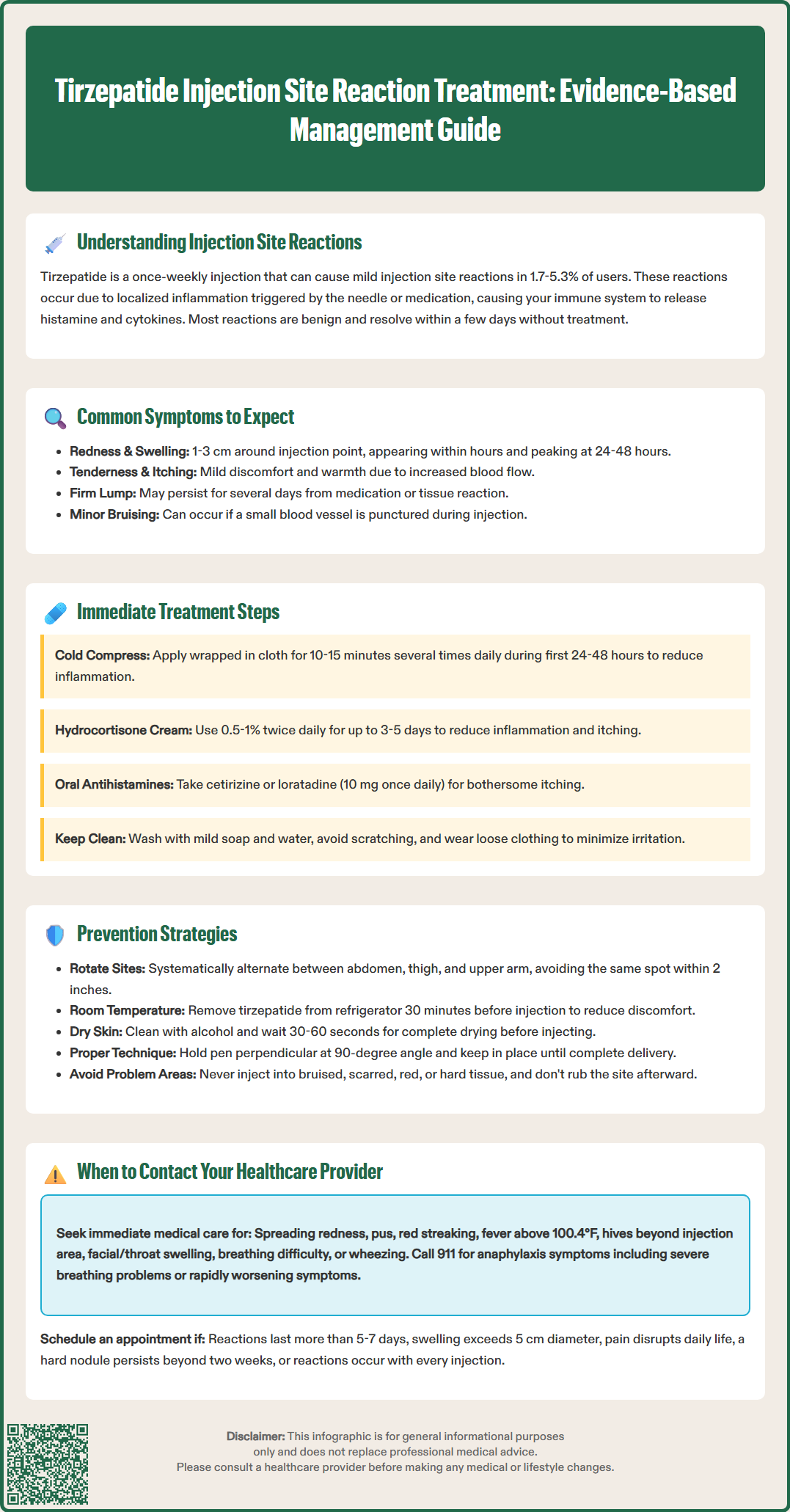
Most tirzepatide injection site reactions respond well to simple, conservative management strategies that patients can implement at home. The primary goals of immediate treatment are to reduce inflammation, alleviate discomfort, and prevent secondary complications such as infection from scratching.
First-line management approaches include:
Cold compresses: Apply a clean, cold compress or ice pack wrapped in a thin cloth to the affected area for 10-15 minutes at a time, several times daily during the first 24-48 hours. Cold therapy causes vasoconstriction, reducing blood flow to the area and thereby decreasing inflammation, swelling, and pain. Avoid applying ice directly to skin to prevent cold injury.
Topical treatments: Over-the-counter hydrocortisone cream (0.5-1%) can be applied sparingly to reduce inflammation and itching. Apply a thin layer twice daily for up to 3-5 days. For pruritus without significant inflammation, calamine lotion may provide symptomatic relief. Ensure the injection site is clean and dry before applying any topical medication.
Oral antihistamines: If itching is bothersome, oral non-sedating antihistamines such as cetirizine (10 mg once daily) or loratadine (10 mg once daily) can provide systemic relief. Diphenhydramine (25-50 mg every 6 hours as needed) is an alternative but causes significant drowsiness and has anticholinergic effects that may be problematic, especially in older adults. Avoid driving or operating machinery if using diphenhydramine.
Gentle skin care: Keep the injection site clean with mild soap and water. Avoid scratching, which can introduce bacteria and lead to secondary infection. Pat the area dry gently and avoid tight clothing that may irritate the site.
Oral analgesics: For significant discomfort, acetaminophen (500-1000 mg every 6 hours as needed, not exceeding 3000 mg daily) can provide pain relief. Those with liver disease or who consume alcohol regularly should use lower doses and consult their healthcare provider. Alternatively, ibuprofen (200-400 mg every 6-8 hours with food, not exceeding 1200 mg daily for OTC use) can provide both pain relief and anti-inflammatory effects. NSAIDs like ibuprofen should be used cautiously in people with kidney disease, heart failure, history of stomach ulcers, or those taking blood thinners.
Avoid applying heat to the injection site during the acute phase, as this may increase inflammation and discomfort. Do not attempt to drain or puncture any swelling, as this increases infection risk.
Prevention strategies significantly reduce the incidence and severity of injection site reactions with tirzepatide. Proper injection technique, site rotation, and medication handling are fundamental to minimizing local adverse effects.
Injection technique optimization:
Site rotation: Rotate injection sites systematically between the abdomen, thigh, and upper arm (if assistance is available). Avoid injecting into the same spot within at least 2 inches of a previous injection site. Maintain a rotation schedule to allow adequate healing time between injections in the same general area.
Proper device use: Follow the Instructions for Use (IFU) provided with your Mounjaro or Zepbound pen. Place the pen perpendicular (90-degree angle) to the skin, press firmly against the skin, and hold the button until the injection is complete and you hear or feel a click. Hold the pen in place for the time specified in your device instructions to ensure complete delivery.
Skin preparation: Clean the injection site with an alcohol swab and allow it to dry completely (30-60 seconds) before injection. Injecting through wet alcohol can cause stinging and irritation.
Room temperature medication: Remove tirzepatide from the refrigerator 30 minutes before injection to allow it to reach room temperature. This can reduce discomfort during injection. Never warm the medication by other means (microwave, hot water, etc.).
Additional preventive measures:
Avoid problematic areas: Do not inject into skin that is tender, bruised, red, scaly, hard, or has scars or stretch marks. These areas have altered tissue architecture that may predispose to reactions.
Proper storage: Store tirzepatide in the refrigerator (36°F to 46°F) and protect from light. Do not freeze. Follow the product-specific storage instructions for how long the pen can remain at room temperature if needed.
Post-injection care: Do not rub or massage the injection site after administration, as this may increase irritation or alter medication absorption.
Needle safety: Use each pen only once as directed. Never share pens between patients, even if the needle is changed.
Patients who experience persistent reactions despite proper technique should discuss alternative injection sites or administration strategies with their healthcare provider. In some cases, healthcare providers may recommend taking an oral antihistamine before injection, though this approach should only be implemented under medical supervision.
While most injection site reactions are benign and self-limiting, certain symptoms warrant prompt medical evaluation to rule out infection, allergic reaction, or other complications. Patients should be educated on red flag symptoms that require professional assessment.
Contact your healthcare provider if you experience:
Signs of infection:
Increasing redness that spreads beyond the immediate injection site
Warmth and swelling that worsens after 48 hours rather than improving
Purulent drainage (pus) or foul odor from the injection site
Red streaking extending from the injection site (lymphangitis)
Fever (temperature >100.4°F or 38°C) or chills
Increasing pain that is disproportionate to the visible reaction
Signs of allergic reaction:
Hives (urticaria) or rash extending beyond the injection site
Facial swelling, particularly of the lips, tongue, or throat
Difficulty breathing, wheezing, or chest tightness
Dizziness, lightheadedness, or rapid heartbeat
Persistent or severe local reactions:
Injection site reactions lasting more than 5-7 days without improvement
Large areas of induration or swelling (>5 cm diameter)
Severe pain that interferes with daily activities or sleep
Development of a hard, painful nodule that persists beyond two weeks
Seek emergency care immediately if you develop symptoms of anaphylaxis, including difficulty breathing, throat swelling, severe dizziness, or rapid progression of symptoms. Call 911 or go to the nearest emergency department.
For recurrent injection site reactions that occur with every dose, schedule a non-urgent appointment with your healthcare provider or diabetes care and education specialist (CDCES). They can observe your injection technique, recommend modifications, or consider whether tirzepatide remains the most appropriate medication for your situation. Documentation of reaction patterns, including photographs if possible, helps clinicians assess severity and guide management decisions.
Serious or unexpected adverse reactions to tirzepatide should be reported to the FDA MedWatch program (www.fda.gov/medwatch or 1-800-FDA-1088), which helps monitor medication safety after approval.
Most tirzepatide injection site reactions appear within hours of injection, peak at 24-48 hours, and resolve spontaneously within 3-5 days. Reactions persisting beyond 5-7 days without improvement warrant medical evaluation.
Use cold compresses or ice packs wrapped in cloth for 10-15 minutes several times daily during the first 48 hours to reduce inflammation and swelling. Avoid heat during the acute phase, as it may worsen inflammation and discomfort.
Contact your healthcare provider for spreading redness, purulent drainage, fever above 100.4°F, red streaking from the injection site, reactions lasting more than 5-7 days, or signs of allergic reaction such as hives, facial swelling, or difficulty breathing.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.