LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
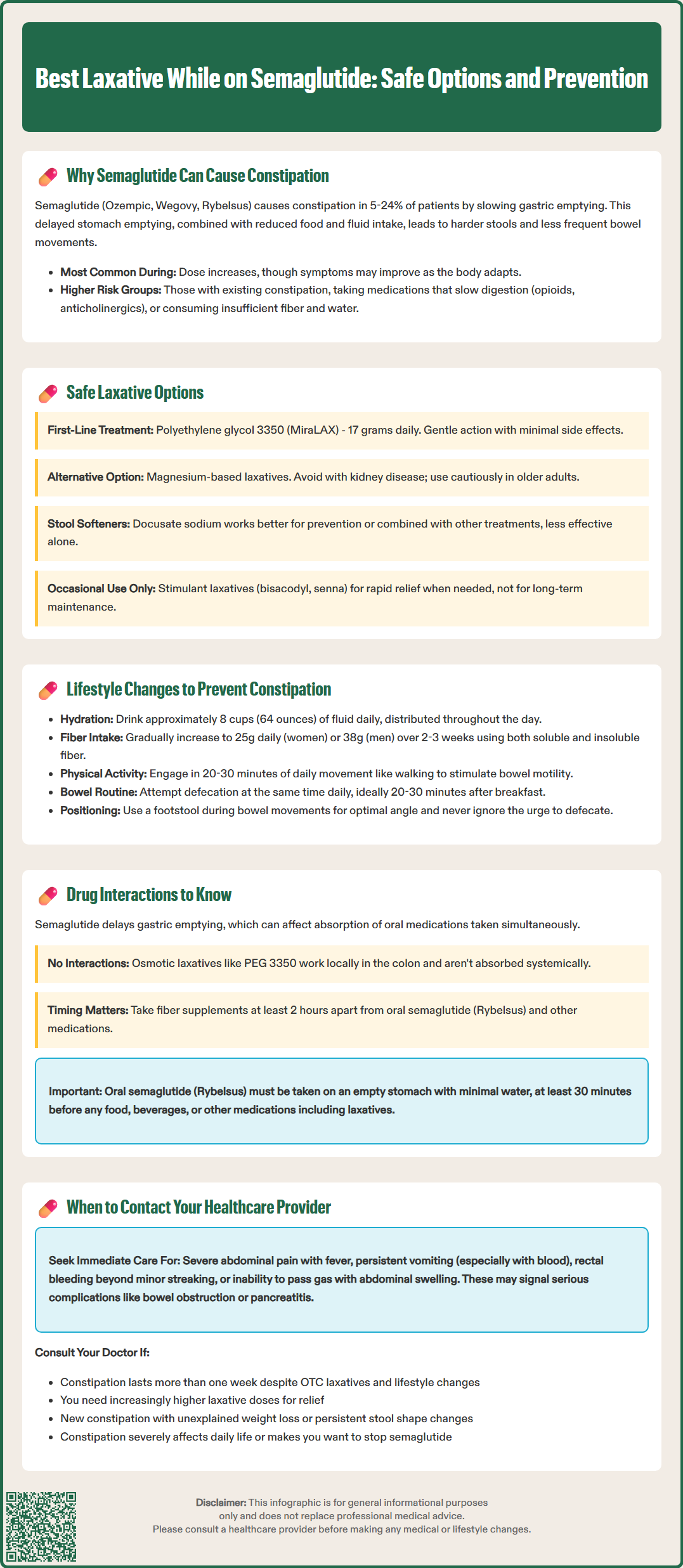
Constipation is a common side effect experienced by patients taking semaglutide (Ozempic, Wegovy, Rybelsus), affecting 5-24% of users depending on formulation and dose. This gastrointestinal issue stems from semaglutide's mechanism as a GLP-1 receptor agonist, which slows gastric emptying to improve blood sugar control and promote satiety. While this delayed transit contributes to the medication's therapeutic benefits, it can lead to uncomfortable bowel changes that impact treatment adherence. Understanding which laxatives are safe and effective while on semaglutide, along with preventive lifestyle strategies, helps patients maintain comfort and continue benefiting from this FDA-approved medication for type 2 diabetes and chronic weight management.
Quick Answer: Polyethylene glycol 3350 (MiraLAX) is generally considered the best first-line laxative for semaglutide-related constipation due to its gentle mechanism, predictable effects, and minimal systemic absorption.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (under the brand names Ozempic and Rybelsus) and chronic weight management (Wegovy). While gastrointestinal side effects are well-documented with this medication, constipation represents a common adverse effect that can impact patient adherence and quality of life.
The mechanism underlying semaglutide-induced constipation primarily relates to its pharmacological action. GLP-1 receptor agonists slow gastric emptying as part of their therapeutic effect. This delayed transit time allows for improved glycemic control and enhanced satiety, contributing to weight loss. However, this slowed gastric emptying, combined with reduced food and fluid intake and potential dehydration, can lead to harder stools and reduced bowel movement frequency in susceptible individuals.
Clinical trial data from the SUSTAIN and STEP programs indicate that gastrointestinal adverse effects are common with semaglutide. Constipation rates vary by formulation and dose, with approximately 5-15% of patients on Ozempic and 11-24% of patients on Wegovy reporting constipation. The incidence tends to be higher during dose escalation phases and may improve with continued therapy as physiological adaptation occurs. Individual susceptibility varies considerably based on baseline bowel habits, dietary fiber intake, hydration status, and concurrent medications.
Patients with pre-existing constipation, those taking other medications that slow gut motility (such as opioids or anticholinergics), and individuals with inadequate fluid or fiber intake face elevated risk. Understanding this mechanism helps clinicians anticipate the problem and implement preventive strategies early in treatment, potentially improving long-term adherence to this effective metabolic therapy.
When lifestyle modifications prove insufficient, pharmacological intervention becomes necessary to manage semaglutide-related constipation. The selection of an appropriate laxative should prioritize safety, efficacy, and compatibility with the patient's overall medication regimen and health status.
Osmotic laxatives represent the first-line pharmacological option for most patients on semaglutide. Polyethylene glycol 3350 (PEG 3350, brand name MiraLAX) is particularly well-suited due to its gentle mechanism, predictable effect, and minimal systemic absorption. This agent draws water into the colon, softening stool and promoting natural peristalsis. The typical starting dose is 17 grams (one capful) dissolved in 4-8 ounces of beverage daily, with effects usually apparent within 1-3 days. While PEG 3350 is generally well-tolerated with minimal adverse effects beyond occasional bloating or flatulence, the over-the-counter label recommends use for no more than 7 days without healthcare provider supervision. For semaglutide-related constipation, longer-term use may be appropriate under clinician guidance.
Magnesium-based osmotic laxatives (such as magnesium hydroxide or milk of magnesia) offer an alternative, though they should be avoided in patients with significant kidney disease and used cautiously in older adults due to potential magnesium accumulation. Lactulose, another osmotic agent available by prescription in the US, may cause more gas and bloating but remains effective for patients who cannot tolerate PEG formulations.
Stool softeners like docusate sodium (Colace) work by allowing water and fats to penetrate the stool, making it easier to pass. While generally safe, docusate is less effective than osmotic laxatives for established constipation and works best as a preventive measure or in combination with other agents. The typical dose is 100-300 mg daily.
Stimulant laxatives such as bisacodyl (Dulcolax) or senna (Senokot) are appropriate for intermittent or adjunct use. These agents stimulate colonic contractions and can provide relief within 6-12 hours. They are suitable for occasional use when more rapid relief is needed but are not typically recommended as sole maintenance therapy.
Rectal options such as glycerin or bisacodyl suppositories can provide rapid relief for patients needing immediate results and may be useful as rescue therapy.
Patients should start with the gentlest effective option—typically PEG 3350—and escalate only if necessary, always under healthcare provider guidance.
While constipation on semaglutide is common and often manageable with over-the-counter interventions, certain clinical scenarios warrant prompt medical evaluation to exclude serious complications or underlying pathology.
Immediate medical attention is required if patients experience severe abdominal pain, particularly if localized, persistent, or accompanied by fever, which may indicate complications such as bowel obstruction, fecal impaction, or rarely, intestinal ischemia. Severe, persistent epigastric pain radiating to the back may indicate pancreatitis, a rare but serious potential complication of GLP-1 receptor agonists. Vomiting, especially if persistent or containing blood or material resembling coffee grounds, requires urgent assessment. Rectal bleeding beyond minor streaking from hemorrhoids, particularly if dark or tarry stools are present, necessitates investigation to exclude gastrointestinal pathology. Inability to pass gas combined with progressive abdominal distension suggests possible obstruction, and laxatives should be avoided in this situation.
Routine consultation should occur when constipation persists beyond one week despite appropriate use of over-the-counter laxatives and lifestyle modifications. This timeline allows for reasonable self-management attempts while preventing prolonged discomfort and potential complications. Patients who require escalating laxative doses or find that previously effective treatments no longer work should discuss alternative management strategies with their provider.
Additionally, new or worsening constipation accompanied by unexplained weight loss (beyond expected therapeutic weight reduction), persistent changes in stool caliber, or alternating constipation and diarrhea warrants evaluation to exclude structural or neoplastic causes, particularly in patients age 45 or older or those with family history of colorectal cancer.
Patients should also contact their healthcare provider if constipation significantly impacts quality of life or medication adherence, as dose adjustment or alternative GLP-1 receptor agonist formulations may be considered. The goal is to maintain the metabolic benefits of semaglutide while ensuring patient comfort and safety through individualized management approaches.
Non-pharmacological interventions form the foundation of constipation management in patients taking semaglutide and should be implemented proactively at treatment initiation rather than reactively after symptoms develop.
Adequate hydration represents a crucial lifestyle modification. Most patients should aim for approximately 8 cups (64 ounces) of fluid daily, though individual needs vary based on body weight, activity level, climate, and medical conditions. Patients with heart failure, kidney disease, or other conditions requiring fluid restriction should follow their healthcare provider's specific guidance. Increased fluid intake helps maintain stool softness and supports the osmotic action of dietary fiber. Patients should be counseled to distribute fluid intake throughout the day rather than consuming large volumes at once, and to increase intake during hot weather or physical activity.
Dietary fiber optimization requires a balanced approach. The Academy of Nutrition and Dietetics recommends approximately 25 grams of fiber daily for women and 38 grams for men, from varied sources. Soluble fiber from oats, psyllium, beans, and fruits helps retain water in stool, while insoluble fiber from whole grains, vegetables, and wheat bran adds bulk and promotes transit. Patients should increase fiber gradually over 2-3 weeks to minimize gas and bloating, which can be particularly problematic given semaglutide's effect on gastric emptying. A fiber supplement such as psyllium husk (Metamucil) can help patients meet targets when dietary intake is insufficient, but must be taken with adequate water.
Regular physical activity stimulates colonic motility through multiple mechanisms, including increased abdominal muscle tone and enhanced parasympathetic nervous system activity. Even modest activity—such as 20-30 minutes of walking daily—can significantly improve bowel regularity. Patients should be encouraged to find sustainable activities that fit their lifestyle and physical capabilities.
Establishing consistent bowel habits helps train the gastrocolic reflex. Patients should attempt to have a bowel movement at the same time daily, ideally 20-30 minutes after breakfast when the gastrocolic reflex is strongest. Using a footstool to achieve a more squatting-like position during defecation can help optimize the anorectal angle. Adequate time should be allowed without straining, and the urge to defecate should never be ignored or delayed when possible.
These lifestyle modifications work synergistically and are most effective when implemented together as part of a comprehensive approach to gastrointestinal health during semaglutide therapy.
Understanding potential interactions between laxatives and semaglutide is essential for safe and effective constipation management, though clinically significant interactions are relatively uncommon with most over-the-counter laxative preparations.
Semaglutide's primary interaction concern relates to its effect on gastric emptying rather than direct drug-drug interactions with laxatives. Because semaglutide delays gastric emptying, it can affect the absorption of orally administered medications. This is particularly important for oral semaglutide (Rybelsus), which must be taken on an empty stomach with no more than 4 ounces of water, at least 30 minutes before food, beverages, or other oral medications.
Osmotic laxatives such as polyethylene glycol 3350 have no known direct interactions with semaglutide. These agents work through local osmotic effects in the colon and are not systemically absorbed to any significant degree. As a general precaution with any medication that might affect transit time, some clinicians recommend separating other oral medications from laxatives, though this is not a specific label requirement for PEG 3350.
Bulk-forming fiber supplements (psyllium, methylcellulose) should be separated from other oral medications by approximately 2 hours, as they may affect absorption of some drugs. This is particularly important for patients taking oral semaglutide (Rybelsus) or medications with narrow therapeutic windows.
Magnesium-based laxatives should be used cautiously in patients taking medications that affect electrolyte balance or renal function. While there is no direct interaction with semaglutide itself, patients on diuretics, ACE inhibitors, or those with chronic kidney disease should avoid regular use of magnesium laxatives. Magnesium products may also reduce absorption of certain antibiotics like tetracyclines and fluoroquinolones, and should be separated by at least 2 hours.
Stimulant laxatives have no documented interactions with semaglutide, though their use should be limited to intermittent relief rather than daily management.
Patients taking multiple medications should maintain a comprehensive medication list and consult their pharmacist or healthcare provider before adding laxatives to their regimen. While serious interactions are rare, individualized assessment ensures optimal safety, particularly in patients with complex medication regimens or multiple comorbidities common in the population prescribed semaglutide for diabetes or weight management.
Yes, polyethylene glycol 3350 (MiraLAX) is safe to take with semaglutide and is considered a first-line treatment option for semaglutide-related constipation. It has no known direct interactions with semaglutide and works through gentle osmotic action in the colon.
Constipation is often most pronounced during dose escalation phases and may improve with continued therapy as the body adapts. If constipation persists beyond one week despite lifestyle modifications and over-the-counter laxatives, contact your healthcare provider for evaluation and alternative management strategies.
Do not stop semaglutide without consulting your healthcare provider. Most cases of constipation can be managed with appropriate laxatives and lifestyle modifications while continuing the medication, allowing you to maintain its metabolic benefits for diabetes control or weight management.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.