LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide (Mounjaro, Zepbound) is a once-weekly injectable medication that combines GIP and GLP-1 receptor agonist activity for type 2 diabetes and chronic weight management. One common question among patients starting this therapy concerns the best time of day to inject tirzepatide. According to FDA prescribing information, tirzepatide can be administered at any time of day, with or without meals. The key to successful treatment is consistency—injecting on the same day each week maintains stable therapeutic levels and supports adherence. Understanding timing flexibility, practical considerations, and proper injection technique helps patients integrate tirzepatide safely into their weekly routine.
Quick Answer: Tirzepatide can be injected at any time of day, with the most important factor being consistency in administering it on the same day each week.
Tirzepatide is a once-weekly injectable medication approved by the FDA for the treatment of type 2 diabetes mellitus (marketed as Mounjaro) and chronic weight management in adults with obesity or overweight with weight-related comorbidities (marketed as Zepbound). It represents a novel therapeutic class as the first dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist.
The medication works through a dual mechanism of action that targets two incretin hormone pathways simultaneously. By activating GIP receptors, tirzepatide may enhance insulin secretion and potentially improve insulin sensitivity and fat metabolism. Concurrently, GLP-1 receptor activation stimulates glucose-dependent insulin release, suppresses inappropriate glucagon secretion, slows gastric emptying, and reduces appetite through central nervous system pathways. This combined approach results in improved glycemic control, significant weight reduction, and improvements in certain cardiovascular risk factors such as blood pressure and lipid profiles.
Tirzepatide is administered as a subcutaneous injection once weekly, with dosing typically initiated at 2.5 mg for 4 weeks, then increased to 5 mg. Doses can be increased by 2.5 mg increments every 4 weeks as tolerated up to a maximum of 15 mg. The medication's extended half-life of approximately five days allows for consistent therapeutic effects throughout the week. Clinical trials have demonstrated substantial reductions in hemoglobin A1c (HbA1c) levels—often exceeding 2% from baseline. Weight loss varies by population, with adults with obesity without diabetes experiencing approximately 15-20% mean weight loss at higher doses, while those with type 2 diabetes typically achieve somewhat less weight reduction.
Tirzepatide is not indicated for type 1 diabetes and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2).
According to the FDA-approved prescribing information, tirzepatide can be administered at any time of day, with or without meals. There is no officially designated "best" time that enhances efficacy or reduces adverse effects. The most important factor is consistency—patients should aim to inject tirzepatide on the same day each week to maintain stable therapeutic levels and establish a reliable routine that supports adherence.
Many healthcare providers and patients find that selecting a specific day and approximate time helps create a sustainable habit. For instance, choosing Sunday morning or Wednesday evening and maintaining that schedule reduces the likelihood of missed doses. The flexibility in timing allows patients to integrate the injection into their existing routines, whether that involves morning medication administration, evening self-care rituals, or alignment with weekly activities like grocery shopping or religious services.
The medication's long half-life means that minor variations in injection time (within the same day) do not compromise therapeutic effectiveness. If a dose is missed, the prescribing information recommends administering it as soon as possible within 4 days (96 hours) after the missed dose. If more than 4 days have passed, patients should skip the missed dose and resume their regular schedule. Additionally, the weekly dosing day may be changed if at least 3 days (72 hours) have elapsed since the previous dose.
The emphasis on "same day each week" rather than "same time each day" reflects tirzepatide's pharmacokinetic profile and distinguishes it from daily medications where precise timing may be more critical. This flexibility represents a practical advantage for patients managing complex medication regimens.
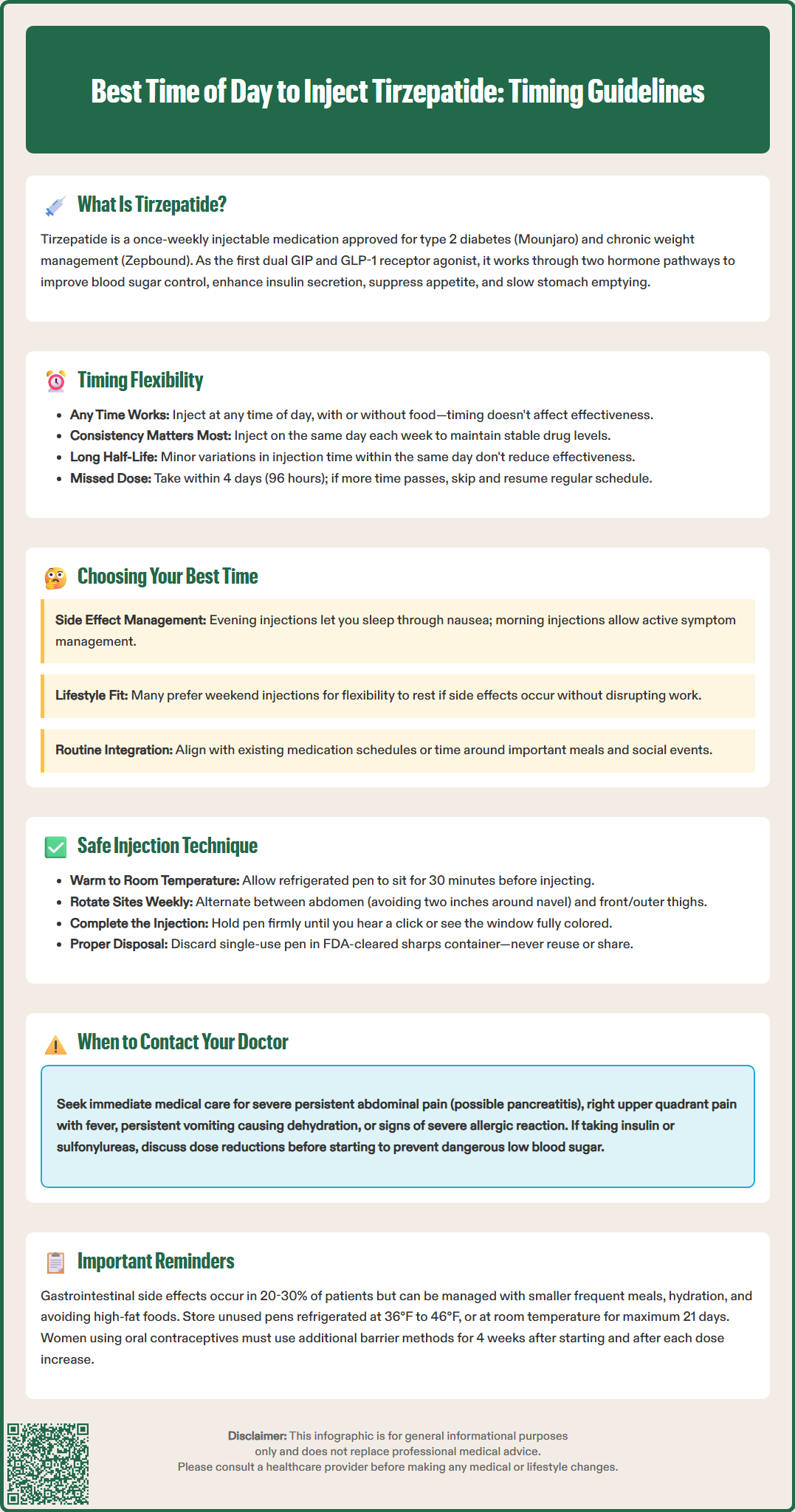
Several practical and clinical factors may influence when patients choose to administer their weekly tirzepatide injection, though these represent individual preferences rather than medical requirements. Gastrointestinal side effects are among the most common considerations. Tirzepatide frequently causes nausea, vomiting, diarrhea, and decreased appetite, particularly during dose initiation and escalation. Some patients prefer evening injections, reasoning that sleeping through the initial hours post-injection may reduce awareness of nausea. Conversely, others choose morning administration to monitor for adverse effects during waking hours when they can implement management strategies.
Work and social schedules significantly impact timing decisions. Patients with demanding weekday responsibilities may prefer weekend injections when they have greater flexibility to rest if side effects occur. Healthcare workers, teachers, or those in customer-facing roles might strategically time injections to minimize potential interference with professional obligations. Similarly, patients may avoid injecting immediately before important social events, travel, or physical activities until they understand their individual response pattern.
Concurrent medications and meal patterns can also inform timing choices. While tirzepatide does not require administration with food, patients taking multiple medications may prefer consolidating their injection with existing medication routines to support adherence. Those experiencing significant appetite suppression might time injections to align with periods when reduced food intake is least disruptive to their nutritional needs or social eating patterns.
Healthcare provider accessibility represents another consideration. Some patients prefer injecting on weekdays when they can readily contact their clinical team if questions or concerns arise, particularly during the initial weeks of therapy. This consideration becomes less relevant as patients gain confidence and experience with self-administration.
Importantly, due to tirzepatide's effect on delaying gastric emptying, it may reduce the absorption of oral contraceptives. Patients using oral contraceptives should use a non-oral method or add a barrier method for 4 weeks after initiation and for 4 weeks after each dose increase. Patients taking insulin or sulfonylureas should discuss potential dose reductions with their healthcare provider to reduce hypoglycemia risk during titration.
Proper injection technique is essential for ensuring medication efficacy, minimizing discomfort, and reducing the risk of injection site reactions. Tirzepatide is supplied in single-dose prefilled pens with a hidden needle designed for subcutaneous injection. Before administration, patients should remove the pen from refrigeration and allow it to reach room temperature for approximately 30 minutes, as injecting cold medication may increase discomfort.
Injection site preparation and rotation are critical safety practices. Patients should select an injection site with adequate subcutaneous tissue, clean the area with an alcohol swab, and allow it to dry completely before injecting. The abdomen (avoiding a two-inch radius around the navel) and front and outer thighs are appropriate sites for self-injection. The back of the upper arms may be used only if the injection is administered by a caregiver. Rotating injection sites weekly helps prevent lipodystrophy, reduces localized irritation, and maintains consistent absorption. Patients should avoid injecting into areas with scarring, bruising, redness, or active skin conditions.
The injection process involves following the specific steps in the Instructions for Use that come with the medication. Unlike multi-dose pens, tirzepatide pens are single-use only and come with the needle pre-attached and hidden. There is no dose dialing required. After removing the base cap, placing the pen against the skin, unlocking, and pressing the injection button, patients should hold the pen in place until the injection is complete (indicated by a click and/or the window turning completely colored). The entire pen should be discarded after a single use in an FDA-cleared sharps container—never recapping or reusing pens.
Storage and handling requirements include keeping unused pens refrigerated at 36°F to 46°F (2°C to 8°C) and protecting them from light. Pens may be stored at room temperature (up to 86°F or 30°C) for up to 21 days. Patients should never freeze tirzepatide or use medication that has been frozen, appears cloudy, discolored, or contains particles. Additional important safety instructions include: never share pens between patients, do not mix tirzepatide with insulin, and administer as separate injections if both medications are prescribed. Proper training from healthcare providers ensures patients can self-administer safely and confidently.
While injection timing does not fundamentally alter tirzepatide's side effect profile, strategic scheduling may help patients better manage common adverse effects and maintain treatment adherence. Gastrointestinal symptoms—including nausea, vomiting, diarrhea, constipation, and abdominal discomfort—are the most frequently reported adverse effects, occurring in 20-30% of patients (varying by dose and population), particularly during dose escalation. These symptoms typically emerge following injection and may persist for several days.
Patients experiencing significant nausea may benefit from evening injections, allowing them to sleep through the period of peak medication absorption. However, this approach should be balanced against the potential for nighttime nausea to disrupt sleep quality. Regardless of injection time, evidence-based management strategies include eating smaller, more frequent meals; avoiding high-fat, spicy, or heavily seasoned foods; staying well-hydrated; and considering over-the-counter antiemetics after consulting with a healthcare provider. If nausea persists or worsens, dose reduction or temporary treatment interruption may be necessary.
Injection site reactions—such as redness, itching, or mild swelling—occur in approximately 2-3% of patients and are generally self-limiting. These reactions are unrelated to time of day but can be minimized through proper injection technique, site rotation, and ensuring medication reaches room temperature before administration. Patients should report severe or persistent injection site reactions, as these may indicate hypersensitivity or anaphylaxis requiring immediate medical attention.
Hypoglycemia risk is generally low with tirzepatide monotherapy but increases when combined with insulin or sulfonylureas. Patients on combination therapy should monitor blood glucose levels regularly and discuss potential dose reductions of insulin or sulfonylureas with their healthcare provider during tirzepatide initiation and dose escalation. Patients may prefer daytime injections when they can more readily recognize and treat hypoglycemic symptoms. Warning signs include shakiness, sweating, confusion, rapid heartbeat, and dizziness—requiring immediate consumption of fast-acting carbohydrates.
Patients should stop tirzepatide and seek immediate medical care if they experience severe, persistent abdominal pain (which may indicate pancreatitis), symptoms of gallbladder disease (right upper quadrant pain, fever, jaundice), persistent vomiting leading to dehydration (which may cause acute kidney injury), or signs of severe allergic reaction. Patients with diabetes should be monitored for diabetic retinopathy complications. Tirzepatide is not recommended during pregnancy and should be discontinued if pregnancy occurs.
No, tirzepatide can be administered at any time of day without affecting its effectiveness. The medication's long half-life of approximately five days ensures consistent therapeutic effects throughout the week regardless of injection time.
If you miss a dose, administer it as soon as possible within 4 days (96 hours) after the scheduled time. If more than 4 days have passed, skip the missed dose and resume your regular weekly schedule.
Yes, you can change your weekly injection day as long as at least 3 days (72 hours) have elapsed since your previous dose. This flexibility allows you to adjust your schedule to better fit your routine while maintaining therapeutic consistency.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.